![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
A calyceal fistula in a renal allograft is most frequently associated with what?
|
*Calyceal fistulae are an uncommon cause of urinary tract fistulae in renal transplants. They are more commonly seen in allografts with multiple renal arterires. They are usually caused by segmental renal infarction secondary to occlusion of a renal artery branch.
|
|
|
What are indications for pre-transplant native nephrectomy?
|
*Severe proteinuria, renal calculi, polycystic kidneys that are causing problems such as lack of space, infections, hemmorhage, hypertension that is not controlled by dialysis or medications.
|
|
|
Is the risk of CIC higher in transplant patients than other classes of patients performing CIC?
|
*According to SASP it is not and they can do CIC.
|
|
|
What is the most common cause of ESRD in the US?
|
*DM is the first, HTN and glumerulonephritis are after that. Of note HTN is dispraportionately higher in african americans.
|
|
|
What is permanent renal failure in the United States?
|
* The definition may vary but our text states that it is an irreversible loss of GFR to less than 10ml/min or a serum creatinine greater than 8.
|
|
|
What is more cost effective dialysis or renal transplantation?
|
*Renal transplantation and so the goal for patients on HD is renal transplantation for all patients that have less of a risk for being transplanted than being on HD and it is a better or cheaper than HD.
|
|
|
Are most patients with ESRD on HD or PD?
|
*Most patients are on HD.
|
|
|
Why would a patient be on peritoneal dialysis as opposed to hemodialysis?
|
*Long distance from a HD unit, desire for self care, difficulties with HD, serious cardiac disease, DM, patients with short stature.
*As opposed to this patients that are poor candidates are poor hygeine, obesity, inflammatory bowel disease, and obliterated peritoneal space. |
|
|
What are some special problems with children that have ESRD?
|
*Poor growth, short stature, poor nutritional status, and psychiatric problems.
|
|
|
What are the main reasons that patients on HD die?
|
*first is heart disease, then stroke, then sepsis.
|
|
|
What was the example of the first attempted organ transplant?
|
*The recipient was a 26 year old female that attempted to commit suicide and was tranpslanted a kidney to the femoral vessels with a cutaneous ureterostomy. She made urine for a short time and then died.
|
|
|
What patients should be counseled about graft failure and disease recurrence?
|
*primary oxalosis, focal segmental glomerulosclerosis, and hemolytic-uremic syndrome.
*For patients with hemolytic uremic syndrome they should undergo a combined renal and liver transplant. |
|
|
Does autosomal dominant polycystic kidney disease recur in a transplant kidney?
|
*No
|
|
|
Why do transplant teams freak out about infections before transplant?
|
*You are going to put these patients on immunosupression and so you want to make sure there are no active infections before transplanting the patients
|
|
|
So if a patient has had cancer are they able to get a transplant?
|
To reduce the risk of cancer recurrence a waiting time of 2-5 years is generally needed before transplant, however the book states that the wait times can be less if patients had low grade low risk cancers.
|
|
|
What is the basic goal of urologic evaluation before a renal transplantation?
|
*You want to make sure that the bladder is going to behave and whether or not the native kidneys need to be removed.
|
|
|
Can you use a defunctionalized bladder for a transplant?
|
*Yes, the bladder will usually become functionally again after the transplant. This is apparently true for most children I am not sure about all adults. If there is concern for significant fibrosis then the patient can have augemntation cystoplasty. This may need to be done after transplant or can be done before.
|
|
|
Is CIC safe for kidney transplant patients?
|
*Yes, it has been done for decades without issue.
|
|
|
Can you perform a transplant into a conduit or continent intestinal diversion?
|
Yes it has been done succesfully.
|
|
|
If you need to do an anti-obstructive procedure such as a TURP on an anuric or oliguric patient whoe needs a transplant do you perform it before or after?
|
*After because you don't want to do that on a dry bed.....very bad.
|
|
|
Sometimes we will say that if a kidney is very large it might be removed before a renal transplant to make room for the tranpslant, how big?
|
The book states that if a kidney extends down below the iliac crest it is best to remove it to make room for the transplant kidney.
|
|
|
What are indications for pre-transplant nephrectomy?
|
*stones that are not amenable to minimally invasive techniques.
*Renal mass *Persistant anti-glomerular basement membrane antibody levels *Recurrent pyelonephritis *Severe hydronephrosis |
|
|
What are the causes of ED in ESRD patients?
|
*Accelerated arteriosclerosis that is associated with dialysis
*Hyperprolactinemia with its associated hypogonadism *Poor self image |
|
|
What are the basic criteria for a renal donor?
|
free from renal disease, free from transmissable malignancy, and free from malignancy
|
|
|
Are ABO incompatibility and a positive lymphocyte to recipient serum test contraindications to transplant?
|
*they used to be but now there are regimens for immunosupression that can deal with these issues if need be.
|
|
|
Can patients with HIV receive an organ transplant?
|
The answer used to be no, but if a patient has low viral loads and high CD4 counts then they can and have successfully undergone transplants
|
|
|
If you have a woman kidney donor and all other things are equal which kidney would you choose?
|
The right kidney as this is the one more likely to develop hydronephrosis during pregnancy and this can be even more cause for concern with a solitary kidney.
|
|
|
What is the imaging modality of choice for renal transplant patients when considering them for surgery?
|
CT angiography with and without contrast of the abdomen and pelvis with delayed phase imaging. This helps you to identify the renal anatomy and the pelvic vascular anatomy as well as the presence or absence of stones and the anatomy of the renal collecting system
|
|
|
Is open donor nephrectomy or lap donor nephrectomy better?
|
Randomized controlled clinical trials are ongoing and appear to show that the results are equivalent.
|
|
|
What are the criteria for ideal donor kidney patient in a deceased patient?
|
The ideal candidate as no hypertension, no active malignancy except for possibly a primary brain tumor or superficial skin cancer that has been treated, no diabetes, normal renal function, no evidence of infection, age between 6 and 50 years old. If the patient has been in the hospital for greater than 2-3 days then blood cultures are drawn.
|
|
|
In a patient that is defined as brain dead and you are trying to maintain an adequate CV parameters for transplant, what are your goals?
|
*SBP>90 or MAPs>60
*UOP > 0.5cc/kg/hr *If UOP goal cannot be achieved and CVPs are elevated then the patient can be placed on low dose dopamine or dobutamine. |
|
|
Which anastomosis should be done first with the transplant the renal artery or the renal vein?
|
The renal artery anastomosis should be done first and then the renal vein because the artery is the more critical of the two anastomoses, the kidney is not tethered by the venous anastomosis and venous occlusion can be delayed until after the renal artery anastomosis.
|
|
|
What is warm ischemia injury of a transplant secondary to?
|
ailure of oxidative phosphorylation and cell death due to ATP depletion. The Na-K pump is impaired and NaCl and water passively diffuse into the cells causing cellular swelling.
|
|
|
What is the most commonly used solution to bathe the transplant kidney?
|
UW solution- lactobionate, raffinose and hydroxyethyl starch which all minimize cellular swelling. Phosphate is used for its buffering ability and adenosine for ATP synthesis during reperfusion. Studies have confirmed its superiority as the best solution and can be used for any organ.
|
|
|
Is there good evidence that supports the use of a ureteral stent at the time of renal transplantation? When is it removed?
|
Yes. Placing a stent has been shown to reduce the incidence of ureteral complications.
Remove in 6-12 weeks after transplant. |
|
|
If you’re using the internal iliac artery for the transplant anastomosis and this fails, can you use the contralateral internal iliac artery? Why or why not?
|
You cannot because this will knock off the cavernosal arteries and ED will result.
|
|
|
Where is the transplant kidney usually placed? Any exceptions?
|
Contralateral iliac fossa w/ rectus-preserving Gibson incision
Obese: easier to place in right iliac fossa because of more superficial iliac veins Pancreas simultaneous transplant: Place left kidney with its longer renal vein in left iliac fossa Child with large transplant: Place on right side which allows access to wider choice of arteries and veins for vascular reconstruction |
|
|
How is the implantation of the ureter into a patient with an ileal conduit different?
|
Basically the anastomosis is the exact same as you would make for a ureteroneocystostomy.
You should irrigate the pouch with antibiotic solution as well as irrigate it free of mucus and choose the best site for the placement of the transplant kidney with the pouch full. The kidney can also be placed upside down so as to allow the ureter to be facing up towards the conduit to prevent ureteral kinking |
|
|
Let’s say that you are doing a transplant on a patient and you are using EDC (extended donor criteria) and considering using transplant kidneys that have an elevated creatinine, what options do you have?
|
You can transplant both kidneys into each of the iliac fossas
You can transplant each kidney into the same iliac fossa, with one anastomosis to the IVC and aorta and the other to the external iliac vessels. |
|
|
Post-operatively, what is the usual IVF rate and type of solution for a renal transplant?
|
D51/2NS to replace insensible losses & 1/2NS to match the urine output
|
|
|
Why is ABO compatibility so important? Is there a way around this?
|
We all have antibodies to the ABO groups that we don’t possess and these antigens are present on endothelial cells. This will cause the incompatible patient to attack the graft vasculature and cause rejection.
As alluded to earlier with plasmapheresis (removing the already pre-formed antibodies), marked immunosuppression at the time of grafting, use of Rituximab, as well as +/- splenectomy to reduce antibody production you can transplant across ABO groups. |
|
|
What are the MHC antigens? What are the two major classes?
|
Glycoproteins that are present on the surface of cells.
There are two major classes the HLA-A, HLA-B, HLA-C group are present on nearly all nucleated cells and are from the MHC gene on chromosome 6. The second group is HLA-DR, HLA-DQ, and HLA-DP. These are present on B lymphocytes, T lymphocytes, dendiritic cells, macrophages, etc. |
|
|
What is the difference between hyperacute, accelerated, acute, and chronic rejection?
|
Hyperacute rejection - occurs immediately after renal revascularization. It is an irreversible process mediated by preformed circulating cytotoxic antibodies that develop after pregnancy, blood transfusions, or an earlier failed transplantation. It is very rare when the crossmatch between recipient serum and donor lymphocytes is negative.
Accelerated rejection - is mediated by humoral and cellular components of the immune response. It occurs within days to weeks and often does not respond to anti-rejection therapy. Acute rejection - can occur any time after transplantation. The symptoms of acute kidney transplant rejection are those of “the flu,” accompanied by pain over an enlarged kidney graft, hypertension, decreased urinary output, fluid retention, increased serum creatinine levels, and radioisotope renography indicating decreased renal blood flow, glomerular filtration, and tubular function. Acute pyelonephritis must be ruled out by urinalysis and, subsequently, negative urine culture. Needle biopsy of the kidney graft is the standard to confirm the diagnosis of acute rejection. The typical histologic findings of acute renal allograft rejection are mononuclear cellular infiltration, tubulitis, and vasculitis. Chronic rejection - is characterized by a gradual decline in renal function associated with interstitial fibrosis, vascular changes, and minimal mononuclear cell infiltration. A positive B-cell crossmatch or a positive flow crossmatch against donor B or T cells is considered by some to be predictive of chronic rejection and poorer long-term graft survival. |
|
|
What is conventional treatment for acute renal allograft rejection?
|
High dose pulse corticosteroids
If corticosteroids fail, then use antilymphocyte antibodies |
|
|
Provide the general mechanisms for each of these mentioned immunosuppressants, and their main organ system toxicities.
|
Tacrolimus:
Inhibits calcineurin & IL-2 production CNS,GI, kidney, endocrine Cyclosporine: Inhibits calcineurin & IL-2 production CNS,GI, kidney, skin, endocrine, dysplipidemia Azathioprine: Inhibits purine synthesis GI, Hematopoietic Mycophenolate mofetil: Inhibits purine synthesis GI, hematopoietic Glucocorticoids: Reduces transcription of cytokine genes CNS, GI, Skin, endocrine, dyslipidemia, wound healing Sirolimus: Inhibits cell cycle progression Hematopoietic, endocrine, dyslipidemia, wound healing Rabbit & equine antithymocyte globulin: Depletes T lymphocytes Rituximab: Depletes B lymphocytes Basiliximab and daclizumab: Blocks IL-2 receptor |
|
|
What are common reasons for early graft dysfunction?
|
Infection
Allograft rejection Urinary or vascular obstruction Cyclosporine or tracrolimus nephrotoxicity Dehydration Hyperglycemia |
|
|
What is the initial treatment of choice for transplant renal artery stenosis?
|
Percutaneous transluminal angioplasty w/ or w/o endoluminal stent.
|
|
|
What are indications for allograft nephrectomy?
|
Remove a symptomatic irreversibly rejected kidney transplant and, in the case of a chronically rejected asymptomatic graft, to withdraw immunosuppression and to prevent the development of anti-HLA antibodies that could delay or prevent a subsequent transplantation.
|
|
|
What is the management of hematuria after a transplant?
|
Early – usually do to catheter trauma or UTI….can be managed symptomatically w/ clot evacuation, treatment of UTI, CBI….rarely if ever have to re-explore
Late – can be a number of things including malignancy, UTI, renal disease…..rule out UTI then do regular hematuria eval including microscopy looking for casts. Adenovirus can cause hemorrhagic cystitis and is self-limited, resolving in 1-2 wk |
|
|
How is a fluid collection managed?
|
Usually, it is a benign & incidental finding.
If associated with pain, fever, then aspirate and culture- if it is pus, treat with antibiotics and drain; continue tac or cyclosporine, stop azathioprine, MMF, or sirolimus; and reduce dose of prednisone. If lymphocele, can unroof by open or laparoscopic techniques, but lateral to graft, just do open (lap too difficult) |
|
|
What is the management of urinary leakage after renal transplant?
|
This is usually at the site of ureteroneocystostomy and can be managed a number of ways. This may be initially simply managed with foley catheter w/ repeating of cystograms a week to two weeks later until urinary leak is healed.
This may need to be done with the addition of percutaneous nephrostomy tube placement and placement of ureteral stenting in an antegrade fashion. Rarely do you have to redo the anastomosis. |
|
|
After a renal transplant, what factors are important in choosing a penile prosthesis?
|
Stable graft function x 6 months with no rejection episodes
Low probability of device malfunction Low doses of maintenanc immunosuppression No intra-abdominal components Minimal tissue dissection No skin infections or UTIs Prophylactic abx and postop abx for at least 2 weeks |
|
|
There is an increased risk of congenital abnormalities in offspring of male transplant recipients who have fathered children.
|
False
|
|
|
What are the guidelines for successful pregnancy after renal transplantation?
|
Good health for 2 years after transplant
Minimal proteinuria No HTN No rejection No urinary tract obstruction Nearly normal renal function Low doses of maintenance immunosuppression |
|
|
Bicarbonate is reclaimed from the glomerular filtrate by what mechanism and where?
|
*Bicarbonate is reclaimed from the glomerular filtrate in the proximal tubules. Hydrogen ion secretion is coupled to sodium reabsorption. In the tubules the hydrogen ion combines with bicarbonate to make carbonic acid (like in carbonated beverages). This then dissociates to carbon dioxide and water and the carbon dioxide is reabsorbed into the tubular cell lumens. It then is hydrolyzed back to carbonic acid or bicarbonate that then diffuses into the peritubular blood.
|
|
|
What percentage of young healthy men on dialysis regain erectile function after transplant?
|
*Around 80%, get these guys some new kidneys!!
|
|
|
What is a frequent reason for early transplant organ failure in children?
|
Thrombosis is a significant cause of kidney transplant loss, especially in children (Singh et al, 1997).
Renal transplantation patients at risk for graft thrombosis are those with previous vascular access thrombosis, previous venous thrombosis, antiphospholipid antibodies, and previous large vein renal transplant thrombosis (DeLoughery, 2004). |
|
|
What are indications for pre-transplant nephrectomy
|
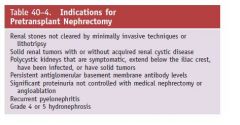
campbell's
|
|
|
How do you deal with a bladder that your not sure about its function in regards to a transplant kidney? In other words you aren't sure if it will function as a good low pressure resorvoir?
|
A defunctionalized bladder usually regains normal volume
within weeks of transplantation. It is advisable that transplantation candidates with small, contracted bladders who have had multiple lower urinary tract operations undergo bladder biopsy. If fibrosis is extensive on histologic examination and the bladder cannot be coaxed into becoming a lowpressure reservoir with bladder cycling, autoaugmentation or augmentation cystoplasty can be done before renal transplantation or afterward if satisfactory bladder function does not return within a few months (Barry, 2004). |
|
|
What is the preferred solution to store kidneys for transplant?
|
The commonly used UW solution (Belzer and Southard,
1988) minimizes cellular swelling with the impermeant solutes lactobionate, raffinose, and hydroxyethyl starch. Phosphate is used for its hydrogen ion buffering qualities, adenosine is for ATP synthesis during reperfusion, glutathione is a free-radical scavenger, allopurinol inhibits xanthine oxidase and the generation of free radicals, and magnesium and dexamethasone are membrane-stabilizing agents. A major advantage of this preservation solution has been its utility as a universal preservation solution for all intra-abdominal organs. campbells |
|
|
What is the typical vascular anastamosis for a renal transplant?
|
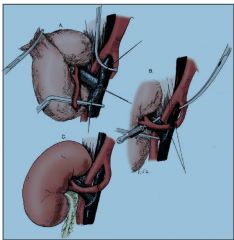
|
|
|
What are ABO blood groups and how do they relate to organ transplantation?
|
The histocompatibility systems of greatest importance in
renal transplantation are the ABO blood group and the major histocompatibility complex (MHC) (Denton et al, 1999; Halloran, 2004). The donor and recipient must be ABO compatible because A and B substances are present on endothelial cells, and most individuals have antibodies to the red blood cell antigens they lack. A common exception is the transplantation of ABO blood group A2 kidneys into blood group O and B recipients, who have low anti-A2 antibody levels (Alkhunaizi et al, 1999). A rare exception is the transplantation across major ABO incompatibilities by recipient preparation with plasmapheresis to remove anti-A or anti-B antibodies, off-label use of the anti-CD 20 antibody rituximab with or without splenectomy to reduce antibody production, and intense induction immunosuppression (Takahashi et al, 2004; Warren et al, 2004). |

