![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
Cardiac myocytes deprived of blood supply start dying after how many minutes?
|
20
|
|
|
Death of the myocytes in a ____________________
myocardial infarction starts in the __________ zone, spreads in a wavefront to the ____________ zone and is usually complete after about _____________. |
Transmural (full thickness)
Subendocardial--> subpericaridal zone 3 hours |
|
|
What is the ECG evidence of ischemia?
|

ST-segment depression
T wave inversion |
|
|
How long does it take for dead myocytes to show microscopic manifestations of their death?
What is the one exception? |
4 hours
Dead thin wavy myocytes my be visible as early as a half hour after infarction. |
|
|
What are the three components of coagulative necrosis of dead myocytes in classic (UNREPERFUSED) myocardial infarction?
|
1. Loss of normal cytoplasmic striations
2. Cytoplasmic hypereosinophilia 3. Nuclear changes (pyknosis, karyorrhexis, karyolysis, loss) |
|
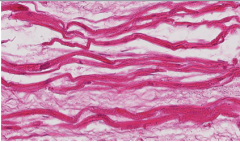
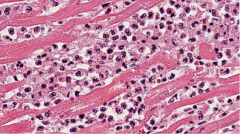
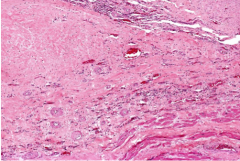
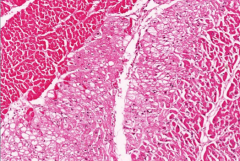
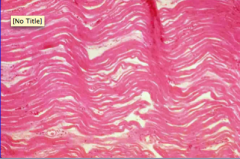
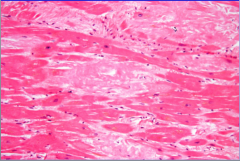
What is shown here?
What is this the earliest evidence of? How early can you see it? |
Thin wavy myocytes: sometimes present,
sometimes the earliest microscopic evidence of myocardial infarction, as early as 30 minutes after it has occurred |
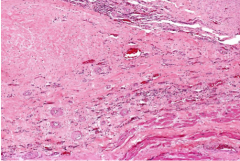
|
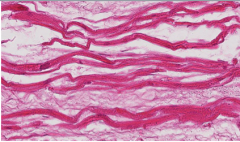
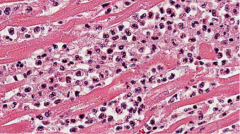
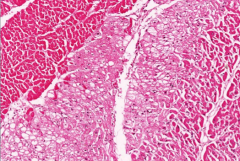
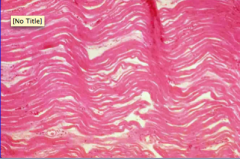
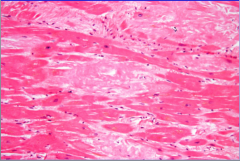
What is shown here?
What has not occurred yet? |
Cardiac myocyte coagulative necrosis in the narrow window after hypereosinophilia (and loss of striations, not evident here only because myocytes sectioned on end) have signaled necrosis, but before neutrophils have responded to the necrosis
� |
|
What is shown here?
When does this usually occur? |
Acute neutrophilic response to acute myocardial
infarction. This typically reaches maximum around 2 days. |
|
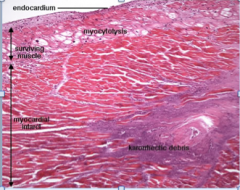
What is the karrorrhectic debris shown here? How does it arise? About how old would this infarct be?
|
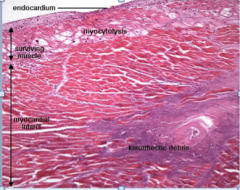
Since they only live for a day or 2, neutrophils
in an acute myocardial infarction begin contributing their breakdown debris after a few days and they yield much more karyorrhexic debris than cardiac myocytes, so extensive nuclear dust (as seen here) is a feature of infarcts 3-6 days old. |
|
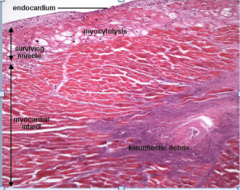
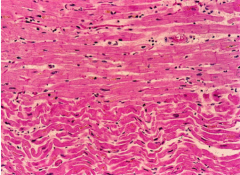
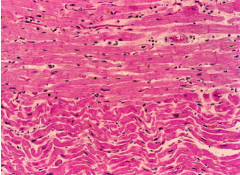
Describe the myocytolysis shown here.
|
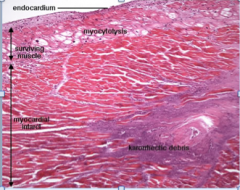
Thin subendocardial layer of cardiac myocytes that can get enough oxygen and nutrients from the cardiac luminal blood before it is pumped out to survive an infarct, survive, not prosper; they commonly catabolize their cytoplasmic contractile proteins (as seen here). Clearing of contractile proteins = MYOCYTOLYSIS.
� |
|
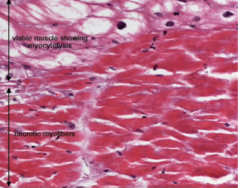
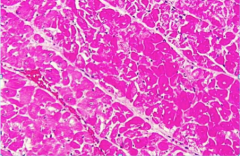
What is show in the image here?
What are the viable myocytes with myoctyolysis also called? |
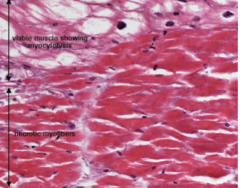
Here is a higher power view of the same infarct showing some of the viable myocytes with myocytolysis, which is also referred to as hibernating myocardium, and non-viable (dead) myocytes with
coagulation necrosis (showing loss of striations, hypereosinophilia and loss of nuclei). |
|
Why are the neutrophils in the subendocardial region? What else enters in this manner?
|
Because they come in from the edges (usually not including the subendocardial edge).
lymphocytes, macrophages and fibroblasts, who follow in the subacute healing phase. |
|
|
In classic (unreperfused) myocardial infarction, what enters in the early subacute phase (days 4-10)?
What happens in days 2-4? |
Infiltration by lymphocytes (bosses), first few at day 2 (sometimes), macrophages (garbage collectors), first few at day 3, fibroblasts (collagen engineers), first few at day 4, (+ / - eosinophils, plasma cells), beginning at the periphery
� |
|
What is this? About how many weeks after the infarct is this?
What types of cells do you see? |
This is a subacute (healing phase) myocardial infarction at 2-3 weeks with numerous fibroblasts and multiple new-grown blood vessels (neovascularization), which tend to come about the same time as fibroblasts, later than lymphocytes and
macrophages. |
|
Is this an early or late subacute infarct? How can you tell?
|
This is a very late subacute infarct, almost completely converted to a scar. Just a few lymphocytes still hanging around (surveying the work of the macrophages and fibroblasts they bossed around).
� |
|
|
Lead V1-V4 correspond to what wall and coronary artery?
|
Anterior, LAD
|
|
|
Leads II, III, and AVF. What wall and coronary artery?
|
Inferior, right
|
|
|
Leads I, aVL, V5-V6. What wall and coronary artery?
|
Lateral, left circumflex
|
|
|
How many hours does it take for dead cardiac muscle to show macroscopic (gross) manifestations of death?
|
12 hours
|
|
|
Acute inflammation (neutrophils), clean-up (macrophages) and repair (fibroblasts) all come in from the edge of a myocardial infarction because why?
� |
There is no blood supply to bring them there (that's why it's infarcted.
|
|
|
True or false.
The bigger the infarct, the longer it takes to heal and be converted to an acellular fibrous scar. How long does a really big one take? |
True
3 months |
|
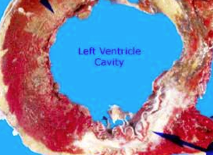
Classic myocardial infarction. Three locations.
Which is acute (hrs old), which is subacute (days old), and which is healed (weeks to years old? |
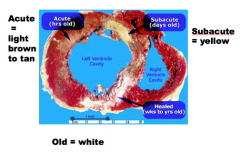
Answers.
|
|
|
What is a transmural infarction?
|
Involves the full thickness of the heart wall.
|
|
|
What are 90% of transmural infarctions associated with?
|
90% associated with occlusive thrombosis superimposed on atherosclerotic plaque with an acute change (disruption of an unstable vulnerable plaque by rupture or erosion)
� |
|
|
What does subendocardial infarction involve?
What will it look like? |
Involving inner portion of heart wall more likely to be patchy and to have episodic extension becoming more common than transmural.
� |
|
|
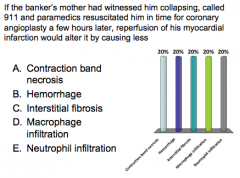
What are the nine effects of REPERFUSION?
|
Myocardial Infarction: Reperfusion Effects
1. Smaller than it would have been 2. More patchy than it would have been 3. Hemorrhage into it 4. More contraction band necrosis 5. Accelerated inflammation and repair 6. Diffusion of inflammation and repair 7. Fewer neutrophils 8. More macrophages 9. More interstitial fibrosis |
|
|
What is the microscopic pathology of subacute phase (4-10 days old) reperfused myocardial infarction?
What changes in repair do you see? |
Lymphocytes (+/- eosinophils, +/- plasma cells), then granulation tissue, collagen. Accelerated inflammation and repair: appears about 1 day older at 2 days
2 days older at 4 days 4 days older at 6 days |
|
|
Describe the microscopic pathology of subacute phase reperfused myocardial infarction days 11-the end.
How much can healing be accelerated? |
Healing of a large infarct can be accelerated from 12 to 7 weeks, a small one done by 2
Patches of preserved myocardium commonly interspersed with scar(may make re-entrant ventricular arrhythmias more common) |
|
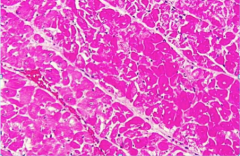
This myocardium has 3 zones: delineate, describe and diagnose each.
|
Zone 1 = hypereosinophilia + loss of nuclei = coagulative necrosis
Zone 2 = vacuolated (cleared) cytoplasm = myocytolosis Zone 3 = interstitial edema and viable myocytes |
|
A 55-year-old black male banker with a body mass index of 31 and 48 pack-year history of smoking ending 17 years ago has a 15-year history of diabetes
mellitus treated with metformin, hypercholesterolemia treated with atorvastatin, and hypertension treated with amlodipine and benazepril. He volunteers to mow his mother’s lawn, collapses while doing so and is found dead. Autopsy shows the following in his heart: What is the most likely cause of death? |
Myocardial infarction --> less than 4 hours old
|
|
What is this? How is it normally?
|
|
|
What is this?
|
Thin wavy myocytes
All dead and dead for a while --> nuclei have faded away. |
|
What is this?
|
Amyloidosis = confluent and hyaline (smooth and featureless)
|
|
This 37-year-old white female with a 22-year history of insulin-dependent diabetes was hospitalized 10 hours prior to death with chest pain and shortness of breath. Three months before, she had begun to experience progressive weakness and for the previous 3 weeks, she had increasing dyspnea on exertion and worsening of a chronic cough.
Describe and make two diagnoses. Why would fibrosis cause malignant ventricular arrhythmias? What is this called? |
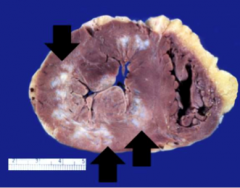
Left ventricle = concentric hypertrophy > 1.4 cm, numerous irregular patches of white scarring
Hypertrophic heart disease Scars from old MI Non conducting tissue --> electrical signal bounces off and sends in all directions to myocytes that pass it on before normal signal. MALIGNANT RE-ENTRANT VENTRICULAR TACHYCARDIA |
|
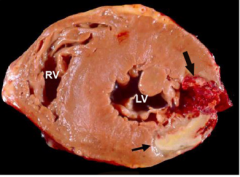
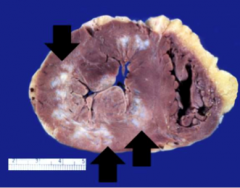
There is a myocardial infarction between the arrows.
How old is it? How can you tell? |
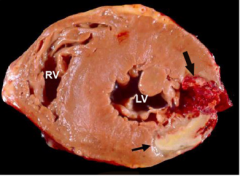
5 days old
3 zones (innermost = yellow, mid = tan, outer = grey-tan) Outer zone = young granulation tissue, many macrophages, not red because neovascularization comes later |
|
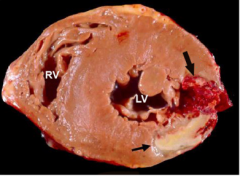
There is a cardiac rupture at the big arrow.
Where is it located relative to the infarct? Why is it located there? Why is it most likely at the time that it occurred relative to the infarct? |
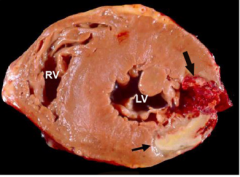
Cardiac rupture
Edge of infarct = surviving muscle pulling on necrotic muscle Necrotic muscle disintegrating into debris field --> consistency of water balloon on fifth day. |
|
|
When do you see thin wavy myocytes?
|
MI first visible as early as 30 minutes = earliest finding
|
|
|
What do you see with coagulation necrosis? When do you see it?
|
MI
Hypereosinophilia + loss of striations + nuclear pyknosis, then karyorrhexis, karyolysis, loss first visible at 4-12 hours |
|
|
When do you see neutrophilic infiltration?
|
MI (acute inflammation)
Follows myocyte necrosis 6-12 hours |
|
What is it?
|
E = decreased neutrophil infiltration
|
|
What is the answer
|
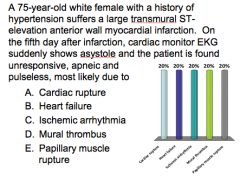
(A) Cardiac rupture!
|
|
|
Cardiac rupture is more common in which patients (5 things)?
When does it generally occur? |
Females (2x)
Elderly (>70) Hypertension history First MI Anterior wall infarct Occurs on the fifth day |
|
|
A 68-year-old white male bartender in Memphis, TN, with a history of smoking presents in February with worsening dyspnea and cough over several days.
Differential? |
HF due to IHD (silent MI)
Pneumonia (bacterial or viral) PE Autoimmune and idiopathic lung disease |
|
|
On further questioning, the dyspnea is on exertion and he has a chronic cough. He awakes at night sweaty, chilly, short of breath and coughing, but he has long had repeated nighttime awakening. He feels sick, has a stuffy nose, sore throat, muscle aches and joint aches, but his answers to questions are all vague and
he does not know what day it is. What could it be? |
Shock = confusion
Influenza = ill, malaise, nasal congestions, sore throat, muscle aches, and cough |
|
|
He appears ill and is obese. His temperature is 38, heart rate 110, blood pressure 110/60, respirations 29 and saturation 93%. His heart has an irregular rhythm, but no murmurs. He has bilateral basal pulmonary crackles. His abdomen is mildly distended, but not tender. He has mild ankle edema. His skin is cool and moist.
Now what do you think it could be? |
Causes of atrial fibrillation:
Heart failure, pneumonia, PE Fever = infection Ankle edema and bibasilar crackles = HF Cool, moist skin = shock |
|
|
His BNP is 400 (normal <100), hemoglobin 14 (nl 13-17), WBC count 21.6 (nl 4.5-11) with 78% segs, platelets 190 (nl 150-400), Na 135 (nl 135-145), and K 4.8 (nl 3.5-5).
Now what do you think? |
Elevated BNP = HEART FAILURE
Elevated white blood cell count and neutrophilia = infectious pneumonia Heart failure due to undiagnosed IHD and influenza pneumonia with sepsis --> precipitated HF |
|
|
What is the effect of sepsis on HF?
|
Vasodilation and increased metabolism --> increased HR and CO to meet increased demand
If coronary atherosclerosis limits blood flow, increased demand on pump can cause it to fail. |
|
|
True or false.
Warm skin can differentiate shock from other types. |
Sometimes...but don't count on it!
|

