![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
56 Cards in this Set
- Front
- Back
|
What is the most common type of laryngeal malignancy?
|
Squamous cell carcinoma - 85-95%
|
|
|
What are the risk factors for laryngeal ca?
|
Tobacco
Alcohol History of prior head and neck SCCA Risk related to tobacco use doe not decrease to baseline despite tobacco cessation for several yrs Other environmental RF such as exposure to wood dust, paint, etc have been reported in the literature but not well studied. |
|
|
What is the clinical presentation of laryngeal cancer?
|
Hoarseness, dysphagia, aspiration, odynophagia, otalgia, dyspnea, hemoptysis, wt loss, globus sensation, and sore throat greater than 2 weeks.
|
|
|
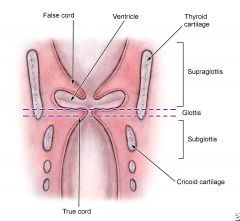
Laryngeal Anatomy and Boundaries - Supraglottis
Which arteries supply the supraglottis? |
Superior laryngeal arteries
|
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What are the boundaries? |
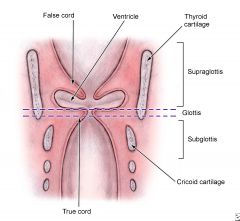
Extends from the superior surface of epiglottis to lateral margin of ventricle at junction of false vocal fold with true vocal fold.
|
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What is the quadrangular membrane? |
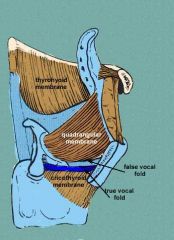
Fibroelastic membrane extending from epiglottis to arytenoids and corniculate cartilage
|
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What are the subsites of the supraglottis? |
Suprahyoid epiglottis
Infrahyoid epiglottis Aryepiglottic folds Arytenoids Ventricle |
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What are the boundaries? |
Extends 1 cm below apex of ventricle
|
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What is the conus elasticus? |
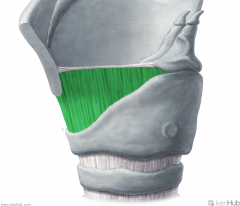
Fibroelastic membrane extending from cricoid cartilage to vocal ligament, limits spread of cancer laterally
|
|
|
Laryngeal Anatomy and Boundaries - Supraglottis
What is Broyles' tendon? |
insertion of vocalis tendon to thyroid cartilage
potential area for tumor spread to thyroid cartilage |
|
|
Laryngeal Anatomy and Boundaries - Glottis
What are the subsites? |
True vocal cords (including ant/post commissure)
|
|
|
Laryngeal Anatomy and Boundaries - Subglottis
What are the boundaries? |
Extends from glottis to inferior border of cricoid cartilage
|
|
|
Laryngeal Anatomy and Boundaries - Subglottis
Which arteries supply the subglottis?? |
Supplied by inferior laryngeal arteries
|
|
|
Laryngeal Anatomy and Boundaries - Subglottis
What are the subsites? |
No subsites..
|
|
|
Where does the pre-epiglottic space extend from?
|
Anterior to epiglottis
Extends from hyoepiglottic ligament/vallecular to thyroid cartilage/thyroepiglottic ligament, bounded anteriorly by thyrohyoid membrane |
|
|
Where does the paraglottic space located?
|
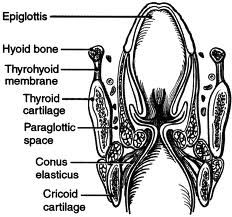
Space outside conus elasticus and quadrangular membrane that may allow for submucosal, transglottic spread of tumor
|
|
|
What is the Reinke's space? What is the importance of this space?
|
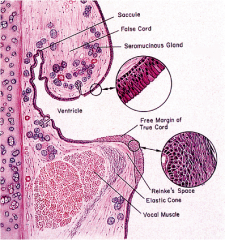
Superficial lamina propria of true vocal fold
- can get edema there..especially in SMOKERS! |
|
|
What is the typical spectrum of premalignant laryngeal lesions?
|
hyperplasia --> atypia --> dysplasia (mild/moderate/severe) --> carcinoma in situ (CIS)
|
|
|
How are mild, moderate and severe dysplasia classified? How about CIS?
|
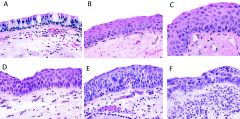
Mild dysplasia - cellular abnormalities limited to basal 1/3 of epithelium (C in image)
Moderate dysplasia - cellular abnormalities up to 2/3 of epithelium thickness (D in image) Severe dysplasia - cellular abnormalities > 2/3 of epithelium thickness (E in image) CIS - intraepithelial neoplasm w/o basement membrane or stromal invasion (F in image) |
|
|
What is the incidence of malignant transformation for mild/moderate dysplasia, and severe dysplasia?
|
Mild/moderate dysplasia - 7-11%
Severe dysplasia - 18% |
|
|
What is the treatment for premalignant laryngeal lesions?
|
Endoscopic excision +/- CO2 laser as needed
Radiation - effective alternative therapy in very elderly, frail, and multifocal lesions. Both surgery and radiation have excellent local control with early lesions. |
|
|
What is the NORMAL tissue histology of the:
Supraglottis - Glottis - Subglottis - |

Supraglottis - ciliated pseudostratified columnar epithelial
Glottis - stratified squamous epithelial Subglottis - ciliated pseudostratified columnar epithelium |
|
|
What is the histology of the follow squamous cell cancers of the larynx:
Well differentiated - Moderately differentiated - Poorly differentiated - |
Well differentiated - keratinization, intercullar bridges, pleomorphic nuclei
Moderately differentiated - less keratinization, more atypical nuclei Poorly differentiated - minimal keratinization, minimal intercellular bridges, numerous atypical nuclei |
|
|
How does supraglottic SCCA typically present? What is the most common subsite involved?
|
Mild odynophagia, dysphagia and referred otalgia via Arnold nerve
Most common subsite involved is the epiglottis |
|
|
What is the typical tumor spread by a supraglottic SCCA?
|
to base of tongue or pre-epiglottic space
|
|
|
What is the incidence of nodal mets to cervical LN at the time of presentation?
|
25-50%
- Typically spreads to level II to IV of th neck; levels I and V are rarely involved |
|
|
What is the incidence of the following T stages for supraglottic SCCA?
T1 T2 T3 T4 |
T1 - 10%
T2 - 29% T3 - 38% T4 - 57% |
|
|
Where is the MOST common site of laryngeal cancer?
|

the glottis
- most in the anterior 2/3rd of true vocal fold |
|
|
What are the typical sx of glottic SCCA?
|
hoarseness and globus sensation
|
|
|
Which cervical levels are involved in glottic SCCA?
|
typically unilateral and in levels II, III, IV and VI
- incidence of cervical mets is low, and is based on T stage |
|
|
How does subglottic SCCA typically present?
|
Can present with airway obstruction, stridor or dyspnea
|
|
|
How common are subglottic SCCA compared to supraglottic and glottic SCCA?
|
Rare, aggressive, and poorly differentiated
|
|
|
Where are the most common areas of hematogenous spread of laryngeal SCCA?
Where are the most common areas of lymphatic spread of laryngeal SCCA? |
Lung > liver > bone
mediastinum |
|
|
What is the mainstay of treatment of early laryngeal cancer (stage I/II)?
|
Mainly tx with single modality - either radiation or surgery - tx is individualized to the pt depending mainly on stage and subsite of laryngeal ca
|
|
|
Stage I/II Early Laryngeal Cancer
What are the advantages and disadvantages of external beam radiation? |
Advantages - useful in nonoperative candidates, avoids up-front tracheotomy in certain patients
Disadvantages - mucositis, laryngeal edema, dysphagia, xerostomia, risk of chondronecrosis, and increased difficulty in detecting recurrence |
|
|
Stage I/II Early Laryngeal Cancer
How long is the entire course of treatment with external beam radiation? |
6-week courses of tx with pts receiving total of 60-70 Gy
|
|
|
Stage I/II Early Laryngeal Cancer
What are the indications for a supraglottic laryngectomy? What are the contraindications? |
Indications:
T1 or T2 with normal vocal cord mobility, tumor limited to supraglottis 2 to 5mm from the anterior commissure Contraindications: Vocal cord fixation, interarytenoid involvement, poor pulmonary status, and thyroid cartilage invasion. |
|
|
Stage I/II Early Laryngeal Cancer
What are the advantages of a supraglottic laryngectomy? What are the contraindications? |
Advantages:
minimal effect on voice, possibility of avoiding irradiation, and appropriate pathologic staging Disadvantages: Applicable to select pts, may require initial tracheotomy, requirement for postoperative swallowing therapy (almost all pts have dysphagia and aspirate postoperatively) |
|
|
Stage I/II Early Laryngeal Cancer
What are the advantages of endoscopic laser excision or microlaryngeal surgery for glottic SCCA? What are the disadvantages? |
Advantages:
possiblity of avoiding irradiation, similar local control as radiation Disadvantages: poorer voice outcomes compared to radiation |
|
|
Stage I/II Early Laryngeal Cancer
What are the indications for endoscopic laser excision or microlaryngeal surgery for glottic SCCA? What are the contraindications? |
Indications:
T1 or T2 lesions with limited involvement of contralateral cord, limited infraglottic extension, and limited involvement of the arytenoids. Of note, preservation of the arytenoids complex results in decreased postop dysphagia and improved vocal outcomes. Contraindications: Vocal cord fixation or bilateral vocal cord impaired motion, interarytenoid involvement, poor pulmonary status, and difficult exposure endoscopically. |
|
|
Stage I/II Early Laryngeal Cancer
How is involvement of the glottic anterior commision addressed? |
Lower locoregional control rates
Surgically best addressed with open procedure such as supracricoid partial laryngectomy with preservation of cricoid and one arytenoid joint. The defect is closed with approximation of base of tongue to laryngeal remnant. |
|
|
Stage I/II Early Laryngeal Cancer
How is an N0 neck managed in Supraglottic and glottic SCCA? |
Supraglottic SCCA - because of the incidence of occult neck disease, the neck should be incorporated into radiation field or the patient should undergo selective neck dissection for N0 neck.
Glottic SCCA - low incidence of occult neck dz; the neck does not need to be tx in clinically N0 cases. |
|
|
What did the RTOG 91-11 study find regarding treatment of laryngeal cancer?
|
Compared nonsurgical tx with induction chemothearpy with radiation, concurrent chemoradiation, and radiation alone.
Stage III or IV patients. Comparable incidence of toxic effects. Laryngectomy free survival and locoregional control better in the concurrent chemoradiation group: 88% at 2 yrs. |
|
|
Which patients with stage III or IV laryngeal cancer are candidates for laryngeal preservation surgery?
|
In select patients with T2 to T4 tumors, supracricoid laryngectomy can be considered. Defect is reconstructed with cricohyoidopexy (CHP) or cricohyoidoepiglottopexy (CHEP) if the epiglottis is spared.
Indications: good pulmonary fnct, limited thyroid cartilage, and epiglottic involvement. Contraindications: involvement of both arytenoid joints, infraglottic extension to cricoid cartilage, invasion of hyoid bone or posterior arytenoid mucosa. |
|
|
What is the primary tx strategy for pts with advanced laryngeal cancer who are NOT candidates for laryngeal preservation surgery?
|
chemotherapy with cisplatin
- applies to most pts with T3 laryngeal cancer |
|
|
When is total laryngectomy performed?
|
In most patients with T4 dz, cartilage invasion, or inability to tolerate chemoradiation, total laryngectomy followed by adjuvant irradiation.
|
|
|
How is the neck managed in pts with Stage III or IV dz?
|
elective tx of neck in clinical No setting recommended in glottic T3 or T4 lesions especially with transglottic involvement. This can be completed with radiation or planned neck dissection with levels II to IV and VI.
With evident neck dz, regardless of site or T shage, comprehensive neck dissection or definitive radiation to the neck is recommended. |
|
|
What is the tx of choice for subglottic laryngeal cancer?
|
Usually presents at advanced stage, so total laryngectomy with adjuvant therapy is the tx of choice.
|
|
|
Which device represents the most reliable technique in voice rehabilitation after total laryngectomy?
|
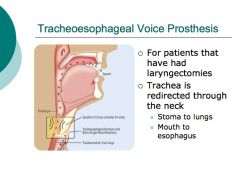
Tracheoesophageal prosthesis.
electrolarynx and esophageal speech are alternatives esophageal speech is difficult to learn. Use of an electrical devise is considered too mechanical sounding by many pt's/ |
|
|
List the major surgical complications of laryngeal cancers
|
Pharyngocutaneous fistula - especially if hx of radiation therapy
Stomal stenosis - could be secondary to stomal recurrence, & may requir pt to wear an appliance such as a laryngectomy tube Dysphagia secondary to pharyngeal stenosis |
|
|
List the major chemoradiation complications of laryngeal cancers
|
Esophageal stenosis - usually secondary to scarring or high-intensity radiotherapy
Nonfunctional larynx - can result from severe local side effects Chondritis - increased risk with biopsy post-chemoradiation tx |
|
|
List the follow up intervals recommended by the NCCN (national comprehensive cancer network).
|
1-3 months for the first year after tx
2-4 months in the second year 4-6 months in third, fourth, and fifth years 6-12 months thereafter should also check thyroid function tests every 6-12 months as there is a 20-65% incidence of hypothyroidism based on tx modality used |
|
|
Recurrences can be salvaged approximately ___% of the time.
|
50%
|
|
|
When is the recommended time to obtain a PET/CT after therapy to see if there is recurrence or mets?
|
10-12 WEEKS after therapy
- if PET/CT is performed sooner after tx, is associated with higher false-positive rate |
|
|
What are the tx modalities for recurrence of laryngeal cancer?
|
Surgery
Reirradiation with or without concurrent chemotherapy - limited by greater risk of side effects Newer anticancer agents - may prolong life, but not a cure Palliative care if cancer incurable |
|
|
Describe verrucous carcinoma
|
A variant of laryngeal squamous cell carcinoma
- 1-2% of laryngeal cancers - exophytic growth of well-differentiated keratinizing epithelium - does not mets unless it has a foci of conventional SCCA - Tx = wide local surgical excision, unless poor candidate; no need for nodal dissection - Radiation therapy generally not required |

