![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
198 Cards in this Set
- Front
- Back
|
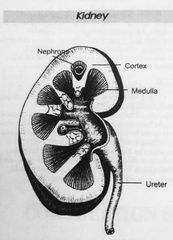
Diagram of a kidney |
|
|
|
Flow of urine through the nephron |
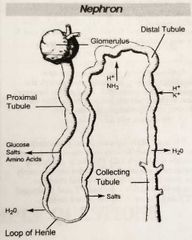
Glomerulus>proximal tube> descending/ascending Loop of Henle> distal and collecting tubules |
|
|
Nephron physiology |
1. Major functional unit of the kidney 2. Approximately 1 million nephrons per kidney 3. Each nephron is composed of glomerulus and renal tubules |
|
|
Glomerulus physiology |
1. Coil of capillary vessels 2. Glomerulus is a NON-SPECIFIC filter of plasma substances less than 70,000 MW 3. Glomerular filtrate is composed of water, glucose, electrolytes, amino acids, urea, uric acid, creatinine, and ammonia 4. Filters 120 ml/minute, or 1/5 of renal plasma |
|
|
Function of the proximal tubule |
1. Reabsorbs water, sodium chloride (salt), bicarbonate, potassium, calcium, amino acids, phosphates, protein and glucose 2. Glucose: threshold substance, reabsorbs at 160-180 mg/dl or less 3. Secretes sulfates, glucuronides, hydrogen ions and drugs Reminder: there should be no glucose in urine! |
|
|
Fuction of descending loop of henle |
Reabsorbs water No solutes reabsorbed As the filtrate travels down the loop of henle, the filtrate becomes more concentrated. |
|
|
Function of ascending loop of henle |
1. Reabsorbs solutes (sodium, chloride, calcium, magnesium) 2. NO WATER REABSORBED As filtrate travels back up the ascending loop of henle, it becomes less concentrated. The ascending loop is the only point in the whole process where water cannot go in our out of the tubules!!! |
|
|
Distal convoluted tubule |
PH regulation Reabsorption and secretion of H+ ions |
|
|
Collecting tubules functions |
Final point of water regulation!! The body utilizes hormones to regulate the amount of water in our body (ADH- anti-dieurtic hormone) Diurese: the act of urinating |
|
|
Functions of distal and collecting tubules |
1. Reabsorbs sodium 2. Secretes potassium, ammonia, and hydrogen ions 3. Potassium ions exchanged for sodium ions |
|
|
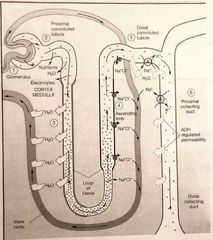
Reabaorption and secretion photo |
|
|
|
Hormones that influence urine output |
1. Aldosterone: electrolyte concentrations 2. Angiotensin: blood pressure 3. Anti-dieurtic hormone: water The process of regulating the amount of urine secreted by the body is controlled by hormones that respond in fluctuations in electrolyte concentrations, blood pressure, and water concentrations |
|
|
Normal urine output |
0.5 liters- 1.5 liters per day OR 1200-1500 ml per day |
|
|
Polyuria |
Increased urine output >2500 ml per day Diseases/causes: diabetes insipidus and mellitus, dieuretics, caffine, alcohol, excessive water intake |
|
|
Oliguria |
Decreased urine output <500 ml per day Diseases/causes: dehydration, vomiting, diarrhea, burns, perspiration |
|
|
Anuria |
Complete cessation (no urine output, or just DROPS) Diseases/causes: kidney damage, decreased blood flow to kidneys |
|
|
Nocturia |
Increased volume at NIGHT |
|
|
Urine composition |
1. Urea (non-protein nitrogen): metabolic waste product produced in liver from breakdown of protein, 1/2 total urinary dissolved organic solids 2. Other organic solids (non-protein nitrogens): uric acid, creatinine 3. Inorganic solids: chloride (primary constitute), sodium, potassium 4. Water |
|
|
Hormones: aldosterone |
Source: adrenal cortex Action: increases rate of sodium reabsorption |
|
|
Hormones: Arginine Vasopressin (AVP) |
**previously called ADH** Source: posterior pituitary gland Action: reabsorption of water from distal tubules
Deficiency of AVP: diabetes insipidus
Diabetes insipidus- disorder of salt and water metabolism marked by intense thirst and polyuria |
|
|
Hormones: erythropoietin |
Source: kidney Action: stimulates production of erythrocytes |
|
|
Urine Collection methods |
1. Random (clean catch): most common, easiest to collect 2. First morning: ideal screening specimen (most concentrated) 3. Midstream clean catch: clean external genetalia, specimen of choice for bacterial cultures 4. Cath: insertion of cath directly into bladder via urethra, avoids external contamination, but my introduce infection 5. Pediatric: sterile, plastic bag, bag checked every 15 minutes, many sources of contamination 6. Suprapubic aspiration: needle through abdomen directly into bladder, BEST specimen for bacterial culture, invasive procedure |
|
|
24 hour urine |
1. Collected over 24 hours 2. First specimen discarded while all others collected 3. Used for quantitative urine studies 4. Completeness of collection method monitored by creatinine levels (should be >1.0 mg/dl) |
|
|
Analysis of urines |
Analyze within 1 HOUR of collection |
|
|
Effects of prolonged sitting of specimens at room temperature |
Increased: nitrates (bacterial growth), pH ( urea converted to ammonia), turbidity
Decreased: glucose (glycolysis due to bacteria and yeast), ketones (exposure to air), bilirubin (exposure to light), urobilinogen, cells and casts (lysis)
Changes in color occur due to oxidation or reduction of metabolites |
|
|
Specimen preservation |
The best urine sample is freshly voided, midstream clean catch. Freeze: okay for chemical analysis, NOT UA Refrigerate: okay for UA, may have crystal formation, slows down bacterial growth Chemically preserve: BEST, boric acid powder |
|
|
Refrigeration of urine |
Preservation method of choice! (Up to 24 hours) May result in precipitation of amorphous crystals After removal from fridge, let sample return to room temperature before testing (about 15 minutes) |
|
|
Physical examination: odor |
Not evaluated, but may provide clues 1. Fruity- ketones 2. Ammonia- old urine 3. "Mousy"- PKU (phenylketonuria) 4. Maple syrup- maple syrup disease |
|
|
Physical examination: clarity |
Normal urine is clear Any of the urinary elements (cells, casts, crystals) or bacteria may make the urine cloudy |
|
|
Physical examination: color |
Normal urine is a pale yellow (straw) to yellow color Urochrome gives urine its normal color Urochromes or urobilin are products of RBC metabolism |
|
|
Physical examination: pH |
Normal urine is slightly acidic (6.0) Random samples: 4.5-8.0 Post prandial sample (2 hours post eating) may be alkaline When urine stands at room temperature for some time, ot becomes alkaline 1. Acidic: metabolic or respiratory acidosis, high protein diet, cranberry juice 2. Alkaline: vegetarian |
|
|
Color: Red |
Hemoglobin Red blood cells Myoglobin Porphrin Uroerythrin |
|
|
Color: Red-brown |
Hemoglobin Red blood cells Myoglobin |
|
|
Color: yellow-brown or yellow-green |
Bilirubin Biliverdin |
|
|
Color: yellow-orange |
Bilirubin Urobilin Pyridium (drug) |
|
|
Color: bright yellow |
Vitamin C |
|
|
Color: dark yellow |
Concentrated specimen Bilirubin Urobilin |
|
|
Color: brown-black |
Methemoglobin (oxidized RBC) Homogentistic acid (Alkaptonuria) Melanin |
|
|
Color: blue |
Indican (Tryptophane Metabolic Disorder) Methylene blue |
|
|
Color: green-blue |
Old urine Pseudomonas |
|
|
Color: port wine |
Porphyrin |
|
|
Specific gravity |
1. Offers the simplest way to check concentration and dilutiom function of kidney tubules 2. Normal: 1.002-1.035 3. Specific gravity is directly proportional to color, the higher the specific gravity, to darker the urine Exception: a pale color urine with high specific gravity is most likely due to glucose! Urine is diluted due to loss of concentrating ability by diabetics |
|
|
Highest specific gravity the kidneys can concentrate |
1.040 Higher values are due to either large amounts of glucose or radiographic dyes from renal x-ray procedures. Reagent strips for specific gravity are NOT affected by radiographic dyes |
|
|
Diabetes insipidus vs. Mellitus |
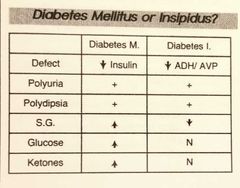
Polyuria- excess urine output (>2500) Polydipsia- excess thirst Specific gravity: DM- increased, remember the kidneys have a hard time reabsorbing glucose, and excess glucose causes increase specific gravity DI- decreased (excess water, less concentrated solutes) |
|
|
Refractometer- TS |
Measure: refractive index No temperature corrections Correct for large amounts of protein and glucose Corrections: Glucose- subtract 0.004 per gram Protein- subtract 0.003 per gram |
|
|
Specific gravity reagent strip |
Measures: indirect- colorimetric pKa change of polyelectrolytes (relative to ionic concentration) |
|
|
Chemical analysis of UA |
Specific gravity, pH, blood, leukocytes, nitrite, protein, glucose, bilirubin, urobilinogen |
|
|
Protein |
Proteins are produced by tubules in the kidneys (uromodulin)
Smaller proteins (microalbumins) can pass through the glomerulus, but mostbprotein that passes through the glomerulus is reabsorbed. |
|
|
Protein on reagent strips |
Principle: "protein error of indicators" Albumin in urine binds to dye, changing color from yellow to green The reagent strip is more sensitive tl albumin than globulin False positive: highly alkaline urine |
|
|
Proteinuria |
1. First indicator of RENAL DISEASE or dysfunction (not detected on reagent strips) 2. Multiple myeloma 3. Orthostatic proteinuria (benign condition resulting in proteinuria after standing) 4. Filtration problem (in glomerulus) or reabsorption problem 5. Strenous exercise |
|
|
Microalbuminuria |
Detected by sensitive albumin tests (level too low to be detected by routine reagent strip) Periodic monitoring benefits patients with diabetes, hypertension, and peripheral vascular disease Enables patients with low levels of albuminuria to begin treatment Several commercial methods for screening |
|
|
Protein confirmation |
Confirmed by SSA (sulfosalicyclic acid) The acidic pH of SSA denatures yhe structure of proteins, causing them to precipitate A urine sample positive for protein goes from clear to cloudy with the addition of SSA |
|
|
Glucose |
Should NEVER be in urine!! Essentially all glucose that enters the kidney is reabsorbed by the tubules The kidneys have a glucose reabsorption threshold of about 175 mg/dl Normal blood glucose is 110 mg/dl |
|
|
Glucose on reagent strips |
Specific for glucose ONLY Principle: glucose oxidase (double sequential enzyme reaction)- glucose oxidase turns glucose into gluconic acid and hydrogen peroxide
False positive: inteference by oxidizing agents (bleach or peroxide) False negative: reducing substances (ascorbic acid or bacteria- it eats glucose!) |
|
|
Two causes for glucosuria |
1. Diabetes mellitus 2. Reabsorption problems |
|
|
Diabetes mellitus v. Insipidus |
Mellitus: HIGH blood sugar, caused by decreases insulin, increased specific gravity, sugar and ketones present Insipidus: NORMAL blood sugar, caused by decreased ADH levels, decreased specific gravity, excessive thirst |
|
|
Clinitest tablet |
For glucose and other reducing sugars Positive: galactose, lactose, fructose, maltose, and pentose Screening test for galactosemia (rare congenital carbohydrate metabolic condition in pediatrics) Principle: Benedict's copper reduction test |
|
|
Copper reduction test vs. reagent strip |
RS -/CRT + = non-glucose sugar or other reducing substance RS +/CRT - = strip more sensitive to glucose than copper reduction |
|
|
Benedict's copper reduction test results |
Positive copper reduction test: sugar (or other reducing substance) other than glucose Negative copper reduction test with positive strip: glucose, because strip is more sensitive than copper reduction method
False negative: ascorbic acid (vitamin C) in extremely high doses |
|
|
Ketones |
In the absence of sugar, your body uses its fat storage for energy The metabolism of fat as a primary energy source reaults in the formation of ketone bodies
Ketone bodies seen in urine: 1. Beta-hydroxy-butyric acid: 78% 2. Acetoacetic acid (aka diacetic acid): 20% 3. Acetone: 2% |
|
|
Ketones on reagent strip |
Principle: sodium nitroprusside + ketones = PURPLE color
**acetoacetic (diacetic) acid is the only ketone body detected on reagent strips**
False positives: highly pigmented urine and levadopa metabolites, high specific gravity False negative: left at room temperature (acetoacetic acid is concerted to acetone, which evaporates upon standing) |
|
|
Confirmation of ketones |
Acetest tablets Specific for acetoacetic acid (diacetic acid) and acetone |
|
|
Increased ketones in urine seen in |
1. Uncontrolled diabetes mellitus 2. High protein diets 3. GI disturbances |
|
|
Blood in urine come in a few forms: |
1. Hematuria: intact red blood cells, cloudy, red 2. Hemoglobinuria: lysed red blood cells, clear, red 3. Myoglobinuria: muscle hemoglobin, more brown than hemoglobin |
|
|
Hematuria causes |
Intact red blood cells in urine Pathogenic causes: trauma to bladder, systemic bleeding disorders, renal diseases, kidney stones (calculi), strenous excerise Non-pathogenic causes: menstration |
|
|
Hemoglobinuria causes |
RBCs readily lyse in alkaline or dilute urine In most cases, the lysing of RBCs happen AFTER the kidney! (Like in the bladder) Causes for cell lysis before the kidney: sickle cell/hemolytic anemias, incompatible transfusions, maleria |
|
|
Myoglobinuria causes |
Myoglobin is heme-containing protein involved in the transport of oxygen in muscles Anything that causes strain on the muscles can release myoglobin into the blood Causes: muscle destruction, exercise, muscle trama, seizures, electric shock |
|
|
Blood on reagent strips |
2-step enzymatic process: 1. Peroxide on strip +blood= O2 2. O2 + chromagen = color change False positive: bleach and other oxidizing substances False negative: ascorbic acid (vitamin C), protein, high specific gravity, increased nitrates Hemoglobin and myoglobin have peroxidase activity |
|
|
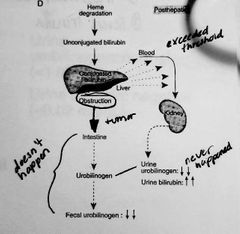
Lifespan and breakdown of bilirubin |
Bilirubin is a normal breakdown product of RBCs. 1. Bilirubin from RBCs floating in the blood. Albumin binds it up so it cannot get into cells (toxic to cells) 2. Uncongugated bilirubin: this albumin-bilirubin complex is too large to pass through glomerulus 3. The complex stays in circulation until it reaches the LIVER 4. Conjugated bilirubin: The liver removes the albumin and conjugates the bilirubin 5. Conjugated bilirubin can pass through the glomerulus. Almost all bilirubin is sent from liver to the intestines 6. The intestines break down bilirubin to urobilinogen 7. Most urobilinogen is broken down further and passed in feces 8. Some goes back into circulation where it ends up in kidneys |
|
|
Photo of breakdown of bilirubin |

|
|
|
Pathology of bilirubin |
Jaundice 3 causes for disrupted bilirubin: 1. Pre-hepatic (before liver) 2. Hepatic (in the liver) 3. Post hepatic (after the liver) |
|
|
Post hepatic bilirubin causes |
Obstruction!! Conjugated bilirubin never makes it to the intestines, not bilirubin is NEVER converted to urobilinogen Increased urine bilirubin **white/grey feces |
|
|
Bilirubin on reagent strip |
Diazo reaction: diazonium salts+ bilirubin= blue/purple color Confirmed by Ictotest False negative: ascorbic acid (vit C), strips exposed to light |
|
|
Bilirubinuria |
Associates with bile duct obstruction and liver damage (hepatitis or cirrhosis) |
|
|
Urobilinogen on reagent strips |
Principle: Ehrlich's reaction: para-dimethylaminobenzaldehyde in acid buffer + urobilinogen = pink/ cherry red color False negatives: formalin (preservative) False positive: some medication, highly pigmented urine |
|
|
Increased urobilinogen |
Liver damage Hemolytic disease |
|
|
Negative urobilinogen |
Indicates bile duct obstruction! |
|
|
Normal bilirubin/urobilinogen in urine |
Bilirubin: <0.02 mg/dL Urobilinogen: <1 mg/dL |
|
|
Nitrites |
Nitrate is a common food byproduct passed in the urine The bacteria that most often causes UTIs (E. Coli and Klebsiella) contain the enzyme nitrate reductase. This enzyme breaks down the normally found nitrAte into nitrite |
|
|
Nitrites on reagent strips |
The nitrate pad contains an amine and aromatic compound. The nitrite changes the amine into a diazo salt The diazo salt + aromatic compound = pink color change Any shade of pink is considered to represent a clinically significant bacteria Normal: negative |
|
|
False negatives on the nitrite reagent strip |
1. Lack of dietary nitrites 2. Urine not in bladder long enough (4 hours minimum) for bacteria to reduce nitrate to nitrite 3. Bacteria are present, but not nitrate reducers 4. Ascorbic acid (vit C) |
|
|
Leukocyte Esterase (enzymes) |
Enzyme produced by granulocytic white blood cells Lymphs DO NOT produce |
|
|
Leukocytes on reagent strip |
Principle: leukocyte esterase splits an ester to form pyrrole compound which reacts with a diazo reagent = PURPLE Positive indicates presence of leukocytes (pyuria) False positive: vaginal discharge |
|
|
Positive strip correlations |
pH- nitrite, leukocyte, microscopic Protein- blood, nitrite, leukocyte, micro Glucose- ketone Ketones- glucose Blood- protein, microscopic Bilirubin- urobilinogen Urobilinogen- bilirubin Nitrite- protein, leukocyte, microscopic Leukocyte- protein, nitrite, microscopic Specific gravity- none |
|
|
Reagent strip reactions: pH |
Reaction principle: 2 indicators provide wide spectrum of color changes False positives/negatives: none Significance: alkaline may indicate "old" |
|
|
Reagent strip reactions: protein |
Reaction principle: protein error of indicators- pH of strip = 3.0, dye changes color of strip False positive: alkaline urine False negative: high salt Significance: proteinuria: best single indicator of early disease (glomerular involvement), can be elevated after strenous exercise |
|
|
Reagent strip reactions: glucose |
Reaction principle: glucose oxidase method (double sequential enzyme) False positive: bleach False negative: ascorbic acid, ketones, high SG, low pH Significance: diabetes mellitus |
|
|
Reagent strip reactions: ketones |
Reaction principle: Na notroprusside + ketone = purple False positive: highly pigmented urine, Levapoda metabolites False negative: ascorbic acid, high specific gravity Significance: uncontrolled diebetes mellitus, high protein diet, dehydration |
|
|
Reagent strip reactions: blood |
Reaction principle: peroxide +blood = O2 + color indicator = color change False positive: bleach False negative: ascorbic acid, ketones, high SG, low pH Significance: 1. Hematuria (systemic bleeding, renal disease, cystitis, calculi, strenous exercise, menstruation), 2. Hemoglobinuria (incompatible blood transfusion, malaria, hemolytic anemia) 3. Myoglobin (muscle destruction) |
|
|
Reagent strip reactions: bilirubin |
Reaction principle: diazo salt + bilirubin = blue/purplish color False positive: medication color False negative: ascorbic acid, increased SG, nitrite Significance: bile duct obstruction, liver damage (hepatitis and cirrhosis) |
|
|
Reagent strip reactions: urobilinogen |
Reaction principle: para-dimethylaminobinzaldehyde + urobilinogen = peach/pink/cherry red color (Ehrlich's reaction) False positive: highly pigmented urine, some medication False negative: nitrite Significance: liver damage (hepatitis and cirrhosis), hemolytic anemias |
|
|
Reagent strip reactions: nitrite |
Reaction principle: nitrite+amine reagent =diazo compound (diazo compound+3-hydroxy-1.2.3.4 tetrahydrobenz)-quinolin =PINK color False positive: medication color False negative: ascorbic acid Significance: bacteria (UTI) |
|
|
Reagent strip reactions: leukocytes |
Reaction principle: leukocyte esterase splits ester to form pyrrole compound. Pyrrole + diazo reagent = purple False positive: bleach False negative: glucose, protein, high SG, some antibiotics Significance: WBC in urine most likely indicates presence of bacteria, reacts with granulocytes, NOT lymphocytes |
|
|
Reagent strip reactions: specific gravity |
Reaction principle: pKa change of polyelectrolyte False positive: protein False negative: alkaline urine Significance: decreased in diabetes insipidus, radiopaque dye |
|
|
4 Urine Stains |
1. Supravital stain: most common is Sternheimer-Malbin, stains everything 2. Gram stain: stains bacteria 3. Hansel stain: stains eosinophils (ex. Patient may be allergic to catheter) 4. Fat stains: Sudan III or Oil Red O (only fat cells pick up stain, confirms presence of fat or triglyceride) |
|
|
Normal urine sediment constituents |
0-2 RBC 0-5 WBC 0-2 hyaline cast Slight mucus |
|
|
Abnormal urine constitutes: red cells |
Normal 0-2 May indicate glomerular damage or menstrual contamination May be altered by pH and osmltic pressure to form "ghost", crenated or swollen cells May be confised with yeast cells and oil droplets; add 2% acetic acid to lyse RBC |
|
|
Abnormal urine constitutes: white cells |
May indicate inflammation or infection (pyuria) |
|
|
Casts |
Cylindrical form Having parallel sides Formed in the lumen of the distal convoluted tubule and collecting duct Major constitute of casts is uromodulin, a glycoprotein secreted by renal tubular epithelial cells |
|
|
Factors that influence cast formation: |
Decreased pH Decreased output Increased specific gravity Increased protein |
|
|
7 types of casts |
1. Hyaline 2. Red cell cast 3. White cells cast 4. Granular cast 5. Waxy cast 6. Fatty cast 7. Broad cast |
|
|
Hyaline cast |
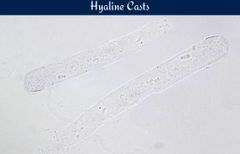
Most frequently seen Primarily uromodulin protein Seen in dehydration |
|
|
Red cell cast |

**Glomerular nephritis** (also known as intrinsic renal disease) Extensive damage to the glomerulus, bleeding from nephron, glomerular dysfunction Solid mass of tightly packed RBC with characteristic orange-red color (unstained sediment) |
|
|
Granular casts |
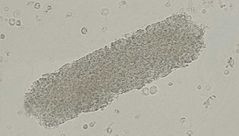
Severe dehydration Disintegration of cellular casts |
|
|
Waxy cast |

End stage renal disease cast Advanced stage of hyaline, granular, or cellular casts Indicates prolonged urinsry stasis (chronic renal disease) Square edges |
|
|
Fatty cast |
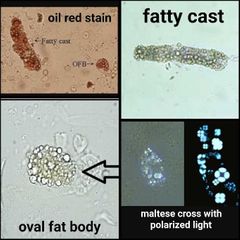
Breakdown of epithelial cell casts that contain oval fat bodies. Rare Significance: Nephrotic syndrome Must do a confirmatory stain (sudan or oil red) If cholesterol is present, the fat droplets will show a maltese cross pattern under polarized light |
|
|
Squamous epithelial cells |
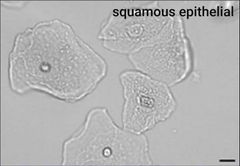
Largest, abudant irregular cytoplasm, central nucelus (RBC size) Notes: least significant, most frequently seen, normal in vaginal lining and lower uretha |
|
|
Transitional epithelial cell |
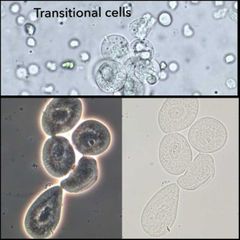
Round or pear shaped, central nucleus, absorbs water (swell to 3x normal size) Notes: renal carcinoma, renal pelvis, bladder, upper urethra |
|
|
Renal tubular epithelial cells |
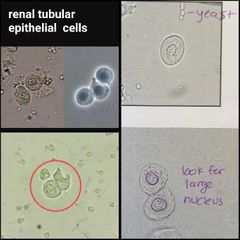
Most significant, round, eccentric nucleus, larger than WBC Notes: tubular necrosis, renal tubules |
|
|
Crystals |
Most crystals are clinically insignificant, because they can be formed in relation to changes in pH, and temperature. Significant Crystals are found in fresh urine! Presence of crystals may indicate renal calculi (kidney stones), metabolic disorders or drug overdose |
|
|
Crystals in alkaline urine (pH >7.0) |
1. Amorphous phosphates: white precipitate in urine, microscopically identical to amorphous urates 2. Triple phosphate: "coffin lid" 3. Ammonium biurate: "thorny apple" 4. Calcium carbonate: dumbell 5. Calcium phosphate: needles in a flower shape 6. Calcium oxalate |
|
|
Abnormal crystals |
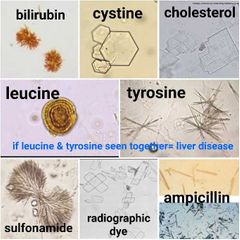
Indicate metabolic disorders or drug metabollites 1. Bilirubin: small yellow-brown cluster of fine needles 2. Cystine: colorless hexagonal plates 3. Cholesterol: tectangular plates with corner notches 4. Leucine: yellow-brown spheres with concentric circles 5. Tyrosine: fine, delicate needles (**when seen with leucine, liver disease indicated**) 6. Sulfonamide: needles or brown spheres, or fans 7. Radiographic dye: empty plates 8. Ampicillin: needles |
|
|
Review: crystals seen in normal acidic urine |
Calcium oxalate Uric acid |
|
|
Review: crystals seen in normal alkaline urine |
Triple phosphate Ammonium biurate Calcium carbonate Calcium oxalate |
|
|
Review: abnormal crystals |
Bilirubin Cystine (memory: sweet 16- six sides!) Leucine Tyrosine Cholesterol |
|
|
Other constitutes found in urine |
1. Bacteria- correlate with presence/absence of leukocyte esterase 2. Yeast- most often represents vaginal infection 3. Parasites- trich, enterobius vermicularis 4. Mucus- no significance 5. Clue cells- squamous epis with bacterial vaginosis |
|
|
Artifacts |
1. Powder (starch) 2. Fat/oil droplets 3. Fibers- fibers polarize, casts don't 4. Hair |
|
|
Inclusion bodies |
1. In viral infections, such as rubella and herpes, cells may contain inclusion bodies 2. CMV produces large intranuclear inclusions 3. Lead poisoning produces cytoplasmic inclusions 4. Hemosiderin (form of iron) contained in urine sediment indicates severe intravascular hemolysis, delayed transfusion reaction, PCH, or as a result of hemochromatosis |
|
|
Microscopic correlations: Red blood cell |
Physical appearance: turbidity, red color Chemical: blood |
|
|
Microscopic correlations: white blood cells |
Physical appearance: turbidity Chemical: protein, nitrites, leukocyte esterase |
|
|
Microscopic correlations: epithelial cells |
Physical appearance: turbidity Chemical: protein |
|
|
Microscopic correlations: casts |
Physical appearance: none Chemical: protein |
|
|
Microscopic correlations: bacteria |
Physical appearance: turbidity Chemical: pH, nitrites, leukocyte esterase |
|
|
Microscopic correlations: crystals |
Physical appearance: turbidity Chemical: pH |
|
|
Diseases of the urinary tract: glomerulonephritis |
RBC cast, increased blood, renal epis, WBCs Symptoms: fever, edema, nausea, oliguria (low urine output) Glomerulus involved, |
|
|
Diseases of the urinary tract: Nephrotic Syndrome |
Change in glomerular permeability, increased fat production Symptoms: edema (due to sodium retention), increased lipids in blood, blood pressure changes Clinical findings: increased protein**, blood, fatty cast, oval fat bodies, renal cells |
|
|
Diseases of the urinary tract: acute tubular necrosis (ATN) |
Tubular disease, causes the destruction of renal tubular cells. Possible afer trauma or post-surgical Toxic buildup of hemoglobin and myoglobin Symptoms: azotremia (BUN/creatinine), oliguria Clinical findings: decresed specific gravity, renal epi cast***, renal epithelial cells*** |
|
|
Diseases of the urinary tract: cystinuria |
Inherited disease where the proximal tubules cannot reabsorb cystine. Cystine readily precipitates in acidic urine and can cause kidney stones. People with cystinuria must always stay hydrated to prevent calculi formation |
|
|
Inherited metabolic disorders: Tyrosinuria |
Seen most often in newborns because the liver is immature. May see tyrosine and leucine crystals in acid urine Catecholamines (metabolic product of tyrosine) test is ordered, results will be decreased due to the body not breaking down tyrosine! |
|
|
Inherited metabolic disorders: Phenylketonuria (PKU) |
Increased urinary excretion of phenylpyruvate (keton) and its metabolites. Can result in severe brain damage or other developmental disorders This is why PKUs are done on ALL newborns! |
|
|
Inherited metabolic disorders: Maple Syrup Urine Disease |
Rare and most often seen in newborns. Its the accumulation of branched chain amino acids **Distinct maple syrup or caramalized sugar odor** |
|
|
Inherited metabolic disorders: Galactosuria |
Galactosuria is a lack of the enzyme or a deficient enzyme needed to break galactose into glucose Can result in liver damage, cataracts, ovarian failure, and brain damage |
|
|
Inherited metabolic disorders: Pyelonephritis (kidney disease) |
Acute: infection of renal tubules. Symptoms include flank pain, fever, nausea, increased frequency to urinate Clinical: leukocyte esterase, nitrites**, increased WBC, bacteria
Chronic: long lasting inflammation of tubules. Urine is allowed to flush backwards from the bladder up into the renal pelvis and back into the kidney Clinical: maybe leukocyte?, NO NITRITE, WBC cast, NO BACTERIA |
|
|
Pregnancy testing |
Human chorionic gondatropin (HCG), a glycoprotein composed of alpha and beta subunits is secreted by the placenta. Can be detected as early as 8-10 days after ovulation HCG peaks at 8-10 weeks First morning specimen is preferred |
|
|
Renal function tests |
Used to test glomerular filtration and tubular function
Tests for glomerular filtration: 1. Clearance tests 2. B2-macroglobulin 3. Cystatin C |
|
|
Creatnine clearance |
Most commonlu used clearance test to access GFR (glomerular filtration rate) This measures the amount of blood filtered to a particular substance in a given time
Production and excecretion of CREATININE is fairly constant day to day
24 hour urine Creatinine >1 mg measures adequacy of collection (Urine creatinine × volume) ÷ serum creatinine = creatinine clearance |
|
|
Creatinine clearance formula with correction for kidney mass |

Mililiters of plasma cleared of creatinine by the kidney per minute
(urine creatinine ÷ serum creatinine) × (urine volume ÷ 1440 minutes) × (1.73 ÷ body surface area) |
|
|
Normal creatinine clearance |
90-120 ml/minute for adults Decreases with age |
|
|
Estimated GFR |
Assists in detecting chronic kidney disease More sensitive than creatinine clearance Calculation based on serum creatinine, patient's age, gender, and ethnicity |
|
|
B2-Microglobulin |
Useful marker of renal tubular function Increased plasma concentration indicate a reduced GFR (not specific) |
|
|
Cystatin C |
May provide an equal or better detection of adverse changes in GFR Disadvantages: 1. Higher cost than creatinine clearance 2. Possible variable results among individuals |
|
|
Lab findings of acute glomerulonephritis |
Gross hematuria Smoky turbidity RBC casts Waxy casts |
|
|
Lab findings of chronic glomerulonephritis |
Hematuria All types of casts, but only occasional to few RBC casts |
|
|
Lab findings of acute Pyelonephritis |
Turbidity Positive nitrite Positive leukocyte esterase WBC casts Bacteria |
|
|
Lab findings of chronic Pyelonephritis |
Positive nitrite Positive leukocyte esterase All types of casts, but only occasional WBC cast |
|
|
Lab findings of nephrotic Syndrome |
May see "free" fat droplets Fatty casts Oval fat bodies |
|
|
Lab findings of cystitis/ lower urinary tract infection |
Bacteria WBCs |
|
|
Reasons for analysis of Cerebrospinal fluid (CSF) |
Meningitis Encephalitis Syphilis Brain abcess/tumor Intracranial hemorrhage Leukemia/lymphoma with CNS involvement |
|
|
CSF characteristics |
1. Normally clear, colorless 2. Xanthochromia: pink, orange, or yellow CSF supernatant (usually due to hemoglobin) Important to differentiate between intracranial hemorrhage and tramatic tap!! |
|
|
Differentiate between intracranial hemorrhage and tramatic tap |
Hemorrhage Appears: all tubes equally bloody Supernate: xanthochromic Clots: none Tramatic tap Appears: clearing of blood in each tube Supernate: clear Clots: yes, due to fibrinogen |
|
|
Distribution of CSF tubes |
1. Chemistry/serology: protein, glucose, lactate, VDRL, latex agglutination tests 2. Microbiology: gram stain, culture, india ink 3. Hematology: cell count and diff |
|
|
Normal CSF lab values |
Protein: 15-45 Glucose: 60-70% plasma glucose Cells: 0-5 WBC Differential: 70% lymph, 30% mono |
|
|
CSF electrophoresis |
OLIGOCLONAL BANDING = Multiple sclerosis Decreased glucose, increased protein |
|
|
Manual cell count calculation for body fluids |
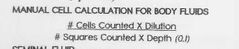
(# cells × dilution)÷ (# squares x depth- 0.1) **For CSF, pleural, pericardial and pertioneal fluids |
|
|
Differentiate causes of meningitis- CSF studies |
Bacterial Protein: very increased Glucose: decreased WBC: neutrophils Lactate: increased
Viral Protein: increased Glucose: normal WBC: lymphocytes Lactate: normal
Fungal Protein: increased Glucose: normal to decreased WBC: lymphocytes and monocytes Lactate: increased |
|
|
Reasons for semen analysis |
1. Infertility (most common) 2. Post vasectomy 3. Forensic medicine (presence of acid phosphatase confirms presence of semen in alleged rape cases; flavin in semen fluoresces on clothing under UV light) |
|
|
Male reproductive system |
Under the influence of testosterone, sperm are produced in the testicles and are stored in the epididymis In the epididymis, the sprem mature and become motile The sperm remain in the epididymis until ejaculation (sperm move to the vas deferens where they are carried to the ejaculatory duct) In the ejaculatory duct, fluid from seminal vesicles are added Semen is the joining of sperm and fluids!! |
|
|
Normal sperm morphology |
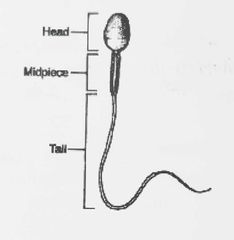
Counted as % of normal forms, normal range is greater than 50% |
|
|
Abnormal morphology |
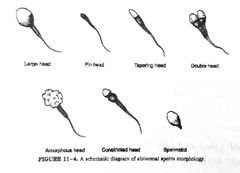
Range: <30% abnormal forms |
|
|
Reference ranges of sperm analysis |
Volume: 2-5 ml Count: 20-250 million/ml Motility: >50% Morphology: <30% abnormal forms Viability: >75% live forms |
|
|
Viability |
Normal: >75% live forms Azoospermia- no sperm Oligospermia- <20 million/ml (Normal count is 20-250 million/ml) |
|
|
Serous fluids and reasons for analysis |
Sepsis Malignancy Systemic disease Pleural, pericardial, peritoneal (ascites) |
|
|
Pleural fluid source |
Thoracic cavity (around lungs) |
|
|
Pleural fluid appearance |
Normal: clear to pale yellow Turbid: WBC cells, bacteria Bloody: trauma, malignancy Milky: chylous fluid |
|
|
Pleural fluid lab tests: |
Cell count Glucose PH Amalyse CEA (carcinoembryonic antigen) |
|
|
Pleural fluid: cell count significance |
Increased RBC: trauma, malignancy Increaced neutrophils: bacteria Increased lymphs: tuberculosis, malignancy |
|
|
Pleural fluid lab value clinical significance: glucose, pH, amalyse, CEA |
Decreased glucose: TB, rheumatoid inflammation, malignancy Decreased pH: TB, malignancy, esophageal rupture Increased amalyse: pancreatitis Increased CEA: malignancy |
|
|
Pericardical fluid source |
Pericardial cavity (around heart) |
|
|
Pericardial fluid appearance |
Normal: clear to pale yellow Turbid: infection, malignancy Bloody: TB, tumor, cardiac puncture Milky: lymphatic drainage |
|
|
Pericardial lab tests |
Cell counts Glucose CEA |
|
|
Pericardial fluid lab tests clinical significance |
Cell count: Increased RBC: TB, tumor, cardiac puncture Increased neutrophils: bacterial endocarditis Decreased glucose: bacterial infection Increased CEA: malignancy |
|
|
Peritoneal (ascites) fluid source |
Peritoneal cavity (around abdomen) |
|
|
Peritoneal fluid appearance |
Normal: clear to pale yellow Turbid: pertionitis, cirrhosis Bloody: trauma Milky: chylous fluid (rich in fats) Green: bile |
|
|
Peritoneal fluid lab tests |
Cell counts Glucose Amalyse Alkaline phosphatase Urea/creatinine |
|
|
Peritoneal lab tests significance |
Cell count Increased RBC: trauma Inceeased neutrophils: peritonitis Decreased glucose: tubercular peritonitis, malignancy Increased amalyse: pancreatitis, GI perforation Increased ALKP: Intestinal periforation Increased urea/creatinine: ruptured bladder |
|
|
Effusion |
Build up of a body fluid in a body cavity due to a pathologic process Pleural, pericardial, and peritoneal |
|
|
Reasons for analysis for synovial fluid |
Sepsis Hemorrhage Crystal induced inflammation |
|
|
Synovial fluid source |
Synovial membrane (around joints) |
|
|
Synovial fluid appearance |
Normal: clear, pale yellow and viscous Bloody: hemorrhagic arthritis Milky: crystals, cells Green tinge: bacteria Deep yellow: inflammation |
|
|
Synovial fluid cell counts |
Normal: <200 WBC <2000 RBC Increased RBC: hemorrhage Increased neutrophils: sepsis (>25%) Increased lymphs: non-septic infection |
|
|
Sweat |
Source: sweat glands (of skin) Appearance: clear and colorless Increased sweat electrolytes (sodium and chloride) confirms diagnosis of cystic fibrosis |
|
|
Gastric fluid source |
HCL and pepsin (secreted in stomach) |
|
|
Gastric fluid appearance |
Depends on diet |
|
|
Gastric fluid lab test and significance |
Titratable acidity Increased: duodenal ulcer, Zollinger-Ellison syndrome Decreased: pernicious anemia (no intrinsic factor) |
|
|
Reasons for amniotic fluid analysis |
Fetal well being Fetal lung maturity- 3 tests 1. Lecithin/Sphingomyelin ratio (L/S) 2. Phosphatidylglycerol (PG) 3. Lamellar body counts |
|
|
Lectin/Sphingomyelin (L/S) ratio |
Measures the phospholipids lecithin and sphingomyelin to assess fetal lung maturity If >2.0, fetal lungs are MATURE **(for diabetic mothers-PG must be present for fetal lung maturity) |
|
|
Phosphatidylglycerol (PG) |
Lipid component of pulmonary surfactants Not detected until about 35 weeks Absence does not rule out mature fetal lungs |
|
|
Lamellar body counts |
Secreted into aveolar lumen at 20-24 weeks Amniotic fluid is analyzed on automated instruments by using platelet count value Advantages: 1. Small sample volume 2. Short turnaround time 3. Low cost 4. Easily interpreted |
|
|
Other amniotic fluid testing |
1. Alpha-fetoprotein (AFP): if INCREASED, associated with neural tube disorders such as Spina Bifida 2. Bilirubin: reliable estimate of fetal red cell destruction due to maternal antibody, increased in HDFN 3. Creatinine: fetal age 4. Foam stability index 5. Fluorescence Polarization Assay |
|
|
Amniotic fluid appearance |
Normal: clear and colorless Yellow-green: bilirubin Red: red cell destruction (HDFN) |
|
|
Transudate vs. Exudate: color |
Transudate: colorless Exudate: Yellow-white: inflammation Red-brown: hemorrhage Yellow-brown: bilirubin Milky-green: chylous fluid (fatty) |
|
|
Transudate vs. Exudate: turbidity |
Transudate: clear, watery Exudate: cloudy, viscous |
|
|
Transudate vs. Exudate: specific gravity |
Transudate: <1.015 Exudate: >1.015 |
|
|
Transudate vs. Exudate: protein |
Transudate: <3 g/dl Exudate: >3 g/dl |
|
|
Transudate vs. Exudate: LD (lactic dehydrogenase) |
Transudate: <200 IU Exudate: >200 IU |
|
|
Transudate vs. Exudate: cell count |
Transudate: <1000/microliter Exudate: >1000/microliter |
|
|
Transudate vs. Exudate: increases associated with... |
Transudate: congestive heart failure, changes in hydrostatic pressure Exudate: infections and malignancies |
|
|
Differentiating benign and malignant cells in fluids chart picture |
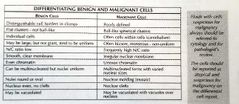
|

