![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
41 Cards in this Set
- Front
- Back
|
Hypothalamus and pituitary geography |
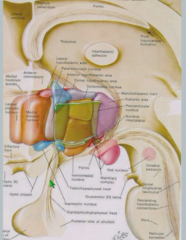
Hypthalamus and pituitary are connected by infundibulum or stalk. Pituitary sits in sella turcica behind eyes |
|
|
Pituitary and optic chiasm relation |
Pituitary is located below optic chiasm - pituitary tumor can cause loss of peripheral vision. |
|
|
Pituitary and carotid sinus relation
|
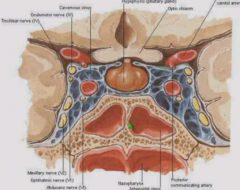
Carotid sinus is lateral to pituitary - pituitary tumor can cause cranial nerve palsies and affect blood flow. Sinus also provides surgical access to pituitary |
|
|
Pituitary on MRI |
Posterior pituitary is "posterior bright spot" |
|
|
Embryonic origin of pituitary
|
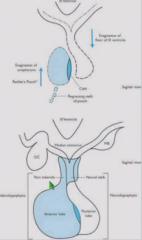
Anterior (adenohypophysis) - from roof of mouth as Rathke's pouch. Formed from trophic and glial cells. Posterior (neurohypophysis) - from third ventricle of brain/diencephalon. Consists of nerve endings |
|
|
Transcription factors which influence pituitary development |
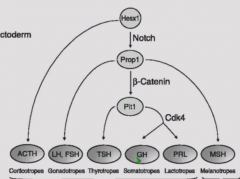
Hesx1, Prop1, PitI Different deficiencies knock out different sets of hormones |
|
|
Magnocellular vs parvocellular neurons |
Magnocellular - project from hypothalamus to posterior pituitary. Secrete vasopressin and oxytocin Parvocellular - release releasing factors into portal plexus which act on anterior pituitary |
|
|
Blood supply of pituitary |
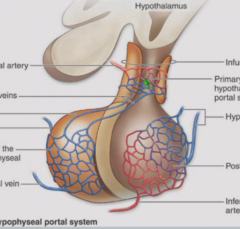
Anterior - portal plexus consists of primary plexus in median eminence and secondary plexus in trophic cells. Exits via anterior pituitary vein. Posterior - One capillary bed of leaky capillaries which neurons project to. |
|
|
Anterior Pituitary hormones |
FLAT PG FSH, LH, ACTH, TH, Prolactin, GH |
|
|
Cell types in anterior pituitary |
Gonadotrophs (LH and FSH) Thyrotrophs (TSH) Somatotrophs (GH) Lactotrophc (Prolactin) Corticotrophs (ACTH) Somatotrophs are predominant, 50% of mass of anterior pituitary. |
|
|
Somatotroph vs gonadotroph morphology |
Somatotrophs have larger nucleus and fewer secretory granules than gonadotrophs. |
|
|
Categories of trophic hormones |
Glycoprotein hormones - LH, FSH, TSH, hCG Somatomammotrophic hormones - Prolactin, GH Derivatives of proopiomelanocortin - ACTH, MSH |
|
|
Glycoprotein trophic hormones |
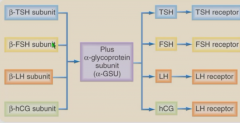
Share a common alpha subunit, diverge at beta subunit. Similar structure so can crossreact. During pregnancy, high hCG stimulates tSH receptor, causing hyperthyroidism. Tumors can secrete just alpha subunit - high alpha subunit levels indicate tumor growth. |
|
|
Somatomammotrophic hormones |
Prolactin and GH Common precursor cell (somatomammotroph), which some anterior pituitary tumors resemble, cosecretes growth hormone and prolactin. |
|
|
List of releasing factors |
GnRH -> LH and FSH TRH -> TSH GHRH -> GH CRH -> ACTH |
|
|
Action of releasing factors |
Released into portal plexus and acts on anterior pituitary to a) control Ca2+-dependent release of trophic hormones b) directly stimulate trpohic factor synthesis Acts via GPCRs except PL and GH. |
|
|
Hypothalamic inhibiting hormones |
Somatostatin inhibits growth hormone. Dopamine inhibits prolactin. |
|
|
Clinical causes of high prolactin |
Prolactin is released when dopamine is absent. Antipsychotic medications can cause rise in prolactin. Tumors causing compression of stalk can also cause increase in prolactin. |
|
|
Characteristics of hypothalamic releasing hormones |
Secreted in pulses Act on plasma membvrane receptors Transduction through cAMP (except GH and prolactin) Stimulate hormone release and synthesis Cause hypertrophy and hyperplasia of target pituitary cells, or tarophy is not secreted. |
|
|
Three hypothalamic-pituitary axes |
Gonadal-hypothalamic-pituitary - GnRH - LH/FSH - estrogen/androgens Adrenal-hypothalamic-pituitary - CRH - ACTH - glucocorticoids Thyroid-hypothalamic-pituitary - TRH - TSH - T3/T4 |
|
|
Ultra-short, short, and long feedback loops |
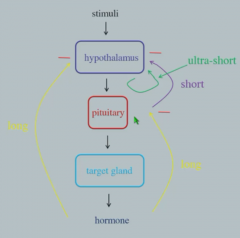
Short - Pituitary hormones inhibit production of hypothalamic releasing hormones. Long - Hormone produced by target cell inhibits production of hypothalamic-releasing factors. Ultra-short - Pituitary hormone inhibits its own production |
|
|
Cortisol circadian rhythms |
Peaks early in morning to help start metabolism. Lowest at midnight. Cortisol or ACTH-producing tumor abolishes circadian pattern - cortisol will always be high. Always check cortisol at night for hypercortisolism and in morning for adrenal insufficiency to sense abnormalities |
|
|
Puberty and HPGA |
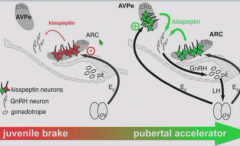
HPGA is suppressed before puberty. At puberty, estrogen stimulates GnRH in cyclical fashion, mediated by kisspeptin and other hormones. |
|
|
Function of LH and FSH |
LH - stimulates ovulation, testosterone production FSH - follicular growth, sperm production |
|
|
LH pattern in men |
LH pattern is pulsatile, random. More in night and early morning to cause morning rise in testosterone. |
|
|
LH pattern in women |
LH is cyclical because ovulation cycle is stimulated by LH surge. Some pulsatility as well. |
|
|
FSH pattern |
FSH levels are more stable than LH levels - high FSH used to diagnose menopause. |
|
|
Progesterone pattern in ovulation cycle |
Progesterone peaks in luteal phase |
|
|
Estradiol and LH/FSH |
Increase in estradiol inhibits LH/FSH release but stimulates LH surge in menstrual cycle. |
|
|
GnRH synthesis |
Created from 92 amino acid precursor, preproGnRH Cleaves into 10 amino acid peptide |
|
|
GnRH neuron embryology |
Originate in olfactory placode, migrate into brain |
|
|
Kallman's Syndrome |
Blocked migration of GnRH neurons from olfactory placode to brain. Hypogonadotrpoic hypogonadism (low androgens, GnRH, LH/FSH) and infertility accompanied by anosmia (difficulty smelling) |
|
|
GnRH neurons |
Few in number with only a small number of synapses. Feedback via small amount of estrogen receptors (direct feedback) and some intermediate feedback via other neurons. |
|
|
GnRH secretion pattern |
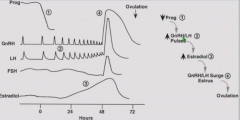
Episodic and pulsatile. Higher in follicular phase (to stimulate FSH/LH) and lower in luteal phase. Slows down in luteal phase due to progesterone. |
|
|
Continuous GnRH release |
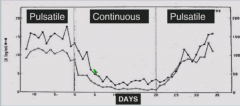
Continuous GnRH release causes suppression of LH and FSH - pulsatility is important. Continuous GnRH used in prostate cancer or precocious puberty to suppress LH, suppressing testosterone production. |
|
|
Pituitary gonadotroph response |
Membrane receptors for GnRH Induces IP3 pathway leading to Ca2+ influx Causes secretion of FSH, LH, or both FSH and LH. |
|
|
hCG in infertility treatment |
hCG stimulates LH and FSH receptors - can be used for infertility treatment |
|
|
ACTH production |
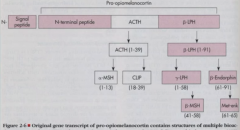
ACTH is cleaved from preprohormone proopiomelanocortin in anterior pituitary |
|
|
Effect of primary adrenal insufficiency on HPAA |
Primary adrenal insufficiencycauses decrease in cortisol and increase in CRH and ACTH. Also increases MSH because of increase in proopiomelanocortin - causes tanning as a side effect. |
|
|
Triggers for ACTH |
CRH Stress Hyperglycemia Hypoglycemia Depression Time of day - morning Vasopressin from posterior pituitary- minor effect Inhibited by cortisol |
|
|
Pattern of ACTH and cortisol |
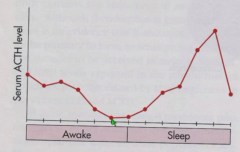
ACTH and cortisol levels go up during sleep and peak in morning. |

