![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What are the cardiovascular diseases drugs are useful in treating? |
hypertension:high blood pressure angina:temporary cardiac pain, usually on exercise myocardialinfarction: sustainedcardiac pain and cell death due to coronary thrombosis arrhythmias:lack of normal heart rhythm heartfailure: insufficient cardiac output to meet body’s needs |
|
|
What are some risk factors in cardiovascular disease? |
High LDL Smoking Obesity Diabetes Male gender Age Family history |
|
|
What can Vasculardysfunction lead to? |
Atherosclerosis, Hypertension |
|
|
What does atherosclerosis directly lead to? |
Angina, Thrombosis |
|
|
What does Hypertension lead to? |
Stroke, Heart failure |
|
|
What else causes a stroke? |
Thrombosis |
|
|
What else do Thrombosis lead to? |
Acute MI |
|
|
What does an acute MI lead to? |
Heart failure ----> Arrhythmias and sudden cardiac death |
|
|
What is atherosclerosis? |
Coronaryheart disease results from atherosclerosis - thebuild-up of cholesterol-rich plaques, causing a stenosis (narrowing) of the arteries |
|
|
What type of process is atherogenesis? |
Atherogenesis: a progressive process Fattystreak ----> Atherosclerotic plaque ----> Plaque ruptureandthrombosis |
|
|
What are acute coronary syndromes precipitated by? |
‘Acutecoronary syndromes’precipitatedby sudden ↓in coronary flow |
|
|
What does thrombosis cause? |
unstableangina NonST segment elevation MI STsegment elevation MI |
|
|
What does the stable plaque lead to? |
vasoconstriction, spasm ----> loss of coronary flowreserve → stable angina Precipitated by an ↑inmyocardial O2 demand |
|
|
What are the main risk factors in athersclerosis? |
Highplasma cholesterol(>5 mM) smoking diabetes Age, male gender, family history HYPERTENSION |
|
|
What is angina caused by? |
Affects~ 2m people in UK •temporary squeezing sensation orpain in chest •most common form = stableangina (angina of effort) •triggered by excitement or exertion •results from cardiac O2demand with restricted blood flow |
|
|
What helps to reduce angina? |
Growthof coronary collaterals helps to reduce the severity of angina |
|
|
What is the drug treatment for angina? |
• ↑O2 supply to ischaemic zone by dilating coronary arteries (mainly collateral arteries will dilate) •↓Cardiac workload and O2 demand = main treatment strategy |
|
|
What is the surgical treatment for angina? |
Using surgery • ↑O2 supply: open up arteries using percutaneous coronary intervention (PCI) or bypass surgery |
|
|
What is Cardiacworkload determined by? |
preload: central venous pressure afterload: arterial pressure and TPRcontractility: stimulation of b-receptorsheart rate |
|
|
What do organic nitrates do? |
Organicnitrates: decreased preload, so decreased workload and O2 demand |
|
|
What do B-blockers do? |
•b-blockers: decreased HR and force, so decreased cardiac workload and demand for O2 •Ivabradine: decreased HR |
|
|
What do Ca2+ channel blockers do? |
•Ca2+ channel blockers •Nicorandil decreased TPR (afterload), so decreased workload and O2 demand |
|
|
How do nitrates decrease workload? |
• nitrates relax veins mainly, so ↓ venous pressure • ↓ “preload” (stretch of heart musclebefore the next beat), so decreased cardiac output (Starling) • so, ↓ workload+ O2demand of heart |
|
|
What do organicnitrates cause? |
NO ---> veinsdilate ----> ↓ cardiac work ---->coronarycollateralsdilate |
|
|
What is the Surgical treatment of angina? |
Coronaryartery bypass grafting (CABG) Percutaneouscoronary intervention (PCI), angioplasty |
|
|
What is a myocardial infarction? |
infarction = deathof myocardial tissue |
|
|
What does MI result from? |
MIresults from coronary thrombosis |
|
|
What happens in coronary thrombosis? |
rupture of atherosclerotic plaque in coronary artery -----> platelet aggregation + bloodcoagulation -----> formation of thrombus (clot insidevessel) -----> regional ischaemia ------> cardiac cell death (myocardial infarction, MI) in a few hours |
|
|
What are the consequences and treatment of severe myocardial ischaemia? |
Arrhythmias •about25% of people die from ventricular fibrillation (VF) •use defibrillator if VF occurs Severe pain (usually) •givemorphine or diamorphine i.v. Poor contractility and then cardiac cell death •cellstake up to 12 hours to die; removing the thrombus duringthis time can save cardiaccells (and thus patients’ lives!). |
|
|
What is Emergencycoronary reperfusion? |
•PerformPCI asap •Use athrombolytic drug i.v. (e.g. alteplase) to break down the thrombus thatis causing the blockage: works by breaking down the fibrin network in the bloodclot •Alsogive antiplatelet drugs, e.g. aspirin plus clopidogrel, which inhibit further plateletaggregation:- aspirin inhibits COX, the enzyme thatproduces the pro-aggregatory factor, thromboxane A2 (TXA2) -clopidogrel inhibits the binding of thepro-aggregatory factor, ADP, to its receptor on platelets |
|
|
What is CHRONIC HEART FAILURE? |
When cardiac output is too low to perfuse tissues adequately (due toabnormally-low contractility) •can result from MI, hypertension,etc. •leads to oedema, breathlessness and ’cardiacremodelling’ an enlarged but weaker heart |
|
|
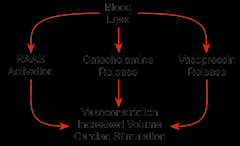
What is the short term blood loss? |
|
|
|
What are the long term effects of heart failure? |
↓ ↓ cardiac output pulmonary oedema arrhythmias cardiac remodelling |
|
|
What are the long term treatments of heart failure? |
Long-term: aim to decrease progressivecardiac remodelling and symptoms: •ACE inhibitors or angiotensin receptor blockers, ARBs (slow cardiacremodelling, decreaseTPR) • b-blockers (decrease symp. stimulation of heart, slow cardiac remodelling) •Aldosterone antagonists (slow cardiac remodelling)Plus •diuretics (reduce oedema) •digoxin (positive inotropic drug) |
|
|
What is Acute(short-term) inotropic support in severe HF? |
b1-adrenoceptoragonists to keep patient alive e.g. dobutamine |
|
|
How are arrhythmias treated? |
Treat with: •defibrillator for VF •drugs (see previous lecture) •surgery to destroy ectopic site ofimpulse generation (radiocatheter ablation), or to implant pacemaker |
|
|
What is bp determined by? |
BP =CO x TPR |
|
|
What is the general definition of hypertension? |
General definition: if BP > 140 / 100 mm Hg = systolicBP / diastolic BP |
|
|
Why do we need to treat hypertension? |
•Need to treat, as is major riskfactor for:–atherosclerosis (causes coronary heart disease)–stroke (can burst a cerebral artery) |
|
|
What lifestyle changes can help? |
•Lifestyle changes help: –lose weight if overweight/obese –eat less salt –take exercise–change job! |
|
|
What are the causes of primary hypertension? |
Thecauses of primary hypertension (the most common type) are unknown. Inthe long term, BP is controlled by the kidneys (Guyton hypothesis)… and perhapsbythe ANS acting to regulate vascular tone and TPR (neurogenic hypothesis) |
|
|
Is a single drug used in most people? |
Nosingle type of anti-hypertensive drug works in >60% of people…Mostpeople must use several of these drugs simultaneously |
|
|
What are the Generalstrategies to reduce risk of CV disease and MI? |
Healthier lifestyle •stop smoking •replace saturated fats in diet with polyunsaturated & monounsaturated fats and eat lesssugar (diabetes →coronary heart disease) •do more exercise •take: omega-3 fish oils, alcohol,antioxidants ???? Give drugs long-term, e.g.: •statins, e.g. simvastatin, to reduce plasma cholesterol by ↓ synthesis of cholesterol in liver•low-dose aspirin to reduce risk of thrombosis |

