![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
109 Cards in this Set
- Front
- Back
|
The nose develops from ___________ cells
|
neural crest cells
migration of neural crest cells around the 4th week of gestation |
|
|
During development of the nose, what are the 3 potential spaces forming between bone and cartilage?
|
Fonticulus nasofrontalis: space between frontal and nasal bone
Prenasal space: space between nasal bones and nasal capsule Foramen cecum: space between frontal and ethmoid bone |
|
|
During nose development, which membrane separates the nasal and oral cavities?
|
nasobuccal membrane
|
|
|
Anatomy
What are the bones of the nose? |
two paired nasal bones, attaching laterally to the nasal process of maxilla
|
|
|
Anatomy
What are the cartilages of the nose? |
Paired upper lateral cartilages
Paired lower lateral cartilages Accessory sesamoid cartilages |
|
|
Anatomy
What structures make up the nasal septum? |
BONE:
Vomer Palatine bone Perperndicular plate of ethmoid bone Maxillary crest CARTILAGE: Quadrangular cartilage |
|
|
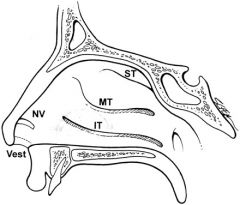
What do the following meati drain?
Inferior meatus: Middle meatus: Superior meatus: |
Inferior meatus: nasolacrimal duct
Middle meatus: maxillary, anterior ethmoid and frontal sinuses Superior meatus: posterior ethmoid sinuses |
|
|
Anatomy
What is the blood supply to the external nose? |
Primary supply from external cartoid artery to facial artery
Superior labial a: columella and lateral nasal wall Angular a: nasal side wall, nasal tip, and nasal dorsum |
|
|
Anatomy
The nasal cavity is supplied by the external and internal carotid arteries. Which external branches? |
External carotid artery system: internal maxillary artery:
- sphenopalatine artery via sphenopalatine foramen: divides into lateral nasal artery, supplying lateral nasal wall; and posterior septal artery, supplying posterior aspect of septum - Descending palatine artery: forms the greater and lesser palatine arteries; supplies lower portion of the nasal cavity - Greater palatine artery: passes inferiorly through greater palatine canal and foramen, travels within hard palate mucosa; bilateral arteries meet in midline and travel through single incisive foramen back into nasal cavity |
|
|
Anatomy
The nasal cavity is supplied by the external and internal carotid arteries. Which internal branches? |
Ophthalmic artery enters orbit and gives off anterior and posterior ethmoid arteries; courses via ant and post ethmoidal canal, takes an intracranial course and then turns inferiorly over the cribriform plate.
- anterior ethmoid artery: supplies lateral and anterior one-third of nasal cavity; anastomoses with sphenopalatine artery (AKA nasopalatine artery; most common artery injuried in septoplasty surgery, causing hematomas) - posterior ethmoid artery: supplies small portion of superior turbinate and posterior septum |
|
|
Anatomy
Which vessels supply Kiesselbach's plexus (Little's area)? |
1) Septal branches of sphenopalatine artery
2) Anterior ethmoidal artery 3) Greater palatine artery 4) Septal branches of superior labial artery |
|
|
Anatomy
Which vessels supply Woodruff's plexus (naso-nasopharyngeal plexus)? |
posterior nasal a.
posterior ethmoid a. sphenopalatine a. ascending pharyngeal a. |
|
|
Anatomy
Where do the following veins drain into? Sphenopalatine vein: Ethmoidal vein: Anterior facial vein: Angular vein: |
Venous system is valveless
Sphenopalatine vein: via sphenopalatine foramen into pterygoid plexus Ethmoidal vein: into superior ophthalmic vein Anterior facial vein: through common facial vein to internal jugular vein; also communicates with cavernous sinus via ophthalmic veins, infraorbital and deep facial veins and the pterygoid plexus Angular vein: drains external nose via ophthalmic vein to cavernous sinus |
|
|
Anatomy
What is the lymphatic drainage of the nose? |
anterior portion of the nose drains toward external nose in the subQ tissue to the facial vein and submandibular nodes
Others pass posterior to tonsillar region and drain into upper deep cervical nodes Most drain into pharyngeal plexus and then to the retropharyngeal nodes |
|
|
Anatomy
Describe the nasociliary nerve, its branches and innervations |
Nasociliary nerve is a branch of ophthalmic division of CN V (CN V1)
Gives off two branches after it enters the orbit: 1) Infratrochlear nerve - supplies skin at the medial angle of eyelid 2) Anterior ethmoidal nerve - leaves orbit with anterior ethmoidal artery; supplies anterior superior nasal cavity, anterior ends of middle and inferior turb and corresponding septum; also region anterior to the superior turb; leaves nasal cavity and supplies skin on dorsum of the tip of nose |
|
|
Anatomy
Describe the maxillary nerve, its branches and innervations |
Maxillary nerve (CN V2) exits middle cranial fossa via foramen rotundum
- Lateral posterior superior nasal branch - posterior portion of superior and middle turbs; post ethmoid cells - Medial posterior superior nasal branch - ant sphenoid, posterior septum and roof of nasal cavity - Nasoplatine nerve - ant hard palate - Greater palatine nerve - inf turb, middle and inferior meatus Infraorbital branch - supplies portion of vestibule of the nose; anterior portion of inferior meatus; part of floor of nasal cavity |
|
|
Anatomy
What are the preganglionic nerves of the pterygopalatine ganglion? |
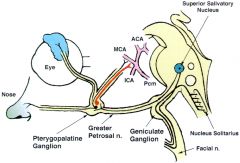
The autonomic innervation of the nose is derived from the pterygopalatine/sphenopalatine ganglion
Preganglionic fibers of the nose are originate from the superior salivatory nucleus in the medulla oblongata --> CN VII --> ggreater superficial petrosal nerve at the geniculate ganglion --> vidian nerve --> pterygopalatine ganglion |
|
|
Anatomy
What are the postganglionic nerves of the pterygopalatine ganglion? |
The autonomic innervation of the nose is derived from the pterygopalatine/sphenopalatine ganglion
Arise in ganglion and join sympathetic and sensory fibers Travel with branches of sphenopalatine nerve and provide secretomotor fibers to mucous glands in nasal mucosa & lacrimal glands Cause vasodilation |
|
|
Anatomy
What are the sympathetic fibers of the nose? |
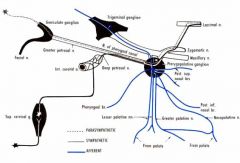
From thoracic spinal nerve (T1-T3)
Postganglionic fibers from superior cervical ganglion and travel with the ICA Leave this plexus as deep petrosal nerve and join the greater superficial petrosal nerve to form vidian nerve (nerve of pterygoid canal) Causes vasoconstriction |
|
|
Anatomy
What is the histology of the nasal vestibule? |
Keratinized squamous epithelium with vibrissae, sweat and sebaceous glands
|
|
|
Anatomy
What is the histology of the anterior 1/3 of nasal cavity & anterior portions of inferior and middle turbs? |
squamous and transitional cell epithelium
|
|
|
Anatomy
What is the histology of the posterior nasal cavity? |
Pseudostratified columnar epithelium
|
|
|
Anatomy
Describe the layers of the mucous blanket |
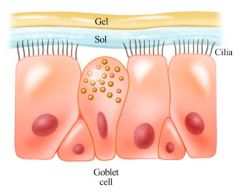
Two layers: gel and sol phase
Gel phase: superficial layer, produced by goblet and submucosal glands; traps particulate matter Sol phase: deep layer, produced by microvilli; provides fluid that facilitates ciliary movement Other components: mucoglycoproteins, immunoglobulins, interferon and inflammatory cells |
|
|
Describe the two physiologic nasal reflexes?
|
Nasal reflexes - multiple that causes periodic nasal congestion, rhinorrhea or sneezing
Postural reflex - increased congestion with supine position; congestion on the side of dependence upon lying on the side Hot or cold temperature reflex - sneezing upon sudden exposure of skin to dramatic temperature extremes |
|
|
List the functions of the nose
|
Airway: conduit for air
Filtration: trap and remove airborne particulate matter Humidification: increases relative humidity Heating: provides radiant heat of inspired air Nasal reflexes: postural, and hot or cold temp reflexes Chemosensation: detects irritants and temp changes Olfaction |
|
|
Describe the change in nasal airflow resistance throughout the day
|
Cycle occurring every 2-7 hours
Mucosal vasculature is under sympathetic tone - when tone DECREASES = vessels engorge = increased airflow resistance |
|
|
What are the 3 regions of nasal resistance?
|
nasal vestibule
nasal valve nasal cavum |
|
|
What are the 3 borders of the nasal valve?
|
Nasal valve is the narrowest point of nasal airway resistance
Borders: lower edge of upper lateral cartilage, anterior end of inferior turbinates, and nasal septum |
|
|
Where are the various locations of olfactory epithelium?
|
Located in upper edge of nasal chamber adjacent to cribriform plates
Superior nasal septum Superior lateral nasal wall |
|
|
What are the two layers of the olfactory epithelium?
|
Olfactory mucosa
Lamina propria |
|
|
Congenital Anomalies
What are the four basic theories of choanal atresia? |
1) Persistence of buccopharyngeal membrane
2) Abnormal persistence of bucconasal membrane 3) Abnormal mesoderm forming adhesions in nasochoanal region 4) Misdirection of neural crest cell migration |
|
|
Congenital Anomalies
What percentage of pt's with choanal atresia also have other associated congenital anomalies? |
20-50%
|
|
|
Congenital Anomalies
What congenital anomalies are associated with choanal atresia? |
CHARGE (coloboma, heart dz, MR, genital hypoplasia, ear anomalies)
Apert syndrome, Crouzon dz, Treacher-Collins syndrome |
|
|
Congenital Anomalies
What is the timing of presentation between unilateral and bilateral choanal atresia? |
Bilateral - presents in newborn with airway distress at birth since newborns are obligate nasal breathers; classic presentation is cyclic cyanosis relieved by crying (paradoxical cyanosis)
Unilateral - presents between 5-24mo with unilateral obstruction and nasal discharge |
|
|
Congenital Anomalies
What are the treatments for choanal atresia? |
Bilateral = immediate management - airway stabilization with oral airway, McGovern nipple
Surgical approaches = tranpalatal, transnasal, endoscopic |
|
|
Congenital Anomalies
List the thee congenital midline nasal masses |
Dermoid sinus cyst (most common)
Glioma Encephalocele Tx of all is surgical excision |
|
|
Congenital Anomalies
What is the presentation of a dermoid sinus cyst? |

Present as a midline nasal pit, fistula, or infected mass located anywhere from the glabella to the nasal columella. May present as intranasal, intracranial or extranasal masses along the nasal dorsum
Mass is nontender, noncompressible, and firm; do not transilluminate |
|
|
Congenital Anomalies
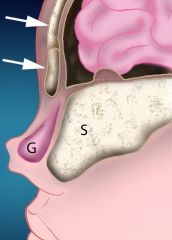
What is the pathophysiology behind dermoid nasal cysts? |
During development, projection of dura protrudes through fonticulus frontalis or inferiorly into prenasal space; the projetion normal regresses and if it does not, the dura can remain attached to the epidermis, causing trapping of ectodermal elements
Have a tendency for repeated infections Tx - surgical excision of entire cyst & tract; I&D is discouraged |
|
|
Congenital Anomalies
What is the presentation of a nasal glioma? |
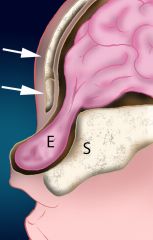
Gliomas are made of neuroglial elements consisting of glial cells in a connective tissue matrix with or without a fibrous connection to the dura. Abnormal closure of the fonticulus frontalis can lead to an ectopic rest of glial tissue .
There is no fluid filled space connected to the subarachnoid space. These lesions usually present as a red or bluish lump at or along the nasomaxillary suture, or as an intranasal mass. They are characteristically firm, noncompressible, do not increase in size with crying, and do not transilluminate. The overlying skin may have telangiectasias. They can be associated with a widened nose or with hypertelorism secondary to growth of the mass. Intranasal gliomas most often arise from the lateral wall of the nose or less often from the nasal septum. 60% are extranasal, 30% intranasal, and 10% are both. Overall, 15% are connected to the dura. The intranasal type is more often associated with dural attachment (35%) than the extranasal type (9%). They are more common in males by a 3:1 ratio although the significance of this has not been established. Tx: surgical excision |
|
|
Congenital Anomalies
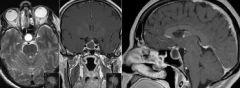
What is the presentation of an encephalocele? |
Encephalocele is a congenital herniation of the CNS tissue through skull base defects; either meningocele (meninges only) or meningoencephaloceles (meninges + glial tissue)
Mass is often bluish or red, soft, compressible and TRANSilluminates; pulsatile and expands with crying or straining |
|
|
Congenital Anomalies
What is a positive Furstenberg test? |
nasal mass expands with compression of internal jugular veins = encephalocele
|
|
|
Congenital Anomalies
Where are the locations of encephaloceles? |
Occipital (most common - 75%)
Sincipital - also called frontoethmoidal encephaloceles, with defect at foramen cecum, just anterior to cribriform plate Basal - defect in floor of anterior cranial fossa between cribriform plate and clinoid process |
|
|
Congenital Anomalies
What are the subtypes of sincipital encephaloceles? |
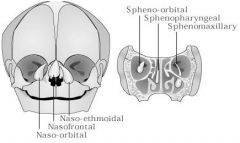
Sincipital encephaloceles AKA frontoethmoidal encephaloceles
Present as an external mass over nose, glabella or forehead Subtypes: 1) Nasofrontal 2) Nasoethmoidal 3) Naso-orbital |
|
|
Congenital Anomalies
What are the subtypes of basal encephaloceles? |
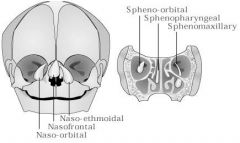
Present as internal intranasal or nasopharyngeal mass
Subtypes: 1) Transethmoidal 2) Trans-sphenoidal 3) Sphenoethmoidal 4) Sphenomaxillary |
|
|
Head and neck teratomas account for what percentage of all teratomas?
|
2-3%
|
|
|
What is the most common site for a head & neck teratoma?
|

Cervical teratoma, followed by nasopharyngeal teratoma
|
|
|
Describe the location and presentation of Rathke's Pouch Cyst
|
Rathke's pouch is an invagination of the nasopharyngeal epithelium in the posterior midline; the anterior pituitary gland develops from this in fetal life.
Remnants of this pouch may persist forming a cyst or tumor Rathke's pouch cyst: 1) Bening cyst in the sella turcica 2) Usually assx but may cause mass effect on pituitary gland or optic chiasm 3) Usually present in 5th or 6th decade of life; F > M 4) MRI is modality of choice Tumor of Rathke's pouch = craniopharyngioma |
|
|
Describe the presentation of Thornwaldt's Cyst
|

Benign nasopharyngeal cyst
Develops from remnant of notochord Sx: postnasal drip, haliotosis, aural fullness, serous otitis media, and cervical pain Examination: smooth submucosal midline mass in nasopharynx Tx: none if assx; if sx, marsupialization through surgical correction via endoscopic approach |
|
|
Describe the presentation of Intra-Adenoidal Cysts
|
Occlusion of adenoid crypts, leading to retention cysts in adenoids
Asymptomatic Present in midline, rhomboid shape on imaging |
|
|
Which branchial arches form a branchial cleft cyst?
|
first or second branchial arches
|
|
|
Explain the sensitization phenomenon in allergic rhinitis
|
Initial exposure to antigen causes antigen-processing cells (macs & dendritic cells) present the processed peptides to T-helper cells.
Upon subsequent exposure to the same Ag, these cells are stimulated to diffentiated into more T-helper cells or B cells. B cells further differentiate into plasma cells and produce IgE specific to that Ag. Allergen-specific IgE molecules then bind to the surface of mast cells, sensitizing them. |
|
|
Explain the early and phase responses in allergic rhinitis, including symptoms
|
Early phase response - starts within 5-15min
- mast cells degranulate, releasing histamine, heparin and tryptase - degranulation also triggers formation of prostaglandin PGD2, leukotrienes LTC4, LTD4, LTE4 and platelet activating factor (PAF) - Sx - sneezing, rhinorrhea, congestion and pruritis Late phase response - starts 2-4hrs later - caused by newly arrived inflammatory cells recruited by cytokines - EOS, neutrophils and basophils prolong the earlier reactions and lead to chronic inflammation |
|
|
How do you differentiate allergic vs nonallergic rhinitis?
|
Nonallergic has same sx as allergic rhinitis except for nasal and ocular pruritis
|
|
|
What are the possible triggers for nonallergic rhinitis?
|
strong fragrances
tobacco smoke changes in temperature cleaning products |
|
|
What are the various classifications of nonallergic rhinitis?
|
1) Infectious rhinitis
2) Vasomotor rhinitis 3) Hormonal rhinitis 4) Occupational rhinitis 5) Drug-induced rhinitis 6) Rhinitis medicamentosa 7) Gustatory rhinitis 8) Nonallergic rhinitis of eosinophilia syndrome (NARES) |
|
|
What is the pathophysiology of vasomotor rhinitis?
|
Predominance of the parasympathetic system leading to vasodilation and mucosal edema.
Cold air and strong odors exacerbate sx |
|
|
Which drugs are responsible for drug-induced nonallergic rhinitis?
|
Antihypertensives: ACEI and beta blockers
NSAIDS Oral contraceptives |
|
|
What is the pathophysiology of gustatory rhinitis?
|
Watery rhinorrhea due to vasodilation after eating, especially with spicy or hot foods
|
|
|
What are the Sx of nonallergic rhinitis of eosinophilia syndrome (NARES)?
|
Rhinitis with approximately 10-20% EOS on nasal smears
Sx of nasal congestion, rhinorrhea, sneezing, pruritis, and hyposmia |
|
|
Discuss the cause and sx of atrophic rhinitis
|
AKA Rhinitis Sicca or Ozena
Mucosal colonization with klebsiella ozaenae and other organisms Nasal mucosa degenerates and loses mucociliary fnct May be either primary or secondary (ie. d/t trauma or nasal surgery (empty nose syndrome)) Presentation - foul smell as well as yellow or green nasal crusting with atrophy and fibrosis of mucosa |
|
|
What is the triad of Wegener's Granulomatosis?
|
Triad:
1) Necrotizing granulomas of respiratory tract 2) Vasculitis 3) Glomerulonephritis |
|
|
What are the nasal presentations of Wegener's Granulomatosis and what are the diagnostic studies?
|
Sinonasal sx usually manifest early with severe nasal crusting, epistaxis, rhinorrhea and secondary rhinosinusitis
+cANCA +anti-Myeloperoxidase and anti-Proteinase 3 Tx: saline irrigation, nasal moisturization and topical Abx |
|
|
What are the nasal presentations of sarcoidosis?
|
Multisystem inflammatory dz with noncaseating granulomas
Sinonasal manifestations: nasal obstruction, postnasal drainage, recurrent sinusitis Serum ACE levels may be elevated |
|
|
Describe the general facts of rhinoscleroma
|
Chronic granulomatous dz due to Klebsiella rhinoscleromatis
Endemic to Africa, central America, or Southeast Asia Usually affects nasal cavity, but may also affect the larynx, nasopharynx, or paranasal sinuses |
|
|
What are the three stages of rhinoscleroma dz progression?
How do you tx the dz? |

1) Catarrhal or atrophic: rhinitis, purulent rhinorrhea, and nasal crusting
2) Granulomatous or hypertrophic: small painless granulomatous lesions in upper respiratory tract that block nasal passages 3) Sclerotic: sclerosis and fibrosis narrowing nasal passages Tx - long-term Abx, biopsy, debridement |
|
|
What are two histologic findings of rhinoscleroma?
|

1) Mikulicz cells: large macrophage with clear cytoplasm containing bacilli
2) Russel bodies in plasma cells (large eosinophilic inclusions) |
|
|
Describe the general facts about rhinosporidiosis, sx, histopathology and tx
|

Rhinosporidiosis is a chronic granulomatous infection caused by Rhinosporidium seeberi
Endemic to Africa, Pakistan, Sri Lanka, or India Sx - friable red nasal polyps, nasal obstruction, and epistaxis Histiopathology - pseudoepitheliomatous hyperplasia, presence of R. seeberi Tx - surgical excision |
|
|
Epistaxis
How is an IMAX ligation performed? |
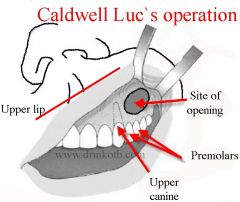
Caldwell-Luc to enter maxillary sinus
Enter posterior wall, vessels clipped |
|
|
Epistaxis
How is an endoscopic sphenopalatine ligation performed? |
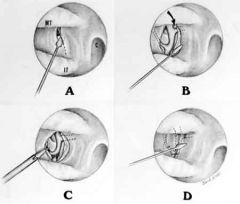
- Follow middle turb to posterior aspect
- Make vertical incision approximately 7-8mm anterior to the posterior end of middle turbinate - Crista ethmoidalis seen and marks anterior sphenopalatine foramen; vessels are posterosuperior to this - Clip or cauterize vessels at this site and replace flap |
|
|
What are the sx of rhinosinusitis?
|
Symptoms (2 or more)
A) one of which should be nasal blockage or obstruction or congestion or nasal discharge (anterior OR posterior nasal drip) B) +/- facial pain or pressure C) +/- hyposmia or anosmia |
|
|
What are the five classifications of rhinosinusitis?
|
1) Acute RS (ARS) - Sx lasting <4 weeks with complete resolution
2) Subacute RS - Sx lasting between 4-12 weeks 3) Chronic RS (CRS) with OR w/o polyps - sx lasting >12 weeks w/o complete resolution of sx 4) Recurrent ARS - 4 or more episodes per year, each lasting >7-10 days WITH complete resolution in between episodes 5) Acute exacerbation of CRS - sudden worsening of baseline CRS with return to baseline after tx |
|
|
Acute Rhinosinusitis
What are the most common agents in acute viral rhinosinusitis? |
rhinovirus and influenzae
Sx lasts <14 days |
|
|
Acute Rhinosinusitis
What are the three cardinal sx for diagnosis of acute bacterial rhinosinusitis? |
1) Purulent nasal discharge
2) Face pain or pressure 3) Nasal obstruction +/- anosmia, fever, aural fullness, cough, and headache |
|
|
Acute Rhinosinusitis
What is the pathophysiology of acute rhinosinusitis? |
Anatomic abnormalities may predispose on to ARS: septal deviation and spur, turbinate hypertrophy, prominent ethmoidal bulla, concha bullosa, pneumatization and inversion of uncinate process.
Acute viral resp infection affects nasal and sinus mucosa leading to obstruction of sinus outflow Other factors: allergies, nasal packing, sinonasal tumors, trauma and dental infections |
|
|
Chronic Rhinosinusitis
What are the four cardinal sx of CRS? |
1) Anterior or posterior purulent nasal drainage
2) Nasal obstruction 3) Face pain or pressure 4) Hyposmia or anosmia |
|
|
What are the criteria to make a diagnosis of CRS?
|
At least two of the four cardinal sx + ONE of the following?
1) Endoscopic evidence of mucosal inflammation: purulent mucus or edema in middle meatus or ethmoid region 2) Polyps in nasal cavity or middle meatus 3) Radiologic evidence of mucosal inflammation |
|
|
What are the 3 subtypes of chronic rhinosinusitis?
|
1) CRS with polyps
2) CRS w/o polyps (mc type, 60-65%) 3) Allergic fungal rhinosinusitis |
|
|
What are the five criteria of Bent & Kuhn for allergic fungal rhinosinusitis?
|
1) Eosinophilic mucin (Charcot-Leyden crystals)
2) Noninvasive fungal hyphae 3) Nasal polyposis 4) Characteristic radiologic findings 5) Type 1 hypersensitivity by history, skin tests or serology |
|
|
What are the characteristic CT & MRI radiologic findings of allergic fungal rhinosinusitis?
|
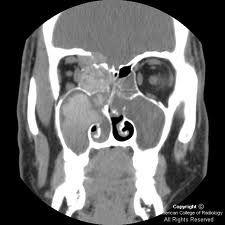
CT findings
1) rim of hypointensity with hyperdense central material (allergic mucin) 2) speckled areas of increased attenuation due to ferromagnetic fungal elements MRI findings 1) peripheral hyperintensity with central hypointensity on both T1 and T2 2) central "void" on T2 |
|
|
What are the typical agents responsible for allergic fungal rhinosinusitis?
|
Dematiaceous fungi (alternaria, bipolaris, curvularia, cladosporium, dreschlera)
|
|
|
Is allergic fungal rhinosinusitis typically unilateral or bilateral?
|
unilateral
|
|
|
Allergic fungal rhinosinusitis has a high association with which disease process?
|
asthma
|
|
|
Up to ___% of CRS pt's have asthma
|
50%
|
|
|
Explain staphylococcal superantigens and their role in CRS
|
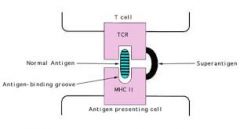
Staph superantigen is an exotoxin secreted by certain S. aureus strains; they activate T cells by linking T-cell receptors with MHC II surface molecule on antigen presenting cells (APC's)
|
|
|
Explain which granulomatous vasculitis may cause CRS?
|
Churg-Strauss syndrome: CRSwNP, asthma, peripheral eosinophilia, pulmonary infiltrates, systemic eosinophilic vasculitis, and peripheral neuropathy
|
|
|
What are the two main categories of fungal rhinosinusitis (nonallergic)
|
Invasive & noninvasive
|
|
|
What are the three types of invasive fungal rhinosinusitis?
|
acute invasive (aka acute fulminant fungal rhinosinusitis)
chronic invasive chronic granulomatous |
|
|
What are the three types of noninvasive fungal rhinosinusitis?
|
sinus fungal ball
saprophytic fungal infestation (SFI) allergic fungal rhinosinusitis |
|
|
Noninvasive Fungal Rhinosinusitis
Sinus fungal ball is usually bilateral or unilateral? What is the most common fungal agent? |

unilateral
Aspergillus fumigates |
|
|
Noninvasive Fungal Rhinosinusitis
Does sinus fungal ball typically present in immunocompromised or immunocompetent pt's? What is the tx? |
Immunocompetent pt's
surgical removal |
|
|
Invasive Fungal Rhinosinusitis
What are the sx of acute invasive fungal rhinosinusitis? |
Nasal painless ulcer or eschar
Periorbital or facial swelling Ophthalmoplegia |
|
|
Invasive Fungal Rhinosinusitis
Does acute invasive fungal rhinosinusitis affect immunocompromised or immunocompitent pt's? |
Immunocompromised
|
|
|
Invasive Fungal Rhinosinusitis
Which organisms are involved in acute invasive fungal rhinosinusitis? |
Septate - Aspergillus, 45* branching
Nonseptate - Mucorales (Rhizopus, Rhizomucor, Absidia, Mucor, Cunninghamella, Mortierella, Saksenaea, Aopohysomyces, and Zygomycosis). 90* branching, necrotic background, serpiginous (Most common in DKA pt's) |
|
|
Invasive Fungal Rhinosinusitis
What is the tx for acute invasive fungal rhinosinusitis? |
aggressive surgical debridement
systemic antifungals correct underlying immunosuppressed states (poor prognosis) |
|
|
Invasive Fungal Rhinosinusitis
Which species are involved in chronic invasive fungal rhinosinusitis? |
Aspergillus fumigates common
Mucor Alternaria Curvularia Bipolaris Candida Drechslera |
|
|
Invasive Fungal Rhinosinusitis
Does chronic invasive fungal rhinosinusitis affect immunocompromised or immunocompetent pt's? |
immunocompetent pts
|
|
|
Invasive Fungal Rhinosinusitis
What is the pathogenesis of chronic invasive fungal rhinosinusitis? |
Tissue invasion by fungal elements >4wks with minimal inflammatory responses
|
|
|
Invasive Fungal Rhinosinusitis
What is the tx for chronic invasive fungal rhinosinusitis? |
Surgical debridement
Systemic antifungals (poor prognosis) |
|
|
Invasive Fungal Rhinosinusitis
What is the pathogenesis of chronic granulomatous fungal rhinosinusitis? |
Tissue invasion by fungal elements >4wks with inflammatory responses (remember, chronic invasive has minimal inflammatory response)
Multinucleated giant cell granulomas centered on eosinophilic materal surrounded by fungus |
|
|
Invasive Fungal Rhinosinusitis
Does chronic granulomatous fungal rhinosinusitis affect immunocompromised or immunocompetent pt's? |
immunocompetent pts
|
|
|
Invasive Fungal Rhinosinusitis
Which species are involved in chronic granulomatous fungal rhinosinusitis? |
Aspergillus flavus
|
|
|
What are the various ways that rhinosinusitis can spread and cause complications?
|
Hematogenous spread: retrograde thrombophlebitis through valveless veins (veins of Breschet)
Direct spread: through lamina papyracea, osteomyelitis |
|
|
What are mucoceles and what is the tx?
|
- Collection of sinus secretions trapped due to obstruction of sinus outflow tract; expansile process
- Mucopyoceles: infected mucocele Tx - endoscopic marsupialization |
|
|
What are some ophthalmologic complications of rhinosinusisits?
What are the Chandler's classifications? |
Chandler's classifications
1) Preseptal cellulitis: inflammatory edema; no limitation of extraocular movements (EOM) 2) Orbital cellulitis: chemosis, impairment of EOM, proptosis, possible visual impairment 3) Subperiosteal abscess: pus collection between medial periorbita and bone; chemosis, exophthalmos, EOM impaired, visual impairment worsening 4) Orbital abscess: pus collection in orbital tissue; complete ophthalmoplegia with severe visual impairement - Sup. orbital fissure syndrome (CN 3, 4, V1, 6) - Orbital apex syndrome (CN 2, 3, 4, V1, 6) 5) Cavernous sinus thrombosis: bilateral ocular sx |
|
|
List 4 neurologic complications of rhinosinusitis
|
1) Meningitis
2) Epidural abscess 3) Subdural abscess 4) Brain abscess |
|
|
List 2 bony complications of rhinosinusitis
|
1) Osteomyelitis: thrombophlebitic spread via diploic veins
2) Pott's puffy tumor: subperiosteal abscess (frontal bone osteomyelitis to erosion of the anterior bony table) |
|
|
You placed a pt with acute rhinosinusitis on Abx. How many days after starting tx would you want to change the ABx if there has been to improvement?
|
72 hours after starting Abx
|
|
|
What is the recommended medical tx of CRS without nasal polyps?
|
1) Long-term oral Abx (>12 wks), usually macrolide
2) Topical nasal steroids 3) Nasal saline irrigation |
|
|
What is the recommended medical tx of CRS with nasal polyps?
|
1) Topical nasal corticosteroids (drops better than sprays)
2) Systemic corticosteroids: 1mg/kg initial dose and taper over 10 days 3) Nasal irrigations Long-term oral Abx 4) long-term oral Abx (>12wks), usually macrolide |

