![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Functions of kidney |
1. Maintain homeostasis despite waste products of diet and metabolism, and environmental and clinical changes 2. Secrete hormones - renin, angiotensin II, prostaglandings, bradykinins, erythropoietin, 1,2(OH)2 vitamin D3 (calicitriol) 3. Catabolize peptide hormones - e.g. insulin which persists in kidney disease 4. Organ of gluconeogenesis, secondary to liver |
|
|
Amount of filtration per day |
150-180 L/day |
|
|
Glomerulus |
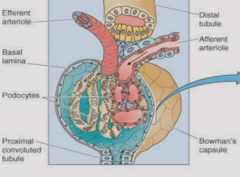
Has capillary tangle from which absorption occurs into Bowman's space Has endothelial cells and specialized epithelial cells (podocytes) with interdifitating foot processes that wrap capillary network and line Bowman's capsule - visceral and parietal epithelial |
|
|
Distal tubule |
In apposition to arterioles Senses transit of solutes, communicates to arterioles through macula densa Whole apparatus is juxtaglomerular apparatus |
|
|
Filtratoin barrier |
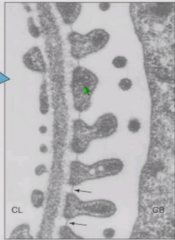
Composed of: Fenestrated endothelium lining capillary lumen Basement membrane of glomerulus - made of type 4 collagen and negatively charged moieties i.e. heparan sulfate. Bowman's capsule with epithelial foot processes separated by spaces |
|
|
Particles filtered by filtration barrier |
RBCs and large proteins remain in blood Medium sized proteins are slowed Plasma water and solutes pass freely |
|
|
Layers of kidney |
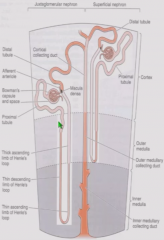
Cortex - glomeurulus and promximal tubules Outer medulla - superficial glomerulus' Loops of Henle Inner medulla - Juxytomedullary glomerulus' Loops of Henle Collecting duct has cortical, outer medullary, and inner medullary portions |
|
|
Nephron |
Glomerulus to distal tubule (Collecting ducts are shared and embryologically distinct from rest of nephron) |
|
|
Blood supply to nephron |
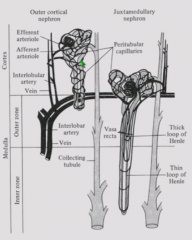
Afferent aa. -> glomerulus -> efferent aa. Efferent arterioles gives rise to peritubular capillary network which removes reabsorbed molecules and secretes secreted molecules. Juxtamedullary nephrons also have thin straight capillaries, vasa recta, which travel with Loop of Henle and help create high osmolality in medullary interstitium. All blood empties to renal vein. |
|
|
Standard processes of nephron |
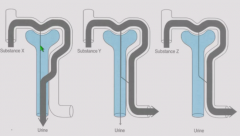
Filtration - across glomerulal capillary basement membrane. Only fraction of plasma water is filtered. Secretion - from peritubular capillaries to tubule Reabsorption - from tubule to peritubular capillaries Scenarios include: filtration with complete secretion, filtration with complete reabsorption, and filtration with net reabsorption (less appears in urine than initially filtered) |
|
|
Reabsorption of key ions |
Water - 98-99% absorbed Na+ - 99% reabsorbed. Some excreted because modern diet is Na+-rich. HCO3- - 100% reabsorbed K+ - 85-95% reabsorbed. Abundant in diet so partly excreted. Urea - 40-50% reabsorbed. Keep some to help conserve water. |
|
|
Clearance |
Removing substance from circulation either by transformation (metabolism) or removal by kidney (renal clearance) Clearance can be described by: - Rate - amount of solute removed/unit time - Half life - Volume of plasma/unit time from which all of substance is removed (mL/min or L/day) |
|
|
Inulin |
Freely filtered and neither secreted nor reabsorbed. Filtered inulin = secreted inulin GFR * Pin = V * Uin, where V = urine flow rate, Pin = plasma inulin concentration GFR = V * Uin/Pin = 125 mL/min |
|
|
Creatinine |
Creatinine behaves like insulin - filtered almost completely at glomerulus but a little secretion. Continuously produces as creatine by muscle and proportion to muscle mass. Stable for each person. Metabolized to creatinine in liver Endogenous so does not have to be administered. |
|
|
Creatinine clearance |
C(creatinine) = V * Ucr/Pcr We can measure flow rate as mL/day instead of mL/minute and then divide by 1440 min/day. |
|
|
Relationship between plasma creatinine and GFR |
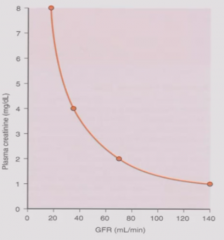
Inverse relationship between plasma creatinine and GFR. GFR = V*Ucr/Pcr Pcr = V*Ucr/GFR Kidney disease leads to loss of glomerular filtration surface area, reducing GFR and raising plasma creatinine. |
|
|
Result of removal of kidney on GFR, creatinine production and excretion of plasma creatinine |
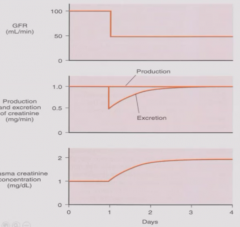
GFR immediately drops to 50%. Creatinine production remains same (function of muscle mass). Creatinine excretion rapidly drops but then increases until baseline because... Plasma creatinine increases to double so that a normal amount remains excreted. |
|
|
Compensatory hypertrophy |
After removal of kidney, growth of contralateral kidney (tubular cell hypertrophy and hyperplasia without new nephrons because glomerulogenesis complete by 32 weeks gestation) Overall GFR is normalized due to increase in single nephron GFR |
|
|
Cases where compensatory hypertrophy is incomplete |
Chronic renal disease of other kidney - single nephron GFR already augmented Elderly - progressive loss of glomeruli, impaired ability to augment SNGFR Growth restricted infants (maternal starvation, placental insufficiency) |
|
|
Urea clearance |
Curea = V * Uurea/Purea = 70mL/min Urea is freely filtered and partially reabsorbed so clearance < GFR. Urea clearance varies with water balance and need to use urea to conserve H2O. |
|
|
RPF |
Paraaminohippurate (PAH) is both filtered at glomerulus and secreted at tubules. All of PAH will appear in urine and none in renal vein. P(pah in artery) * RPF (artery) = (P(pah in vein) * RPF(vein)) + (Upah * V) Vein term cancels out because PAH is not found in veins. RPF = V * Upah/P(pah in artery) = 625 mL/min |
|
|
Renal blood flow |
Renal blood flow = RPF/1-hematocrit = 1300 mL/min, or 20% of cardiac output |
|
|
Filtration fraction |
GFR/RPF = 125/625 = 0.2 20% of plasma water is filtered at glomerulus Can be modified |

