![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
A 35-year-old man is admitted with systolic blood pressure (BP) of 60 mm Hg and a heart rate (HR) of 150 bpm following a gunshot wound to the liver (Fig. 1–1). What is the effect on the kidneys? (A) They tolerate satisfactorily ischemia of 3–4 hours duration. (B) They undergo further ischemia if hypothermia is present. (C)They can become damaged, even though urine output exceeds 1500 mL/d. (D)They are affected and cause an increased creatinine clearance. (E) They are prevented from further damage by a vasopressor. |
(C) High-output renal failure should be sus- pected if the BUN continues to rise with urine output >1000–1500 mL/d. It is associated with mild-to-moderate renal insufficiency; in comparison, severe renal injury results in olig- uric renal failure. The kidneys do not tolerate ischemia for more than 30–90 minutes. Hypo- thermia is protective. There is a decrease in cre- atinine clearance. Vasopressors aggravate the deleterious effects of shock. |
|
|
|
Twenty-four hours after colon resection, urine output in a 70-year-old man is 10 mL/h. Blood chemistry analysis reveals sodium, 138 mEq/L; potassium, 6 mEq/L; chloride, 100 mEq/L; bicar- bonate, 14 mEq/L. His metabolic abnormality is characterized by which of the following? (A) Abdominal distension (B) Peaked T waves (C) Narrow QRS complex (D) Cardiac arrest in systole (E)J wave or Osborne wave |
(B) Hyperkalemia can manifest by GI or cardiovascular signs. GI symptoms include nausea, vomiting, intestinal colic, and diarrhea. Abdominal distension as a result of paralytic ileus is due to hypokalemia. An ECG is useful to monitor potassium levels. Hyperkalemia is characterized by peaked T waves. ECG changes also include ST-segment depression, widened QRS complex, and heart block. Cardiac arrest occurs in diastole with increas- ing levels of potassium. Osborne (J) wave is seen in hypothermia. |
|
|

3. |
C) In hyperkalemia, all oral and intravenous potassium must be withheld. Sodium chloride worsens the metabolic acidosis. Sodium bicar- bonate intravenously is given to divert potas- sium intracellularly by causing alkalosis. Calcium gluconate (1 g [10 mLof 10% solu- tion]) is given to counteract the effect of potas- sium on the myocardium. The hypertonic glucose solution stimulates the synthesis of glycogen, which causes cellular uptake of potassium. Small amounts of insulin (1 U/5 g of glucose) is helpful. The usual recommen- ded dose is 100 mLof 50% glucose with 10 U of insulin. Calcitonin is used for treating hypercalcemia. Serum magnesium is also ele- vated in renal failure. |
|
|
|
A 55-year-old man with Crohn’s disease had undergone resection of small bowel and anas- tomosis. Ten days later, he is found to have bil- ious drainage of 1 L/d from the drains. He is started on total parenteral nutrition (TPN). Four days later, his arterial blood gases (ABGs) are pH, 7.25; PO2, 98 mm Hg; and PCO2, 40 mm Hg. His anion gap is 10. The most likely cause is which of the following? (A) Diabetic ketoacidosis (B) Renal failure (C) Hypovolemic shock (D) Small-bowel fistula (E) Uncompensated metabolic alkalosis |
(D) This patient has metabolic acidosis with normal anion gap. The normal value of anion gap is 10–15. Loss of bicarbonate (e.g., small- bowel fistula, pancreatic fistula, or diarrhea) and gain of chloride (e.g., administration of ammo- nium chloride or HCl and decreased excretion as in distal renal tubular acidosis) result in meta- bolic acidosis with normal anion gap. In con- trast, in acidosis due to increased production of an organic acid (e.g., ketoacids in diabetes, sulfur and phosphoric acid in renal failure, and lactic acid in shock), the anion gap is increased. |
|
|
|
A 55-year-old man sustains numerous injuries involving the abdomen and lower extremities. During the intra- and postoperative periods, he is resuscitated with 10 Lof Ringer’s lactate and 2 U of packed red blood cells (RBC). After initial improvement, he has severe dyspnea on the second postoperative day. The most useful initial diagnostic test is which of the following? (A) Electrocardiogram (B) Analysis of arterial blood gas (C)Insertion of a central venous line (D) Ventilation-perfusion scan (E) Computed tomography (CT) scan of abdomen
|
(B) The patient has acute respiratory distress syndrome (ARDS). Measurement of ABGs pro- vides initial evaluation of pulmonary function in terms of oxygenation and ventilation. ECG is valuable for diagnosing myocardial ischemia or cardiac arrhythmias. Ventilation perfusion scanning is used for diagnosing pulmonary embolism. Acentral venous line provides infor- mation regarding the volume status of the patient, which may be low to normal in ARDS. |
|
|
|
A20-year-old man involved in a car crash sus- tained severe injuries to the chest, abdomen, and lower extremities. He is intubated and requires increasing concentration of oxygen to maintain his PO2. The pathologic changes do which of the following? (A) They cause the alveolar capillary membrane to become more impermeable. (B) They most frequently occur after severe injuries. (C) They are associated with low compliance. (D) They show a characteristic localized pattern on x-ray. (E) They involve a decrease in dead-space ventilation.
|
(C) Increased airway resistance (stiff lung) may be noted early in shock lung. The alveo- lar capillary membrane becomes more per- meable. There is a leak of a high-protein fluid from the capillary to the interstitial tissues and then into the alveoli. This is commonly called ARDS. Sepsis syndrome is the most frequent cause of ARDS (39%), followed by aspiration, multiple transfusion, massive soft- tissue injury, multiple trauma, near drown- ing, fat embolism, DIC, and pancreatitis. ARDS is associated with ventilation–perfusion imbalance. In some areas of lung, there is ven- tilation with no perfusion, whereas, in other areas, nonventilated alveoli are being per- fused. The net result is decrease in functional residual capacity, shunting, and increased dead space ventilation. Chest x-ray reveals diffuse alveolar infiltration, and findings are normal in the initial stage. |
|
|
|
A24-year-old woman is scheduled for an elec- tive cholecystectomy. The best method of iden- tifying a potential bleeder is which of the following? (A) Platelet count (B) A complete history and physical examination (C) Bleeding time (D) Lee-White clotting time (E) Prothrombin time (PT)
|
(B) Ahistory of bleeding should alert the clini- cian to evaluate the underlying cause. The bleed- ing time is influenced by those factors affecting platelet and capillary integrity. Prolongation of the PT may be attributed to decreased absorption of fat-soluble vitamin K, liver impairment, or decrease in the blood components because of consumption. |
|
|
|
A24-year-old man who is admitted to the intensive care unit (ICU) following severe head injury develops seizures on the fourth day of hospitalization. His urine output is 500 mL over 24 hours, sodium is 115 mEq/L, and serum and urine osmolality are 250 and 800 mOsm, respectively. The metabolic abnormal- ity is due to which of the following? (A) Administration of D5W (5% dextrose in water) and 0.33 normal saline (B) Syndrome of inappropriate secretion of antidiuretic hormone (SIADH) (C) Decreased antidiuretic hormone (ADH) secretion (D) Nasogastric suction (E) Renal insufficiency
|
(B) Possible causes of this syndrome include head injury, central nervous system (CNS) dis- orders, neoplastic diseases, pulmonary dis- eases, drugs, and idiopathic. It results in impaired water excretion characterized by olig- uria, hyponatremia, significantly decreased serum osmolality, and increased urinary osmo- lality. Administration of a hypotonic solu- tion(D5/0.33 NS) would not result in decreased urine output. Decreased ADH secretion would result in an increased urine output as opposed to a decreased urine output. Naso-gastric suc- tion while it can result in a hypo-kalemia, hyponatremia is less likely. Renal insufficiency would likely result in a decreased urine osmolality. |
|
|
|
A40-year-old man who weighs 65 kg is being observed in the ICU. Twenty-four hours post- operatively, he develops convulsions. His serum sodium is 118 mEq/L. Appropriate management includes which of the following? (A) Administration of normal saline (0.9%) (B) Administration of hypertonic saline (3%) (C) Emergency hemodialysis (D) Administration of vasopressin (E) Administration of Lasix, 40 mg intravenously (IV)10. A30-year-old man who weighs 60 kg has the fol- lowing laboratory values: hemoglobin, 10 g/dL; serum sodium, 120 mEq/L; serum potassium, 4 mEq/L; serum chloride, 90 mEq/L; and serum CO2 content, 30 mEq/L. What is his sodium |
(B) Hyponatremia occurs because of overhydra- tion and/or inadequate sodium replacement. When serum sodium is <130 mEq/L, acute symptomatic hyponatremia is manifested by CNS symptoms due to increased intracranial pressure. Muscle twitching and increased tendon reflexes seen in moderate hyponatremia progress to convulsions, loss of reflexes, and hyperten- sion with severe hyponatremia. Oliguric renal failure may become irreversible if not immedi- ately treated. Mild asymptomatic hyponatremia is treated with fluid restrictions. In the presence of CNS symptoms, the patient should be given hypertonic saline. |
|
|
|
A30-year-old man who weighs 60 kg has the fol- lowing laboratory values: hemoglobin, 10 g/dL; serum sodium, 120 mEq/L; serum potassium, 4 mEq/L; serum chloride, 90 mEq/L; and serum CO2 content, 30 mEq/L. What is his sodium deficit approximately? (A) 20 mEq (B) 200 mEq (C) 400 mEq (D) 720 mEq (E) 120 mEq |
(D) Sodium deficit is estimated by multiplying the decrease in serum sodium times the total body water, which is 60% of body weight:(normal serum sodium − observed serum sodium) × 0.6 × (total body weight) = (140 − 120) × 0.6 × 60 = 720 mEqHalf of this amount should be administered over 12–18 hours. |
|
|
|
A65-year-old man has urine output of 10 mL/h following abdominal aortic aneurysmectomy. Acute tubular necrosis is suggested by the pres- ence of which of the following? (A)Urine osmolality of more than 500 mOsm/kg (B)Urine sodium of more than 40 mEq/L (C) Fractional excretion of sodium of <1% (D) Blood urea nitrogen (BUN)-to-serum creatinine ratio (SCR) of more than 20 (E) Urine-to-plasma creatinine ratio (PCR) of more than 40 |
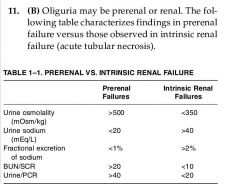
|
|
|
|
A30-year-old man with a history of Crohn’s dis- ease of the small bowel is admitted with ente- rocutaneous fistula. The daily output from the fistula is 2 L. The approximate composition of the fluids in mEq/Lis which of the following?Na K Cl HCO3 (A) 10 26 10 30 (B) 60 10 130 0 (C) 140 5 104 30 (D) 140 5 75 115 (E) 60 30 40 40 |
(C) The composition of various GI secretions is different. They are as follows: A, saliva; B, gas- tric; C, ileal; D, pancreatic; and E, colonic. The composition of intestinal fluid is the closest to that of plasma. |
|
|
|
A 70-year-old woman has a small-bowel fistula with output of 1.5 L/d. Replacement of daily losses should be handled using the fluid solution that has the following composition in mEq/L.Na K Cl HCO3 (A) 130 4 109 28 (B) 154 0 154 40 (C) 77 0 77 0 (D) 167 0 0 167 (E) 513 0 513 0 |
(A) The composition of small intestinal fluid is sodium, 140 mEq/L; potassium, 5 mEq/L; chlo- ride, 104 mEq/L; and bicarbonate, 30 mEq/L. Daily losses are best replaced by administra- tion of balanced salt solution (Ringer’s lactate) whose composition is depicted in A. B repre- sents normal saline (0.9%), C is half normal saline (0.45%), D is M/6 sodium lactate, and E is 3% sodium chloride. |
|
|
|
A 70-year-old man has undergone anterior resection for carcinoma of the rectum. He is extubated in the operating room (OR). In the recovery room, he is found to be restless with an HR of 136 bpm and a BP of 144/80 mm Hg. ABG analysis on room air reveals pH, 7.24; PCO2, 60 mm Hg; PO2, 54 mm Hg; HCO3, 25 mEq/L; and SaO2, 90%. The physiologic status can best be described as which of the following? (A) Respiratory alkalosis (B) Respiratory acidosis (C) Metabolic acidosis (D) Metabolic alkalosis (E) Combined respiratory and metabolic acidosis
|
(B) Adecrease in pH below 7.4 indicates acido- sis. PCO2 is increased over 40 mm Hg, suggest- ing respiratory acidosis. To differentiate pure from combined acidosis, pH is calculated based on changes in CO2. Achange of 10 mm Hg from 40 mm Hg changes pH by 0.08 from 7.4. In this case, there is a 20 mm Hg increase in PCO2, which would decrease pH by 2 × 0.08 = 0.16 from 7.4 or 7.24. The measured pH is 7.24. Therefore, the patient has pure respiratory acidosis. |
|
|
|
A 70-year-old man has undergone anterior resection for carcinoma of the rectum. He is extubated in the operating room (OR). In the recovery room, he is found to be restless with an HR of 136 bpm and a BP of 144/80 mm Hg. ABG analysis on room air reveals pH, 7.24; PCO2, 60 mm Hg; PO2, 54 mm Hg; HCO3, 25 mEq/L; and SaO2, 90%. Appropriate management for this patient should be which of the following? (A)To administer 40% oxygen by mask (B)Morphine, 2 mg IV (C)Ringer’s lactate, 250 mLover 1 hour (D) Intubation and ventilatory support (E) Deep breathing and coughing
|
(D) Respiratory acidosis in the immediate post- operative period is due to inadequate ventila- tion. Adequate ventilation needs to be restored by prompt intubation and ventilatory support. Use of morphine will further depress the respiration.
|
|
|
|
16. A60-year-old woman with mild hypertension is admitted for elective hysterectomy. On preoper- ative evaluation, she is found to have osteoarthri- tis; over the previous 6 months, she had noted watery diarrhea that was becoming progres- sively worse. The serum potassium is 3 mEq/L. Which is the most likely cause of hypokalemia? (A) Myoglobinemia (B) Villous adenoma of colon (C) High-output renal failure (D) Massive blood transfusion (E) Spironolactone (Aldactone) |
(B) Villous adenoma of colon can resultin watery diarrhea and hypokalemia. Massive tissue injury producing myoglobinemia is associated with significant release of intracellular potassium. Massive blood transfusion results in release of large amounts of potassium. The ability to excrete potassium is impaired in high-output renal failure. Spironolactone is a potassium- sparing diuretic. |
|
|
|
A 64-year-old man underwent major abdominal surgery to remove a ruptured aortic aneurysm. Four days after the operation, an attempt was made to wean him off the ventilator. ABG analysis reveals pH, 7.54; PCO2, 30 mm Hg; PO2, 110 mm Hg; HCO3, 30 mEq/L; and SaO2, 99%.17. Blood gas analysis reveals which of the following? (A) Respiratory acidosis (B) Metabolic alkalosis (C) Respiratory alkalosis (D) Compensated respiratory acidosis (E) Combined respiratory and metabolic alkalosis
|
(E) Achange in PCO2 of 10 mm Hg from the normal value of 40 mm Hg produces a 0.08 change in pH (from 7.4). APCO2 of 30 mm Hg, representing a decrease of 10 mm Hg, can account for an increase in pH by 0.08 (i.e., 7.4–7.48). The patient’s measured pH is 7.54. The additional increase in pH is due to meta- bolic alkalosis.
|
|
|
|
A 64-year-old man underwent major abdominal surgery to remove a ruptured aortic aneurysm. Four days after the operation, an attempt was made to wean him off the ventilator. ABG analysis reveals pH, 7.54; PCO2, 30 mm Hg; PO2, 110 mm Hg; HCO3, 30 mEq/L; and SaO2, 99%. What will be the most likely complication due to the metabolic changes experienced by the patient? (A) Hypokalemia (B) Shift of oxyhemoglobin dissociation to the right (C) Hyperkalemia (D) Hypercalcemia (E) Hyperchloremia
|
(A) Alkalosis is associated with hypokalemia. Hypokalemia can be sudden and severe. It is related to (a) intracellular shift of potassium in exchange for hydrogen and (b) excessive uri- nary potassium loss. The oxyhemoglobin dis- sociation curve is shifted to left, and a decrease in levels of ionized calcium can result in tetany and convulsions.
|
|
|
|
A42-year-old man with small-bowel fistula has been receiving TPN with standard hypertonic glucose-amino acid solution for 3 weeks. The patient is noticed to have scaly, hyperpigmented lesions over the acral surfaces of elbows and knees, similar to enterohepatic acrodermatitis. What is the most likely cause of the condition? (A) Copper deficiency (B) Essential fatty acid deficiency (C) Excess glucose calories (D) Hypomagnesemia (E) Zinc deficiency
|
(E) Zinc is one of the metalloenzymes involved in lipid, carbohydrate, protein, and nucleic acid metabolism. Skin lesions similar to enterohep- atic acrodermatitis are the most common sign seen in zinc deficiency. Other manifestations include hypogonadism, diminished wound healing, and immunodeficiencies. Copper defi- ciency is characterized by microcytic hypo- chromic anemia. |
|
|
|
Questions 20 through 22A27-year-old man is involved in a car crash while traveling in excess of 70 mi/h. He sustains an intra- abdominal injury and a fracture of the femur. The BP is 60/40 mm Hg, and the hematocrit is 16%.20. Which physiologic changes will ensue? (A) Peripheral vasodilation (B) Inhibition of sympathetic tone (C) Temperature rise to 103.8°F (D) Eosinophilia (E) Lactic acidosis |
(E) The fall in pressure will signal changes via baroreceptors located in the arch of the aorta and carotid sinus and will cause sympathetic stimulation with tachycardia, peripheral vaso- constriction, and hypothermia. Eosinopenia rather than eosinophilia is more likely to be present. There is a switch from aerobic to anaer- obic metabolism. Lactic acid accumulation indi- cates an adverse prognosis in shock. There is a progressive deterioration in prognosis as the blood lactate level increases from 1 to above 3 mm/L. |
|
|
|
There is likely to be a proportionately greater increase in blood flow to which of the following? (A) Kidneys (B) Liver (C) Heart (D) Skin (E) Thyroid gland
|
(C) The fall in cardiac output results in a rela- tively larger proportion of blood to be distrib- uted to the heart. The changes are mediated mainly by sympathetic stimulation. There is increased arteriolar and precapillary sphincter tone in the skin and in the renal and splanchnic circulation. In the heart, coronary artery vasodi- lation occurs, which is brought about partly by local release of vasodilator substances (due to hypoxemia and acidosis). |
|
|
|
Initial resuscitation is best done by adminis- tration of which of the following? (A) D5W (B) D5W and 0.45% normal saline (C) Ringer’s lactate solution (D) 5% plasma protein solution(E) 5% hydroxyethyl starch solution
|
(C) Initial resuscitation of a trauma patient is best done by administering Ringer’s lactate, because it is isotonic, and it is similar to plasma in electrolyte composition. There is no conclu- sive evidence that colloid solutions (albumin, plasma protein solution, or hydroxyethyl starch solution) improve the rate of resuscitation or eventual outcome. D5W and D5W and 0.45% normal saline are hypotonic. Use of crystalloid solutions also aids in the resuscitation of the interstitial compartment. |
|
|
|
A30-year-old man is brought to the emergency department following a high-speed car accident. He was the driver, and the windshield of the car was broken. On examination, he is alert, awake, oriented, and in no respiratory distress. He is unable to move any of his four extremities; how- ever, his extremities are warm and pink. His vital signs on admission are HR 54 bpm and BP 70/40 mm Hg. What is the diagnosis? (A) Hemorrhagic shock (B) Cardiogenic shock (C) Neurogenic shock (D) Septic shock (E) Irreversible shock
|
(C) Neurogenic shock (not to be confused with spinal shock, which is defined by loss of reflexes below the area of spinal cord injury, a neurologic phenomena) is secondary to high spinal cord injury as evidenced by inability to move all four extremities. Neurogenic shock is clinically man- ifested by warm skin, bradycardia, and hypoten- sion. In septic shock, while the skin is warm, the patient usually has tachycardia. In all other types of shock, the skin is cold. Treatment consists of volume replacement with balanced salt solution (lactated Ringer’s solution). On rare occasions, some patients may need vasoconstrictors (e.g., phenylephrine hydrochloride). |
|
|
|
A48-year-old man with severe vomiting as a result of gastric outlet obstruction is admitted to the hospital. There is marked dehydration, with urine output 20 mL/h, and the hematocrit is 48%. Clinical confirmation of pyloric obstruction is most readily established by which of the following? (A) Observation of peristalsis from left to right (B) Observation of peristalsis from right to left (C) Percussion of the upper abdomen (D) Succussion splash (E) Auscultation of the upper left abdomen
|
(D) Succussion splash is elicited by placing one hand behind and the other in front of the left abdomen and rib cage and rocking the patient gently between the two hands. In pyloric obstruction, one can feel the fluid hitting the fingers (succussion). Peristalsis is likely to be observed in infants with congenital pyloric stenosis.
|
|
|
|
A48-year-old man with severe vomiting as a result of gastric outlet obstruction is admitted to the hospital. There is marked dehydration, with urine output 20 mL/h, and the hematocrit is 48%. What isthe predominantmetabolic abnormality? (A) Aspiration pneumonia with respiratory alkalosis (B) Hypochloremic alkalosis (C) Salt-losing enteropathy (D) Intrinsic renal disease (E) Metabolic acidosis
|
(B) Duodenal ulcer and gastric carcinoma are the most likely causes of pyloric obstruction in adults. Metabolic alkalosis results from loss of fixed acids from the stomach. The bicarbonate content of the blood accompanies the elevation in pH. In severe metabolic alkalosis, paradoxical loss of acid (hydrogen) in the urine occurs in an attempt to conserve potassium. Hypokalemia worsens the metabolic consequences of meta- bolic alkalosis.
|
26.(D) Potassium should not be given initially until moderate hydration has been achieved, and urine flow is adequate. Normal saline is required initially to correct the hypochloremia.
|
|
|
A48-year-old man with severe vomiting as a result of gastric outlet obstruction is admitted to the hospital. There is marked dehydration, with urine output 20 mL/h, and the hematocrit is 48%. Initial treatment for this patient should include which of the following? (A) Administration of 10% dextrose (D10W) in one-third saline solution IV (B) Antiemetic (C) Hemodialysis to correct azotemia (D) Saline fluid replacement with appropriate potassium administration (E) Ringer’s lactate solution
|
(D) Potassium should not be given initially until moderate hydration has been achieved, and urine flow is adequate. Normal saline is required initially to correct the hypochloremia. |
|
|
|
A48-year-old man with severe vomiting as a result of gastric outlet obstruction is admitted to the hospital. There is marked dehydration, with urine output 20 mL/h, and the hematocrit is 48%. Severe hypochloremic metabolic alkalosis fails to respond to standard therapy. His metabolic abnormality can be corrected by infusing which of the following? (A) Normal saline (B) Ringer’s lactate solution (C) Hypertonic saline (D) 0.1 N hydrochloric acid (E) 1 N hydrochloric acid
|
(D) Initial management of hypochloremic meta- bolic alkalosis includes administration of isotonic sodium chloride solution with replacement of potassium chloride. Inpatients refractory to stan- dard therapy use of O.1 N and 0.2 N hydrochlo- ric acid has been shown to be safe and effective therapy. Ammonium chloride solution has also been used, but this can lead to ammonia toxicity, especially in patients with hepatic insufficiency.
|
|
|
|
A48-year-old man with severe vomiting as a result of gastric outlet obstruction is admitted to the hospital. There is marked dehydration, with urine output 20 mL/h, and the hematocrit is 48%. In the absence of malignancy, further treatment after appropriate resuscitation should include which of the following?Questions: 17–31 5 (A) Jejunostomy feeding (B) Vagotomy and drainage (C) Steroids (D)No foods given orally (PO) for 6 weeks (E) Pyloromyotomy alone
|
.(B) The actual surgical treatment for obstruc- tion caused by peptic ulcer is controversial. Appropriate gastric surgery with drainage usu- ally is required if pyloric stenosis is severe. Drainage procedures include pyloroplasty, gas- trojejunostomy, or antrectomy. An alternative to vagotomy and drainage would be vagotomy, antrectomy with gastrojejunostomy, or a Billroth II subtotal gastrectomy with gastrojejunal anas- tomosis. It is important to be certain that a gas- tric carcinoma is not the cause of the pyloric outlet obstruction.
|
|
|
|
Questions 29 through 31During cholecystectomy in a 67-year-old woman, there is severe bleeding from accidental injury to the hepatic artery. The patient requires transfusion of 2000 mLof blood. After the operation, 24-hour urine output varies between 1250 and 2700 mL/d. She was adequately hydrated, but BUN levels continue to rise 10–12 mg daily over a 5-day period.What is the main finding? (A) Progressive bleeding (B) High-output renal failure (C) Postcholecystectomy syndrome (D) Glomerulonephritis (E) Obstructive jaundice
|
(B) The presence of an adequate urine output does not preclude a diagnosis of high-outputrenal failure. The mechanism is based in part on prior ischemia to the nephron structure of the kidneys. There may be an initial period of olig- uria. Urea, potassium, and acids are still partly excreted in the urine, and lactate or bicarbonate is given to avoid development of acidosis.
|
|
|
|
During cholecystectomy in a 67-year-old woman, there is severe bleeding from accidental injury to the hepatic artery. The patient requires transfusion of 2000 mLof blood. After the operation, 24-hour urine output varies between 1250 and 2700 mL/d. She was adequately hydrated, but BUN levels continue to rise 10–12 mg daily over a 5-day period.Metabolic changes likely to occur include which of the following? (A) Hyperkalemia (B) Hyponatremia (C) Hypophosphatemia (D) Metabolic alkalosis (E) Hypomagnesemia
|
(A) Potassium should not be given, and potas- sium levels must be monitored carefully to avoid hyperkalemia. Phosphorous and mag- nesium levels may be increased, and hyperna- tremia is likely to occur when fluid is restricted and a solute-poor urine is excreted. Autopsy in patients dying early shows that the distal nephron is affected more than the proximal nephron. Although mortality figures are high, if the patient survives the postoperative period, satisfactory renal function can be anticipated.
|
|
|
|
During cholecystectomy in a 67-year-old woman, there is severe bleeding from accidental injury to the hepatic artery. The patient requires transfusion of 2000 mLof blood. After the operation, 24-hour urine output varies between 1250 and 2700 mL/d. She was adequately hydrated, but BUN levels continue to rise 10–12 mg daily over a 5-day period. Management includes which of the following? (A)Restriction of fluids to 750 mL/d (B)8 Lof fluid daily to remove urea (C) Replacement of fluid loss plus insensible loss (D)80 mEq potassium chloride (KCl) per 12 hour (E) Ammonium chloride IV |
(C) Marked fluid restriction may result in hypernatremia. If the condition is treated appro- priately, urea nitrogen usually falls after 1 or 2 weeks. In elderly and cardiac patients, pul- monary edema occurs more readily, and diuret- ics may be contraindicated because azotemia may be made more severe. Ammonium chlo- ride would make the acidosis worse. Potassium has to be monitored carefully, because severe hyperkalemia is readily induced.
|
|
|
|
Questions 32 and 33A14-year-old boy with a known bleeding tendency since infancy has severe epistaxis. Examination reveals an equinus contracture of the right leg and a large hemarthrosis.32. What is the most likely diagnosis? (A) Diethylstilbestrol (DES) was taken by the mother during pregnancy (B) Aplastic anemia (C) Henoch-Schönlein purpura (D) Hemophilia (E) Wilson’s disease with cirrhosis
|
(D) Hemophilia (factor VIII deficiency) usually occurs during infancy. It is sex-linked, recessive, and affects males almost exclusively. DES administered during the mother’s pregnancy has not been incriminated in coagulation disor- ders but is associated with vaginal carcinoma in adolescent girls. Henoch-Schönlein purpura usually occurs about 3 weeks after a streptococ- cal infection and includes joint pain, purpura, and nephritis. Wilson’s disease is associated with a disturbance in copper metabolism. |
|
|
|
Questions 32 and 33A14-year-old boy with a known bleeding tendency since infancy has severe epistaxis. Examination reveals an equinus contracture of the right leg and a large hemarthrosis. Treatment should include which of the following? (A) Penicillamine (B)Transfusion of factor VIII to 30% of normal factor levels (C)Transfusion of factor VIII to 10% of normal factor levels (D) Platelet transfusion (E) Exploration of joint
|
(B) Spontaneous bleeding occurs when factor VIII is reduced below 2–3%. Once serious bleeding occurs, a higher factor VIII activity— probably approaching 30%—is required for adequate hemostasis. The half-life of factor VIII is 8–12 hours. In minor lesions, 10 U/kg body weight of factor VIII is administered. For severe lesions, the dosage is 40–50 U/kg body weight |
|
|
|
A 10-year-old boy with history of prolonged bleeding after minor injury is scheduled for ton- sillectomy. The bleeding time, PT, and fibrinogen are normal. What would be the most helpful investigation? (A) Fibrinolysis (euglobulin clot lysis time) (B) Platelet count (C) Thrombin time (D) Partial thromboplastin time (PTT) (E) Factor VII assay
|
(D) The clinical picture is suggestive of hemo- philia. The normal bleeding time excludes cap- illary fragility or platelet deficiency. If fibrinolysis was evident, the fibrinogen level would be reduced. In the presence of a normal PT, a pro- longed PTT indicates a deficiency of factor VIII, IX, XI, or XII. The PT evaluates the extrinsic coagulation pathway. The normal PT excludes factor VII deficiency. The thrombin time eval- uates fibrinogen to fibrin conversion with an external source of thrombin and will be normal as fibrinogen levels are normal. |
|
|
|
Questions 35 to 37A22-year-old man is brought into the emergency department in profound shock after a fall from the fourth floor of a building. After resuscitation, small- bowel resection and hepatic segmentectomy are performed at laparotomy. He receives 15 U of packed RBCs, 4 U of fresh-frozen plasma, and 8 L of Ringer’s lactate. On closure, diffuse oozing of blood is noted.35. What is the most likely cause? (A) Hepatic failure (B) Hypersplenism (C) Platelet deficiency (D) Factor IX (Christmas factor) deficiency (E) Congenital hypoprothrombinemia
|
(C) Thrombocytopenia is the major hemostatic disorder in massive blood transfusion. Platelet transfusion usually is indicated when more than 6–8 U of blood is transfused rapidly. There is the risk of causing hepatitis. Stored blood is defi- cient in factors V and VIII; as such, PT and PTT may be slightly prolonged after massive blood transfusion. Fresh-frozen plasma is the source of factors V and VII, which would be deficient in banked blood. Unless there is previous liver cir- rhosis, the procedures enumerated are unlikely to lead to liver failure. Hypersplenism occurs in patients with enlarged spleens. |
|
|
|
Which test is most likely to be helpful in man- agement of patient? (A) Platelet count (B this ) Bone marrow biopsy (C) Liver-spleen scan (D) Factor VIII assay (E) Smear for Howell-Jolly bodies
|
(A) Platelet deficiency is likely to be evident, but tests to exclude other causes of bleeding are indicated. The possibility of defibrinogenation, intravascular coagulopathy, or fibrinolysis must be excluded by appropriate coagulation studies. Bleeding from a vein or artery, incom- patible blood transfusion, DIC, acidosis, and hypothermia are other considerations to explain any unusual bleeding after a major surgical procedure. |
|
|
|
Bleeding persists despite all appropriate blood coagulant replacement, and laparotomy reveals multiple sites of bleeding from the liver and the rest of the abdomen. Treatment should include which of the following? (A) Hepatic artery ligation (B) Packing with laparotomy towels (C) Immediate closure (D) A large dose of heparin (E)Solu-Medrol, 1 g IV
|
(B) In desperate cases where bleeding persists despite all other measures, packing the abdomen with laparotomy packs may offer temporary control. The patient is taken to the OR 24–48 hours later for removal of packing after stabi- lization of hemodynamic status and correction of coagulopathy.Answers: 24–41 21 |
|
|
|
38. A50-year-old suffering from chronic alcoholism isadmittedto the hospital. He hasmuscletremors and hyperactive tendon reflexes. Serum mag- nesium is 1.8 mEq/L (normal 1.5–2.5 mEq/L). Concerning magnesium, which of the follow- ing statements is true? (A) It is mainly extracellular (B) Excess may cause a positive Chvostek’s sign (carpopedal spasm) (C) Deficiency is treated with parenteral bicarbonate (D)Symptoms are due to deficiency of magnesium (E)It may become elevated in acute pancreatitisQuestions 39 and 40
|
(D) Symptoms are due to magnesium deficiency. Magnesium is mainly intracellular. Magnesium deficiency occurs in the presence of starvation, malabsorption syndrome, acute pancreatitis, and chronic alcoholism. Symptoms are charac- terized by neuromuscular and CNS hyperactiv- ity, such as muscle tremors, hyperactive tendon reflexes, and tetany with a positive Chvostek sign. The syndrome of magnesium deficiency can exist in the presence of normal serum mag- nesium levels. Magnesium deficiency is treated with parenteral magnesium sulfate or magne- sium chloride. |
|
|
|
A 30-year-old man with multiple injuries has severe renal insufficiency. On the third day of hospitalization, he is lethargic with generalized weakness and decreased deep tendon reflexes. An electrocardio- gram (ECG) reveals a widened QRS complex with elevated T waves. What is the most likely cause of the patient’s condition? (A) Hypokalemia (B) Hyponatremia (C) Hypermagnesemia (D) Hypocalcemia (E) Hypophosphatemia |
(C) Symptomatic hypermagnesemia is seen after early thermal injury, massive trauma, surgical stress, and in the presence of severe renal insufficiency. ECG changes resemble those seen with hyperkalemia. Hypokalemia and hypophosphatemia can cause symptoms of generalized weakness, but potassium and phosphorus are increased in renal failure. Hypokalemia is characterized by flattening of T waves and U waves. Hypocalcemia is characterized by hyperactive tendon reflexes. Hyponatremia is characterized by nervous irri- tation as restlessness and convulsions with no specific ECG changes.
|
|
|
|
A 30-year-old man with multiple injuries has severe renal insufficiency. On the third day of hospitalization, he is lethargic with generalized weakness and decreased deep tendon reflexes. An electrocardio- gram (ECG) reveals a widened QRS complex with elevated T waves.What should be the immediate management of the patient? (A) Administration of potassium chloride (B) Administration of calcium chloride (C) Restriction of fluid intake (D) Use of Kayexylate enemas (E) Administration of hypertonic saline
|
(B) Administer calcium chloride. Management of hypermagnesemia involves correction of extracellular volume deficit and acidosis and withholding exogenous magnesium. Calcium chloride should be administered to reverse the ECG changes temporarily. Peritoneal dialysis or hemodialysis is necessary for persistent symptoms or toxicity. Calcium chloride stabi- lizes the cardiac cell membrane and thereby reduces the risk of dysrhythmias.
|
|
|
|
A45-year-old male with a known history of alcoholism is admitted with acute pancreatitis. His serum calcium is 7 mg/dL. Management is based upon which of the following?(A)One-fourth of calcium in serum is ionize (B) Alkalosis increases the ionized calcium component (C) Hypocalcemia may cause polyuria and polydypsia(D) Determination of serum albumin is necessary (E) Treatment should involve intravenous administration of calcium chloride
|
(D) Determination of serum albumin or protein level is necessary for proper determination of serum calcium level. For every 1 g decrease of serum albumin, the serum calcium level is cor- rected by 0.8. Intravenous administration of calcium chloride is indicated in the presence of symptoms. Approximately 45% of serum cal- cium is ionized and responsible for neuromus- cular stability. Half of the calcium in the blood is bound to protein, and an additional 5% is attached to substances other than protein. Alkalosis decreases the ionized component. Hypercalcemia causes polydypsia and polyuria. |
|
|
|
A 36-year-old diabetic woman develops meta- bolic changes following salpingo-oophorectomy. Serum osmolality of the blood can be calculated from serum values of which of the following? (A) Sodium, potassium, chloride, and bicarbonate (B) Sodium, potassium, urea, and hemoglobin (C) Sodium, potassium, glucose, and urea (D) Sodium, albumin, urea, and glucose (E) Sodium, potassium, albumin, and glucose
|
(C) Serum osmolality is calculated from serum values of sodium, potassium, glucose, and BUN by using the formula 2 (Na + K) + BUN/2.8 + glucose/18. |
|
|
|
Questions: 32–46 743. In a 12-year-old boy who sustained severe head injury caused by a fall from the third floor of a building, the syndrome of diabetes insipidus is characterized by which of the following? (A) Low serum sodium (B) High urinary specific gravity or osmolality (C) High serum osmolality (D) Low urine output (E) Expanded extracellular fluid volume
|
(C) Injury to the pituitary stalk in major skull fractures involving the base of the skull can result in decreased secretion of vasopressin (ADH). There is increased urine output that is diluted (osmolality <270 mOsm/kg). The extracellular fluid volume is contracted, resulting in high serum osmolality (>300 mOsm/kg)andincreased serum sodium.
|
|
|
|
In a 40-year-old woman receiving TPN for small-bowel fistula, what finding can be attrib- uted to hypophosphatemia? (A) Increased cardiac output (B) Diarrhea (C) Increased energy production (D) Rhabdomyolysis (E) Increased white blood cells (WBC) function
|
(D) Hypophosphatemia results in decreased syn- thesis of phosphorylated intermediate metabo- lites such as adenosine triphosphate (ATP), 2, 3-DPG, and cyclic adenosine monophosphate (cAMP). Deficiency can result in erythrocyte membrane instability, WBC dysfunction, platelet dysfunction, congestive heart failure, arrhyth- mias, weakening of respiration muscles, hemol- ysis, and rhabdomyolysis. |
|
|
|
Questions 45 and 46A 60-year-old woman who underwent a mastectomy for breast cancer 2 years earlier presents to the emer- gency department with headache, backache, and fre- quent vomiting. She is extremely thirsty and stuporous.45. Which test is most likely to identify the cause? (A)CT scan of the head (B) X-ray of spine (C) Serum sodium determination (D) Serum calcium determination (E) Serum glucose determination
|
(D) The symptoms are suggestive of hypercal- cemia. Major causes of hypercalcemia are cancer with bony metastasis and hyperparathyroidism. Symptoms involve the GI, renal, musculoskele- tal, and CNS. |
|
|
|
What should be the initial management of the patient? (A) Restrict fluid intake (B) Normal saline infusion (C) D5W infusion (D) Thiazide (E) Hemodialysis |
(B) Patients with hypercalcemia have decreased extracellular fluid volume due to vomiting and polyuria. Vigorous resuscitation with salt solu- tion will lower the serum calcium by dilution and increased renal excretion. Furosemide and not thiazides increase renal excretion of calcium. Additional therapy includes administration of oral or intravenous inorganic phosphates, corti- costeroid, mithramycin, and calcitonin. |
|
|
|
A40-year-old man is found to have severe metabolic acidosis with a high anion gap. What is the most likely cause? (A) Diarrhea (B) Methanol ingestion (C) Proximal renal tubular acidosis (D) Distal renal tubular acidosis (E) Ureterosigmoidostomy
|
(B) Methanol ingestion results in increased pro- duction of lactic acid causing an increased anion gap. The other conditions listed are associated with normal anion gap. Diarrhea, proximal renal tubular acidosis, and ureterosigmoidostomy result in loss of bicarbonate, while distal renaltubular acidosis is associated with decreased acid excretion. |
|
|
|
Following surgery for a perforated appendix with generalized peritonitis and multiple intra- abdominal abscess, a 25-year-old man is admit- ted to the ICU. On the third postoperative day, he continues to be febrile and has a nasogastric tube. What is the metabolic characteristic seen in him? (A) A decrease in energy expenditure (B)Fat as his primary fuel (C) Respiratory quotient of 0.6–0.7 (D) Proteolysis (E) Decreased hepatic synthesis of protein
|
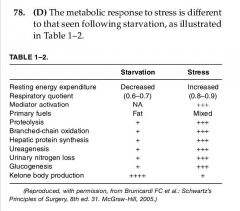
|
|
|
|
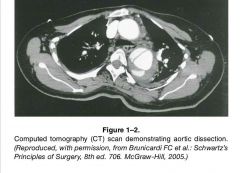
You are asked to see a 70-year-old male admitted to the ICU with anterior chest pain radiating to the back described as “a tearing sensation.” The pain reached maximum intensity within 30 min- utes. The patient has a history of hypertension (noncompliant with medications). His BP in the ICU is 170/110 mm Hg, HR =110/min. Physical examination reveals a 2/6 diastolic murmur and unequal femoral pulses. ACXR of this patient was normal and the CT chest, which was obtained, is shown in Fig. 1–2. Which of the fol- lowing statements regarding his treatment and prognosis are correct? (A) The patient will require nitroprusside and beta blockade, but will not require surgical intervention. (B) The patient will require only nitroprusside but will not require surgical intervention. (C) The patient will require nitroprusside and b-blockade prior to emergency surgical intervention. (D) Neither nitroprusside nor b-blockade is required prior to surgical intervention. (E) Nitroprusside and b-blockade are required initially, but surgery may be done electively within 4–6 weeks. |
(C) The patient has a diagnosis of dissecting aortic aneurysm. This requires emergent med- ical as well as surgical intervention. The BP needs to be lowered by using nitroprusside as well as a b-blocker to reduce dp/dt (the force with which the heart is pumping). Once BPis controlled the surgical intervention is needed to correct the problem. |
|
|
|
The type of thyroid cancer with the worst prognosis (5–yearsurvival <1%) is:
|
anaplastic thyroidcancer
|
|

