![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
a. What two findings are indicative of a lateral patellar dislocation on an MRI?
|
i. Torn medial patellar ligament
ii. Bruise of lateral epicondyle |
|
|
b. What are the risk factors for patellar dislocation?
|
i. Female
ii. Family hx iii. Prior hx iv. Degree of trauma |
|
|
c. What is the function of the medial patellofemoral ligament?
|
i. Primary stabilizer of lateral displacement (50-60%)
ii. First 20-30 degrees of flexion-- stabilizer |
|
|
d. What muscle weakness can increase the incidence of MPFL rupture?
|
i. VMO dysplasia
|
|
|
e. What is the non-operative treatment of patellar dislocation?
|
i. Pelvifemoral rehab
ii. Core strengthening iii. VMO strengthening iv. Orthoses v. Taping |
|
|
f. What is the rate or redislocation in MPFL rupture?
|
i. 15-44%
|
|
|
g. What is the gold standard for surgical treatment of MPFL rupture?
|
i. Reconstruction
|
|
|
h. When is surgery indicated in MPFL rupture?
|
i. Hx of 2 documented patellar dislocations
ii. Excessive lateral mobility on PE |
|
|
i. What tissues are used for a graft it MPCL reconstruction?
|
i. Tibialis anterior (allo)
ii. Hamstring (auto) |
|
|
j. What is the recovery time for an MPFL reconstruction?
|
i. 3 months to get back to sports
|
|
|
k. What is the recovery time for an ACL rupture?
|
i. 6 months
|
|
|
l. What is the redislocation rate after an MPFL reconstruction?
|
i. 1%-2%
|
|
|
a. What is a Segond fracture?
|
i. Avulsion fracture of new anterolateral ligament of knee
ii. Associated with ACL tear |
|
|
b. What are the symptoms of a meniscus tear?
|
i. Unable to continue (sport)
ii. Clicking and pain on medial side of knee |
|
|
c. What is a meniscus tear?
|
i. Disruption of meniscus integrity
|
|
|
d. What makes up the menisci?
|
i. Fibrocartilage
|
|
|
e. What is a bucket-handle tear of the meniscus?
|
i. Vertical longitudinal tear
ii. Becomes displaced into intercondylar notch of femur iii. Leg can’t extend fully, can flex a little iv. EMERGENT PROBLEM |
|
|
f. What can cause a meniscal tear?
|
i. Twisting
ii. Stepping wrong iii. Antecedent minor injury |
|
|
g. How do you dx a meniscal tear?
|
i. Clinically
ii. MRI to evaluate character of tear iii. **Joint line pain iv. McMurray test |
|
|
h. How many meniscal tear patients develop radiographic arthritis in 10-20 years after surgery?
|
i. 50%
|
|
|
i. What are some factors that can make a meniscus tear worse?
|
i. Women
ii. Obesity |
|
|
a. What does A mean in a Lachman test?
|
i. Good endpoint
|
|
|
b. What does B mean in a Lachman test?
|
i. No solid endpoint
|
|
|
c. What Lachman grade indicates an ACL tear?
|
i. Grade II
|
|
|
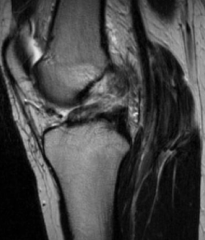
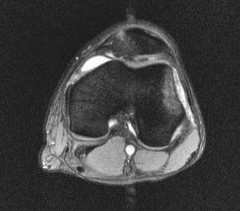
d. What is indicative of an ACL tear on an MRI?
|
i. Bone bruise of lateral femoral condyle
|
|
|
e. How long is the recovery for an ACL tear?
|
i. 4-6 months
ii. Can be seen in office up to a year later |
|
|
f. What can cause an ACL tear?
|
i. Twist on planted foot
ii. Fall from height |
|
|
g. What are the symptoms of an ACL tear?
|
i. Joint effusion
ii. Lachman grade II iii. + pivot shift |
|
|
h. What happens to the ACL bundles during extension?
|
i. Anteriomedial-- loosens
ii. Posteromedial-- tightens |
|
|
i. What happens to the ACL bundles during flexion?
|
i. Anteromedial tightens
ii. Posterolateral loosens |
|
|
j. At what degree is the anteromedial bundle of the ACL tensioned during a repair?
|
i. 30 degrees
|
|
|
k. What is crepitation?
|
i. Crackling or grinding in knee
|
|
|
l. What % of adults develop osteoarthritis 10 years after an ACL reconstruction?
|
i. 50%
|
|
|
a. What are the elements of management of osteoarthritis?
|
i. Weight management
ii. Self management education iii. Physical activity iv. Injury prevention |
|
|
ACL tear MRI
|
|

|
ACL tear MRI
|
|

|
Meniscal tear
|
|
|
Patellar dislocation MRI
|
|
|
b. What should a person with a BMI >25 do to reduce their risk of OA?
|
i. Lose 5% BW
|
|
|
c. What are some activities you can do for non-operative management of OA?
|
i. Education
ii. Low impact aerobics iii. Maintain flexibility iv. Quad strengthening v. Patellar taping |
|
|
d. What medications can you take for OA?
|
i. NSAIDs and/or acetaminophen
ii. Don’t rx glucosamine and chondroitin |
|
|
e. What medications should someone with GI problems take for OA?
|
i. Acetaminophen
ii. Topical NSAIDs iii. COX-2 inhibitors |
|
|
f. What is the use of steroid injections in the tx of OA?
|
i. Provide short-term relief
|
|
|
g. What treatments are contraindicated for OA?
|
i. Hyaluronate products
ii. Needle lavage iii. Arthroscopy for primary dx of DJD |
|
|
h. What will a radiograph show in OA?
|
i. Loss of joint space
ii. Subchondral cysts iii. Sclerosis iv. Osteophyte formation |
|
|
i. What is the technique behind marrow stimulation?
|
i. Microfracture
|
|
|
j. What is the last resort for OA tx?
|
i. Knee arthroplasty
|

