![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
What is pulmonary ventilation?
|
Inspiration + expiration
|
|
|
What is inspiration?
|
air is taken into the lungs; external intercostals and diaphragm contract, size of thoracic cavity increases as the diaphragm flattens and the external intercostals lift the rib cage; lungs adhere to pleura so volume of lungs increases and pressure decreases, bringing air in
|
|
|
What is expiration?
|
air passes out of the lungs; inspiratory muscles relax, elastic lung tissue recoils to decrease volumes; this forces gas molecules to come together and increases pressure, so they are pushed out
|
|
|
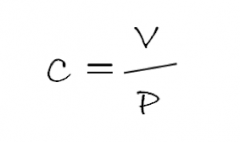
What is Boyle's Law?
|
P=1/V
|
|
|
For the glass bottle apparatus, what happened when the diaphragm was pushed up?
|
internal jar volume decreases and pressure increases; this makes the volume of the balloons (lungs) decrease; air flows out of lungs
|
|
|
For the glass bottle apparatus, what happened when the diaphragm was pulled down?
|
internal jar volume increases, pressure decreased, volume of balloons increased; air goes into lungs
|
|
|
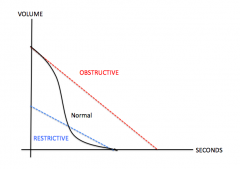
What is chronic obstructive pulmonary disease?
|
airflow in and out of lungs is reduced (asthma or emphysema, bronchitis); to diagnose you need to measure pulmonary flow rates and ERV
INCREASED AIRWAY RESISTANCE, difficult expiration |
|
|
What is chronic restrictive pulmonary disease?
|
decreased lung capacity
Acute lung injury Pleurisy Pulmonary fibrosis Pneumonia Pulmonary edema MS, Obesity, Cystic Fibrosis Difficult inspiration |
|
|
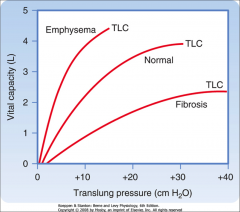
Why is emphysema obstructive?
|
The collapsed alveoli reduces the elastic nature of the lungs, increasing the compliance. Since compliance is increased, the lungs are far too flexible and it is difficult to expel all the air in your vital capacity (VC itself stays the same). That's why it's obstructive - because the increased compliance obstructs the total expelling of air. If you can't breathe out as much, in the case of emphysema, how does that affect the lung capacities? Hint: think of expiratory reserve volume.
|
|
What are the question marks?
|
|
|
|
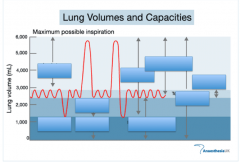
What is tidal volume?
|
the amount of air inhaled or exhaled with each breath under resting conditions (normal quiet breathing); ~500 mL
|
|
|
What is inspiratory reserve volume?
|
the amount of air that can be forcefully inhaled after a normal tidal volume inhalation; ~3100 mL
|
|
|
What is expiratory reserve volume?
|
the amount of air that can be forcefully exhaled after a normal tidal volume exhalation; ~1200 mL; reduced in obstructive diseases like emphysema because it’s tiring to get air out
|
|
|
What is vital capacity?
|
the maximum exchangeable air in the lungs. The maximum amount of air that can be exhaled after maximal inspiration.
|
|
|
What is residual volume?
|
amount of air remaining in lungs after max exhalation; about 1200 mL, important because it allows gas exchange to go on continuously even between breaths
|
|
|
What equation relates several properties of lungs?
|
VC= TV + IRV + ERV: ~4800 mL
|
|
|
What does the dry spirometer measure?
|
measures volumes exhaled air only; need to reset to 0 after each trial
|
|
|
How do we calculate minute respiratory volume?
|
= Tidal Volume x Respirations/minute=liters/minute
|
|
|
What did we calculate with the dry spirometer?
|
• ERV (breathe additional air out as much as you can after exhaling from normal breath)
• Vital capacity (inhale as much as possible and exhale as much as possible) |
|
|
What did we calculate AFTER using the dry spirometer?
|
• Percentage vital capacity; Percentage VC=(measured VC/Predicted VC) x 100
• Inspiratory reserve volume; IRV=VC – (TV + ERV); normal range is 2100 to 3100 mL • Residual volume: Predicted RV=Vital capacity x age correction factor |
|
|
Purpose of using pulmonary function test/peak flow meter:
|
: helps clinician distinguish between obstructive and restrictive pulmonary diseases; airway resistance increased in obstructive disorders but in restrictive total lung capacity declines
|
|
|
What did we measure using the peak flow meter?
|
• Peak expiratory flow rate (in L/min); predicted average peak flow rate=what we measured x age correction factor
|
|
Fill in da blanks
|
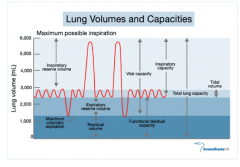
|
|
|
How did we calibrate the biopac?
|
used calibration syringe, blew through bacteriolcal filter; needed to hold parallel to ground because sensitive to gravity; simulating five breathing cycles (pushing plunger in for one second, waiting two seconds, pulling plunger out for one second, waiting two seconds)
|
|
|
How did we use the biopac in part 1?
|
three normal breaths, inhaled as much as possible, three normal breaths, exhaled as much as possible, inhaled (given L)
|
|
|
What specifically did we measure with the biopac in part 1?
|
• Measured tidal volume for first three breaths (diff between highest and lowest peaks)
• IRV: highlighted from peak of maximum inhalation to last peak of normal respiration right before it • ERV: highlighted from the trough of max exhalation to trough of last normal exhalation • VC: peak of max inhalation to trough of max exhalation • Assumed residual volume is 1.0 L because can’t measure it |
|
|
How did we measure the predicted vital capacity?
|
Males=.052 (height in cm)- .022(age in years) – 3.60
Females: .041(height in cm) - .018(age in years) – 2.69 Measured values 20% lesser or greater than the calculated predicted value are normal |
|
|
What did we measure in the second part of the biopac lab?
|
measuring Forced Expiratory Volume; a test in which a limit is placed on the length of time a subject has to expel vital capacity air
|
|
|
What is FEV1?
|
percentage of vital capacity expelled forcibly after a max inhalation in period of one second; usually 66-83%
|
|
|
What is FEV2?
|
percentage of vital capacity expelled forcibly after a max inhalation in period of two seconds; usually 75-94%
|
|
|
What is FEV3?
|
percentage of vital capacity expelled forcibly after a max inhalation in period of three seconds; usually 78-97%
|
|
|
Does an asthma patient have a normal vital capacity? FEV?
|
Asthma patient has a normal vital capacity but FEV reduced due to heavy mucus secretion; airway diameter is reduced, longer to get that air out
|
|
|
How did we measure FEV with biopac?
|
had person breathe normally for three cycles, then inhaled as much as possible and exhaled as quickly as possible for three seconds
|
|
|
How did we analyze the data with the biopac in part 2?
|
• Selected where we started the maximum exhale, use delta T to determine the three seconds, click calculate FEV; from there use p-p measurement [max value in selected area] for each interval (it represents vital capacity)
|
|
|
Would a smaller subject tend to have less or more vital capacity than a larger person?
|
Less—plugging a smaller height in the VC predicted equation gives it a lower value.
|
|
|
Individuals with asthma tend to have smaller airways due to smooth muscle constriction, excess mucus secretion, and thickened walls in the bronchial tree. How does this affect their vital capacity, and the FEV?
|
Vital capacity wouldn’t change because it is only dependent on height and age. FEV would decrease because less air would be able to be expelled in one second due to a smaller aiway.
|
|
|
What is compliance?
|
A measure of a lung’s resistance to changes in volume at a given pressure: how “stiff” the lung is.
|
|
|
What is high compliance?
|
High compliance: poor elastic recoil, “floppy lungs”
problem exhaling air |
|
|
What is low compliance?
|
high elastic recoil, “stiff lungs”
problem inhaling air |
|
|
What are factors affecting lung compliance?
|
Chest wall stiffness (extrinsic...scoliosis, pleurisy, obesity, arthitis, ALS)
Lung stiffness (intrinsic) Elasticity of lung tissue (intrinsic...fibrosis) and surface tension (intrinsic) |
|
|
Can we use FEV to distinguish between diseases?
|
Not really...decreases in all segments for asthma (obstructive) AND fibrosis (restrictive)
|
|
|
What type of disease does a spirometer measure?
|
Restrictive diseases because detects lung volumes
|
|
|
What type of disease does a peak flow meter measure?
|
Obstructive diseases; measures the max speed you can exhale
|
|
|
What is FVC vs FEV?
|
FVC is simply a measure of vital capacity.
It’s “forced” to get the true value Repeated 3x FEV is simply a measure of volume exhaled, over a particular time interval. |
|
|
What diseases affect compliance?
|
|

