![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
Premonitory (Prodromal) Signs of Labor
1.Lightening 2.Braxton Hicks Contractions 3.Cervical changes "ripening" changes "ripening" 4.Bloody show |
1.Lightening
•When the fetus’s presenting part descends in the TRUE pelvis, this settling is called Lightning or “dropping” Resulting symptoms: - Breathe easier - Urinary frequency - Leg Cramps - Edema of Lower extremities - Increase vaginal secretions 2.Braxton Hicks Contractions •Irregular, intermitting, painless, contractions Promote oxygen (placenta circulation) to the fetus 3. Cervical changes "ripening" - Softening (cervix like butter, softer than Goodell Sign) - Effacement - Occasional dilation of the cervix to 1 or 2 cm 4.Bloody show With softening and effacement of the cervix, the mucous plug is often expelled. Results in a small amount of blood loss from exposed cervical capillaries --> Pink tinged secretions. |
|
|
Premonitory (Prodromal) Signs of Labor
5.GI symptoms 6.Rupture of membranes 7.Nesting behaviors 8.Other premonitory symptoms |
5.GI symptoms - just prior to the onset on labor:
- Mild diarrhea - Indigestion - Nausea/vomiting 6. Rupture of membranes Amniotic membranes rupture before the onset of labor in @ 12% of women. 80% of these women will have spontaneous labor in 24 hours. 7.Nesting behaviors - Sudden burst of energy. Occurs @ 24-48 hours before labor. Nurses need to caution prospective mothers not to overexert themselves during this energy burst. (warn patient to conserve energy until labor) 8.Other premonitory symptoms a.Weight loss of 0.5 - 1.5 Kg (1.1 – 3.3 lbs). (^estrogen& drop progesterone) b.Increased backache and sacroiliac pressure. (because relaxin on pelvic joint) |
|
|
STAGES OF LABOR
First Stage of Labor "Stage of Dilatation": Latent or Early Phase |
Begins with the onset of regular uterine labor contractions and ends with the complete dilatation of the cervix.
Subdivided into Phases: 1. Latent or Early Phase •Uterine contractions (cxs) become established. •Up to 3 cms dilated. •Cxs usually mild. •Women often talkative, eager to answer questions. •Cxs increase in frequency, duration, & intensity. oStart as mild cxs, lasting 15-20 seconds duration, with frequency of 10-20 minutes. ------->Progress to moderate intensity cxs (50 -> 60 mm Hg), Duration of 30-40 seconds, Frequency of 5-7 minutes. Length of the latent phase < 1 hour --> many hours nulliparous: 8.6 Multiparous: 5.3 |
|
|
First Stage of Labor "Stage of Dilatation": Active Phase
|
2. Active Phase - 4 --> 7 cms dilated.
•Uterine cxs increase in intensity - moderate -strong (50 – 70 mm Hg). •Increase in duration (40-60 seconds). •Increase in frequency (q 3-5 minutes). •Effacement complete. •Dilation should be 1.2 cm/hr in nullipara and @1.5 cm/hr in multiparas. •Bloody show increases. •Fatigue evident. •Apprehension increases as cxs become stronger and more frequent. •More serious and introverted. •Focused on breathing and relaxation. •Fetal descent is progressive. |
|
|
First Stage of Labor "Stage of Dilatation":
Transition Phase |
3.Transition Phase
•Cervix dilates 8 --> 10 cms. •Cxs: Frequency 1 1/2 - 2 minutes. oDuration 60 - 90 seconds. oIntensity - strong (> 75 mm Hg). •Bloody show heavy. •Intact membranes often rupture. •Rate of fetal descent increases: oAt least 1 cm/hr in nullipara and 2 cm/hr in multiparas. •Characteristics of this phase: Restlessness Frequent position changes Profuse diaphoresis Leg cramps Nausea/Vomiting, hiccupping, belching Hyperventilation-^breathe rate Inner directed Tired Difficulty understanding directions Request medications Angry about cxs. Anxious to get it over with Increasing rectal pressure -> urge to defecate. •Transition phase should not be longer that 3 hrs for nullipara or 1 hour for multipara. Average length of First Stage:@13 hrs for nulliparas and shorter for multiparas (7 hrs 20 min average). |
|
|
SECOND STAGE OF LABOR "Stage of Expulsion"
|
•Begins with complete dilation and ends with the birth of the baby.
•Average length nullipara 1-3 hrs and multipara 15 minutes to 1 hour. •Cxs continue like transition phase. •Latent phase(laboring down)– period of rest, while fetus passively descends. •As fetal head descends --> urge to push “Ferguson’s reflex”. •Active phase – active pushing phase oAs women pushes, intra-abdominal pressure is exerted from cxs of maternal abd muscles. oWomen often feel relieved - feel a sense of control with pushing (less pain). |
|
|
THIRD STAGE OF LABOR "Placental Stage":
1. Placenta Separation |
THIRD STAGE OF LABOR "Placental Stage"
Begins with delivery of the baby and ends with delivery of the placenta. Two Phases of the third stage of labor: 1. Placenta Separation After the baby is born, the uterus contracts firmly - -> Diminishes uterine capacity and surface area of placental attachment. Placenta begins to separate. Signs of placental separation - A globular shaped uterus. - A rise of the fundus in the abd. - A sudden gush or trickle of blood. - Further protrusion of the umbilical cord out of the vagina. |
|
|
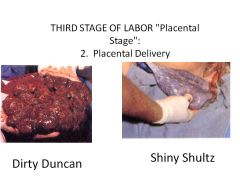
2. Placental Delivery
When signs of placental separation appear --> Women asked to bear down to aid in placenta expulsion. Fetal side presenting - "Shiny Schultz" Maternal side presenting - "Dirty Duncan". |
|
|
FOURTH STAGE OF LABOR
|
Physiologic readjustment period of the mother's body.
(going back to pre-pregnancy) Lasts 1 - 4 hours after delivery. |
|
|
NURSING CARE OF THE LABOR CLIENT:(Objective) ASSESSMENT
|
ASSESSMENT
•Subjective information obtained: oDemographic information: Name, age oAttending physician or midwife oSupport people oBlood type and Rh oResults of serology testing, HIV testing oRubella titer oWeight: Prepregnant and current oAllergies oDrug and alcohol consumption oHx of previous illnesses oPregnancy data: Gr, Para, F P A L, EDC Descriptions of previous labor and delivery Problems during prenatal course oMethod of Infant feeding oPrepared childbirth classes? Type? oRequests regarding labor and delivery oHx of special tests oHx of Preterm labor requiring tocolytic therapy oPediatrician oNutrition, Hydration & Sleep. First must determine if client is in labor True labor or false labor? Assess contractions Frequency Duration Intensity |
|
|
NURSING CARE OF THE LABOR CLIENT:(Subjective) ASSESSMENT
|
Subjective Assessment:
"How often do the cxs occur?" "How long do the cxs last?" "What is the level of pain?" "What was the time of the first cx?" "At what time did the cxs become regular?" "Do the cxs become more or less frequent with walking?" |
|
|
NURSING CARE OF THE LABOR CLIENT:(Objective 2) ASSESSMENT
|
Objective Assessment:
•Assess cxs by placing your fingertips on the uterine fundus. oAs cx begins, you will feel a tightening or hardening of the fundus. oThis tightening increases to a hard, board-like consistency at the acme (peak) of the cx. oThen gradually diminishes as the cx goes down. •At least three successive cxs should be assessed to provide enough data to determine the contraction pattern. •Frequency recorded in minutes. •Duration recorded in seconds. •Nurse also needs to assess intensity cxs by palpation. oMild cx: Fundus easily indentable. (chin-->soft tissue) oModerate cx: Fundus slightly indentable. (nose-->cartilage) oStrong cx: Unable to indent fundus.(forehead-->bone) |
|
NURSING CARE OF THE LABOR CLIENT:
|
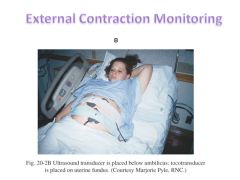
External Tocotransducer "TOCO"
•A flat disk with a pressure sensitive button. Placed on the area of greatest contractility. As the uterus cxs, pressure is exerted against the toco button. ----> Transmitted to the monitor and recorded on graph paper. •Uterine cxs can be assessed for frequency and duration. •External monitor does not accurately reflect intensity of cxs. oBut still recorded on graph paper. oNurse needs to continue to assess intensity by palpation. •Factors affecting monitoring: - Obesity - Frequent position changes - Coughing - Vomiting |
|
|
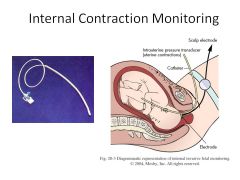
•Intrauterine Pressure Catheter (IUPC)
•Provides information regarding frequency, duration,and intensity. oIntensity of 40-75 mm Hg considered adequate to cause cervical changes. •IUPC is inserted directly into the uterine cavity. oFetal membranes must be ruptured. oCervix must be dilated 2-3 cms. •Pen set at 12-20 mm Hg (normal uterine resting tone). |
|
|
NURSING CARE OF THE LABOR CLIENT:Bloody show,
Vaginal bleeding |
Bloody show
•Subjective data o"What was the frequency and amount of discharge?" •Objective data - Assess during vaginal exam (VE) Vaginal bleeding •Subjective data o"What was the amount, color, & consistency?" •Objective data oObserve drainage only. oVE NEVER DONE IN PRESENCE OF FRESH BLEEDING! |
|
|
NURSING CARE OF THE LABOR CLIENT:Membrane status
|
•Subjective data:
o"Is there leaking?" o"Have you experienced spontaneous rupture of membranes (ROM)?" o"What was the amount? Color? Consistency? and Time of occurrence? •Most of time there is little question about the integrity of the membranes r/t amniotic fluid can be seen draining from the vagina. •However, sometimes fluid is not seen draining --> oQuestion arises of whether membranes are ruptured or not. |
|

|
Nitrazine test
•Done prior to a VE. •Use small section of nitrazine tape --> placed next to moist vaginal tissues. •Tape impregnated with a dye that reacts to amniotic fluid. •Testing involves the pH of the vaginal fluid. oAmniotic fluid = 7.0 -7.5 oVaginal secretions = 4.5- 5.5 oUrine = 5.5 - 6.5 oAmniotic fluid --> color change to blue-green; blue-gray; or deep blue. oVaginal secretions and urine --> no color change. •Bloody show can give false positive reading. •Infections can also give false positive readings. |
|
|
NURSING CARE OF THE LABOR CLIENT
|
•Determination of ROM can also be done with a sterile speculum exam.
oNurse's role - assist MD/CNM oPhysician will visualize the cervix --> sterile cotton swabs are used to collect vaginal secretions from the cervical os. Test with nitrazine or make a slide to check for ferning. •Slide prepared for Fern Test needs to dry for 5-7 minutes.----> Examined under microscope for amniotic fluid. Looks like clusters of fern leaves. •Blood and infections can also interfere with test. Microscopic exam of vaginal fluid. •Fluid place on slide & stained----> •Examined for evidence of: oFetal squamous cells oVernix olanugo •Visualization of fluid emerging from cervical os can bedone --> Ask client to push or cough during speculum exam. oIf fluid seen --> membranes ruptured. |
|
|
Assess fetal membranes during VE
|
Palpate for movable bulging sac through the cervix.
If membranes intact feels like a bulge. Observe for expression of amniotic fluid during VE. |
|
|
Assess Labor Progress
|
Cervical dilation and effacement are evaluated directly with a sterile VE.
1cm----------------------------------------10cm Also assessed during VE: Fetal station Fetal position Determined by the suture lines and position of the fontanelles in relationship to the maternal pelvis. If posterior fontanelle is located just under the maternal pelvic bone --> fetal position is anterior. If posterior fontanelle is located toward the back of the mother's pelvis --> fetal position is posterior. |
|
|
Assessment of Fetal Status:
Subjective & Objective |
Subjective data:
"Has the baby moved or kicked since labor began?" Objective data Abdominal Assessment Position the mother in a supine position, with knees flexed, and a pillow under her shoulders. Done on empty bladder. Examiner needs to warm hands. Inspection - Observe the abdomen for shape & size. Lie of the fetus should be assessed. Uterus projects up & down = Longitudinal lie. Uterus projects left & right = Transverse lie. Where is the movement? Activity reflects the position of the feet. |
|
|
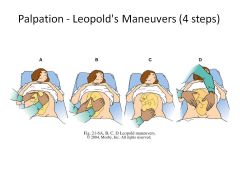
Done between cxs.
Determine fetal position, number of fetuses, and location on fetal heart. |
|
|
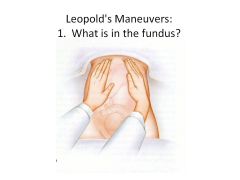
1. What is in the fundus?
Stand facing client --> Palpate superior surface of fundus with both hands. Determine shape, size, consistency and mobility of form. Head: Firm, hard, & round. Moves independently of the body. Buttocks: Less defined, feels softer. Moves only in conjunction with the body. |
|
|
Leopold's Maneuvers:
2. Where is the back and where are the small parts? |
2. Where is the back and where are the small parts?
Use both hands, one on each side of the abd. to determine on which side of the uterus is the back located. One hand stationary, the other palpates. Repeat maneuver reversing palpating hand and stationary hand. Back is hard, smooth, curved, resistant surface. Opposite side - fetal frontal surface (concave & soft) with small parts (hands and feet). |
|
|
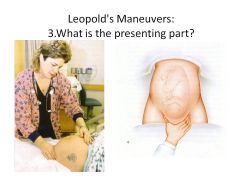
3. What is the presenting part?
To determine which fetal part is presenting over the pelvic inlet. Grasp lower portion of the uterus just above the symphysis pubis, between thumb and fingers; try to press fingers together. If head --> presenting part hard and round. If buttocks --> presenting part soft. This maneuver validates presenting part. |
|
|
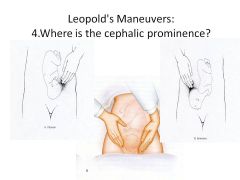
4. Where is the cephalic prominence?
For cephalic presentations, to determine the degree of flexion. Turn around and face client's feet. With fingers of both hands, press in two inches on both sides of abd. just above the symphysis pubis; exert gentle pressure downward in the direction of the birth canal. One hand will meet firm resistance or obstruction = "Cephalic prominence". The other hand will descend down further,without meeting resistance. If cephalic prominence felt on the opposite side of the fetal back, and the same side as the small parts --> feeling brow --> head flexed --> vertex presentation. If cephalic prominence on the same side of the fetal back --> feeling occiput --> head extended and face downward --> face presentation. Also aides in determining descent: If cephalic prominence readily palpable --> head not engaged. After engagement --> difficult to feel cephalic prominence |
|
|
Fetal Heart Assessment:
Doppler or Electronic Monitor |
Fetal heart sounds are transmitted through the convex portion of the fetus that lies in intimate contact with the uterine wall.
Fetal back = Vertex and Breech presentations Chest = Face Presentations |
|
|
Fetal Heart Assessment:
Location of Fetal Heart is according to fetal presentation. |
Cephalic Presentation = Lower quadrant of the maternal abd.
Breech presentation = At or above the level of the maternal umbilicus. Transverse Lie=just above or below the maternal umbilicus. |
|

Fetal Heart Assessment:
|
As the presenting part descends and rotates through the maternal pelvis --> fetal heart location descends
and moves toward the midline. After fetal heart rate (FHR) is located --> counted for one minute. Take mother’s pulse simultaneously with FHR. Nurse should also listen to FHR through and just after a cx to detect any abnormal heart rate. |
|
|
External uses an ultrasound transducer that emits sounds waves.
Water soluble gel applied to aid in conduction. Ultrasound transducer is applied to the abd. via elastic belt. FHR converted into audible beeping sounds --> sounds are translated into electronic impulses and plotted on a graph. |
|
|
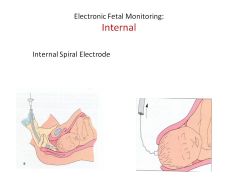
Internal uses a spiral electrode which is attached to the skin of the presenting part.
Attached to the parietal portion of the fetal scalp. To insert internal fetal electrode: 1.Cervix must be dilated 2 cms. 2. Membranes must be ruptured. 3. Fetal presenting part must be accessible by vaginal exam. |
|
|
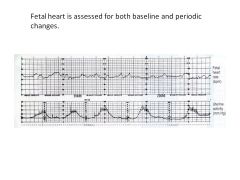
Baseline rate - The range of FHR observed between cxs,during a continuous 10 minute period of monitoring.
Variability also affects the baseline. |
|
|
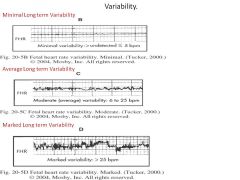
Variability = Normal irregularity of the FHR.
A measure of the interplay effect between the sympathetic nervous system and the parasympathetic nervous system. |
|
|
Two types of variability:
(STV) & (LTV) |
Short Term Variability (STV)
-Change in FHR from one beat to the next. -Commonly charted as present or absent. Long Term Variability (LTV) -Larger rhythmic fluctuations of the FHR. -The difference between the lowest FHR and the highest within one min. Classification: Minimal Variability: < 5 bpm. Average Variability: 6-25 bpm. Marked Variability: > 25 bpm. |
|
|
Periodic changes
|
Transient decelerations or accelerations in the FHR from the baseline that occur in response to cx's and fetal movement.
|
|
|
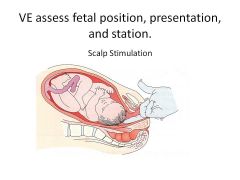
If fetal head is the presenting part – scalp stimulation can be performed.
Applying gentle digital pressure against the head by examiners fingers --> note fetal response. Reactive fetus increase FHR 10-15 bpm. This indicates normal fetal neurologic function. |
|
|
Intrapartum Care:
Laboratory tests Continuous Nursing Care Fetal well being |
Laboratory tests
Urine clean catch CBC Blood type and Rh if not known. Continuous Nursing Care Signs of labor progress: Uterine cxs Women's behavioral response to labor Fetal well being FHR q 15 mins via doppler or evaluated q 15 min if fetal monitor starting in active labor. (less frequent in latent phase). Second stage - q 5 minutes. Assess character of amniotic fluid. |
|
|
Intrapartum Care:
(SROM)& (AROM) |
Spontaneous Rupture of Membranes (SROM) or Artificial Rupture of Membranes (AROM)
Nursing priority: Assess FHR for several minutes and VE for prolapsed cord. Assess characteristics of the fluid. Assess cxs Linen change. |
|
|
Intrapartum Care
|
Fluids
Fluids po – sips of water or athletic drinks. Ice Chips may given to minimize risk of anesthesia complications and because of slowed gastric emptying time. -No solid foods. -IV fluids given to maintain hydration – Use electrolyte soln without glucose. Maintain I & O Urinary elimination -Voiding encouraged q 2 hours. -Assess for palpable bladder or visually distended bladder. -Cath if unable to void. -Assist with ambulation and position changes. -Ambulation encouraged if membranes intact. -When lies in bed - position changes q 30 - 60 min. -Comfort measures -Assess support persons abilities -Prepare of delivery --> table set up. -Documentation after birth - delivery record -Need to calculate length of labor. |
|
|
|
|
|
|
|
|
Nursing Dx
Prior to labor |
Nursing Dx
Prior to labor Anxiety Fear High Risk for Infection First Stage of Labor High risk for injury High risk for altered tissue perfusion Altered urinary elimination Anxiety Fatigue Pain Ineffective individual coping High risk for FVD High risk for infection Second Stage of Labor Altered urinary elimination Altered tissue perfusion Impaired skin integrity Pain Ineffective individual coping High risk for infection Third Stage of Labor Anxiety High risk for FVD |

