![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
9 Cards in this Set
- Front
- Back
|
Which factor(s) will influence refractive change of a LRI?
a. age b. pachy c. pre-op Ks d. IOP |
a. Age, as pt ages, a given LRI will have MORE effect
|
|
|
Def: regular vs. irregular astigmatism. With-the-rule vs. against-the-rule?
|
Reg: axes 90-degrees apart, w/in 15-degrees symmetrical
- With: +/- 15-degrees from 90 - Against: +/- 15 degrees from 180 - Oblique: everything else Irreg: 2 main axes not 90-degrees apart and not symmetrical btw eyes |
|
|
What is the refractive effect of LRIs? Where would they be placed to relieve with-the-rule astigmatism?
|
LRIs flatten in their plane, so you would place LRIs at 90/270 for with-the-rule (think: baby/flat)
|
|
|
How to address minor astigmatism during CE using LRIs.
|
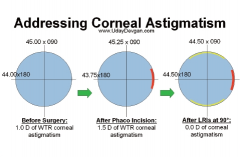
Steep axis at 90, slightly increased (0.5D) by main wound, so LRIs at steep (90/270).
|
|
|
POM #1 LASIK noted to have epithelial ingrowth, no Sx, 20/20. What next?
|
Observe. Often 1-2mm epi ingrowth causes no issues. If it does (astig/irritation), can lift flap conservatively, scrape or apply EtOH, then replace flap with BCL
|
|
|
POM #1 LASIK (ou) with 20/20 POD #1 presents w/ pain OD, 20/30 od, IOP wnl ou, tr cell and slight flap elevation od. Pt is taking PF 2/2 as Rx'ed (x2-3mo). Dx/What next?
|
PISK: pressure-induced stromal keratitis. IOP can be falsely read low due to LASIK flap floating on intervening fluid (cushioning). use Tpen peripheral cornea for accuracy. tr cell is likely wnl due to dilation.
Tx: STOP PF (LASIK pts usually only need for days/1 wk) |
|
|
When using microkeratome, what are flat corneas at risk for vs. steep ones (complications)?
|
Flat: free flap (if large enough, can just put cap on after LASIK)
Steep: button-hole (K buckles); abort and do surface ablation later |
|
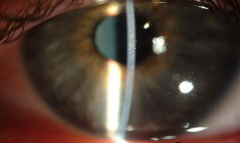
POW #1 LASIK w/ red, irritated OD. Dx? Staging? Tx?
|
DLK: diffuse lamellar keratitis
Infiltrates: stage 1=faint, periph, 2=faint, central, 3=dense, central, 4=dense central + flap melt Tx: PF, poss lifting flap to irrigate |
|
|
Pt w/ 20/30 found to have decentered ablation post-LASIK. Options?
-wavefront guided LASIK or PRK -wavefront optimized LASIK or PRK -topo guided LASIK or PRK |
Needs re-surfacing. with topo (3rd)
1. Wavefront guided (Visx): std in-OR aberrometry LASIK 2. Wavefront optimized (Alcon Allegreto Wavelight): smooths periph transition zone to reduce higher order abberations 3. topo guided (NIdek topolyzer): resurface w/ eximer (coming summer 2014) |

