![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
88 Cards in this Set
- Front
- Back
|
Ezetimbe
What is it? Place in Therapy |
Cholesterol Absorption Inhibitor
Add-on to statin therapy for LDL-C reduction; monotherapy for patients with contraindications or statin intolerance No outcomes data are available |
|
|
Ezetimbe side effects
|
|
|
|
Ezetimbe Monitoring
|
|
|
|
Ezetimbe Contraindications
|
NONE
|
|
|
Ezetimbe general info:
|
|
|
|
Ezetimbe with simvastatin (Vytorin)
|
• Same as ezetimibe (Zetia®) with simvastatin (Zocor®)
• Available in 10/10 mg, 10/20 mg, 10/40 mg, and 10/80 mg tablets • Usual starting dose: 10/20 mg or 10/40 mg daily in the evening |
|
|
Fixed dose Niacin with statin:
Advicor Simcor |
Advicor: extended release niacin(Niaspan) with lovastatin
Simcor: extended release naicin(Niaspan) with simvastatin |
|
|
Key Points:
Omega 3 fatty acids (FAs) |
• Docosahexaenoic acid (DHA) & Eicosapentaenoic acid (EPA) are only 2 omega-
3 fatty acids with cardiovascular benefits • Both DHA and EPA are equally on a mg-per-mg basis • Alpha linoleic acid is technically an omega-3, but does not have CV benefits • Used to provide TG lowering and non-HDL reductions • If TG ≥ 500 mg/dL might have an ↑ in LDL-C when treated with omega-3 FA • No increased risk of systemic toxicity when used with a statin |
|
|
Prescription FA:
Lovaza |
o Each 1 g capsule contains 465 mg EPA and 375 mg DHA
o FDA approved for hypertriglyceridemia o Dosing is 4 caps/day given once daily or BID with food (this dose provides 3360 mg omega-3 fatty acids daily) o Do not freeze these capsules |
|
|
OTC Fish Oil products
(nutritional supplements) |
o Typical products: 1 g contains 120 mg DHA and 180 mg EPA, the
remaining content is remnant fish oils o Other higher potency products are available o Use a product that is “USP-Verified” o Freezing or using enteric coated OTC fish oil products minimizes dyspepsia/fishy smelling belching o Dosing on OTC label will not lower TG values; higher doses are needed |
|
|
Omega 3 FA dosing
|
based on total amt. EPA and DHA
For: TG lowering: 2-4 g daily CV risk reduction in AVD pts: 1 g daily |
|
|
Starting dyslipidemia drug therapy:
|
o Select rational initial doses based on LDL-C reductions needed
o Titrate dose up and/or add an additional agent to achieve targets o For niacin, titrate dose up slowly to maximize tolerability o TLC is appropriate for all patients to augment effects of drug therapy |
|
|
Patient Education for dyslipidemia therapy
|
o Highlight the long-term benefits of therapy
o Describe appropriate use and special dosing considerations o Describe realistic expectation of side effects o Educate regarding precautions for myalgia depending on the regimen o Explain and encourage TLC |
|
|
High LDL-C
monotherapy and comination regimen options |
Monotherapy:
statin ezetimbe niacin bile acid sequestrant Combinations: statin + ezetimbe statin + bile acid seq. statin + niacin (higher risk systemic toxicity) niacin + bile acid seq. |
|
|
Mixed dyslipidemia
(High LDL-C, high TGs) monotherapy and comination regimen options |
Monotherapy:
statin(high dose needed) niacin Combinations: statin + fibrate (higher risk systemic toxicity) statin + niacin (higher risk systemic toxicity) bile acid seq. + niacin |
|
|
High TGs
monotherapy and comination regimen options |
Monotherapy:
fibrate niacin fish oil Combination: fibrate + statin (higher risk systemic toxicity) fibrate + niacin (higher risk systemic toxicity) Fibrate + omega 3 FA Niacin + statin (higher risk systemic toxicity) niacin + omega 3 FAs omega 3 FAs + statin |
|
|
Hypertryglyceridemia
|
|
|
|
Combination therapy key points:
dyslipidemia |
|
|
|
Metabolic Syndrome Criteria
|
3 of 5 needed to diagnose MetSyn:
1. Abdominal Obesity o Waist circumference ≥ 40” for men, ≥ 35” for women (lower in Southeastern Asian populations) 2. High Triglycerides o ≥ 150 mg/dL or drug treatment for elevated TGs 3. Low HDL-C o < 40 mg/dL (men), < 50 mg/dL (women), or drug treatment for low HDL-C 4. Elevated Blood Pressure o ≥ 130/≥ 85 mmHg, or drug treatment for hypertension 5. Elevated fasting glucose o ≥ 100 mg/dL, or drug treatment for hyperglycemia Tertiary Targets (HDL-C goals) apply to these patients after attaining both primary and secondary targets |
|
|
Diabetic Dyslipidemia
Type 2 diabetes |
“Diabetic Dyslipidemia” (a.k.a. atherogenic dyslipidemia):
|
|
|
Diabetic Dyslipidemia
Treatment and goals |
Nearly all should be on a statin:
|
|
|
Mechanisms by Which Diet Potentially Influences Risk of Coronary Heart Disease
|
DIET
--> INTERMEDIARY BIOLOGICAL MECHANISMS: 1. Lipid levels-HDL, LDL, TG, lipoproteins 2. BP 3. Thrombotic Tendency 4. cardiac rhythm 5. endothelial function 6. systemic inflammation 7. insulin sensitivity 8. oxidative stress 9. homocysteine level --> RISK OF CORONARY HEART DISEASE |
|
|
Coronary Heart Disease (CHD) Lifestyle
Risk Factors: |
Risk Factors:
– Obesity – High waist circumference • Men: >42” • Women: >35” – Physical Inactivity – Diet high in saturated & trans fat |
|
|
Weight Loss Effect on Lipids
|
• Weight loss will have profound affect on
lowering lipids, independent of macronutrient composition of diet (negative energy balance). • High waist circumference (visceral fat) highly correlated with CHD & Type 2 diabetes |
|
|
Butt fat vs. Gut fat cells:
|
Gut Fat:
•Large Insulin- Resistant Adipocytes •Adrenergic Receptors ↑ • Insulin-Mediated Antilypolysis •Catecholamine- Mediated Lipolysis ↑ -->increase Fatty Acids Butt Fat: •Small Insulin-Sensitive Adipocytes •Adrenergic Receptors ↓ |
|
|
Abdominal vs. reduced obesity
|
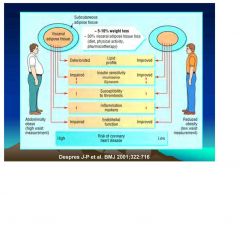
|
|
|
Plasma Lipids Improve with
Weight Loss Meta-analysis of 70 Clinical Trials |
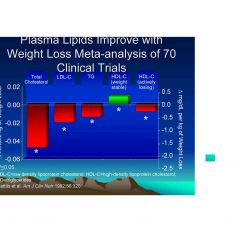
|
|
|
Relative risks of coronary heart disease for moderate overweight (body mass index [calculated
as weight in kilograms divided by height in meters squared], 25.0-29.9) adjusted for age, sex, smoking, and physical activity (A) and additionally adjusted for blood pressure and cholesterol concentrations (B), sorted by descending study size (reflected by the size of the square) |

|
|
|
Relative risks of coronary heart disease for obesity (body mass index [calculated as weight in
kilograms divided by height in meters squared], >=30.0) adjusted for age, sex, smoking, and physical activity (A) and additionally adjusted for blood pressure and cholesterol concentrations (B), sorted by descending study size (reflected by the size of the square) |

|
|
|
Dietary Fat Intake
|
• Total fat in the diet to be limited to 25-35% of
total daily calories • Types of Fat: – Saturated fat (“bad fat”) – usually solid at room temp • Increase total cholesterol and LDL; no changes to HDL – Foods sources: • Meat, poultry skin • High-fat dairy products • Fried foods, chips & snack foods • Butter • Baked goods (tropical oils) • AHA recommends <10% of calories from sat fat |
|
|
Trans Fats
|
• Trans Fats
– Increase total and LDL cholesterol – Decrease HDL cholesterol – As little as 1-3% of total calories from trans fat can impact cholesterol levels • Produced through process of “hydrogenation” – Food sources • Stick margarine • Crackers and snack foods • Baked goods • AHA recommends limiting trans fat (eating as little as possible) |
|
|
Unsaturated Fats
|
• Unsaturated Fats (usually liquid at room
temp) • Types of unsaturated fats: – Monounsaturated (olive oil, canola oil, peanut oil, nuts, avocado) – Polyunsaturated fats (sunflower, soybean, safflower oils) • AHA recommends 25-35% of calories from unsaturated fats |
|
|
Omega 3 FAs
|
• Omega-3 Fatty Acids
– Mainly from “fatty fish” (salmon, mackerel, tuna, but also flax seed oil) • Omega-3 FA have “anti-inflammatory” action • AHA recommends 2-3 servings/week of fish |
|
|
Carbohydrates and Lipids
|
• Diet high in whole grains and fiber associated
with lower blood lipid levels • Several studies link high fruit and vegetable intake with lower total cholesterol and lower CHD risk (antioxidant content) • Studies with antioxidant supplements have not shown the same benefits and may be harmful (Vitamin E & beta carotene) |
|
|
Protein and Lipid association
|
• Association between high animal protein
intake and increasing blood lipids • Association between higher protein from plant sources and lower lipids (Omni Heart Study). |
|
|
physical activity and lipid association
|
• Physical Inactivity major risk factor for
CHD • Regular physical activity contributes to primary and secondary prevention of CHD LDL Total cholesterol HDL Cholesterol 150 – 200 minutes PA per week to prevent a weight gain of <3% in most adults |
|
|
Physical activity for active weight loss
|
• <150 minutes/week
|
|
|
Physical activity for weight loss maintenance
|
• 200-300+ minutes/week (more research is
needed) • Do more, maintenance is better Physical activity is best predictor of weight loss maintenance!!!!!!!!! |
|
|
Resistance training and weight loss
|
• Research does not support resistance
training as effective for weight loss, with or without diet restriction. • May promote gain or maintenance of lean mass and loss of body fat. • May improve chronic conditions. • May increase functional capacity so client can (and may want to) do more. |
|
|
Common Nutrition/Lifestyle
Recommendations HTN |
Hypertension
– Weight Loss* – Increased physical activity* – Increased fruit & vegetable intake* – Decrease sodium intake *Associated with decreased incidence of type 2 diabetes |
|
|
Common Nutrition/Lifestyle
Recommendations Hyperlipidemia |
• Hyperlipidemia
– Weight Loss – Increased physical activity – Increased fruit and vegetable intake – Decreased saturated fat and trans fat intake* – Increased monounsaturated fat and omega-3 fatty acids *Associated with decreased incidence of type 2 diabetes |
|
|
How much physical activity is enough?
|
• Surgeon General: accumulate 30 minutes
of moderate intensity physical activity on most days of the week • 10,000 steps/day = 30 minutes of accumulated physical activity |
|
|
CORONARY ANATOMY
|
• coronary arteries branch from aorta
• epicardial vessels send branches into myocardium (= endocardial arteries) |
|
|
Which regions of the heart does the RCA supply?
|
rt. ventricle. + posterior. left. vent.
|
|
|
Which regions of the heart does the LCA supply?
|
ant. + lateral left. ventricle.
|
|
|
What does the coronary circulation deliver?
What does it remove? |
coronary circulation delivers nutrients
& removes metabolites/wastes |
|
|
Coronary perfusion occurs primarily during diastole rather than during systole. Why?
|
1. During systole, aortic valves block main coronary artery outflow.
2. As myocardium contracts, endocardial vessels are being compressed-->esp. the ones closest to the blood b/c more muscle is pushing it. |
|
|
Define myocardial ischemia
|
myocardial O2 supply is less than myocardial demand
|
|
|
myocardial O2 demands are met by:
|
coronary blood flow.
- myocardium can't extract more O2 from blood - blood can't carry more O2 - coronary blood flow can increase up to 5X (when there is an increase in demand) |
|
|
What can change myocardial O2 supply?
(coronary blood flow) |
Aortic Diastolic Pressure
Duration of diastole coronary vascular bed resistance |
|
|
How does aortic diastolic pressure affect myocardial O2 supply?
|
it is the coronary perfusion pressure
|
|
|
How does duration of diastole affect myocardial O2 supply?
|
increase duration of diastole to increase blood flow.
Can increase diastole by decreasing heart rate. |
|
|
How does coronary vascular bed resistance affect myocardial O2 supply?
|
Increase resistance to blood flow which decreases blood flow
|
|
|
vasodilation stimuli are:
|
hypoxia, adenosin, decreased pH
|
|
|
What affects myocardial O2 demand?
|
wall stress
heart rate contractility |
|
|
How does wall stress affect myocarcial O2 demand?
|
increase radius of the ventricle, increase myocardial O2 use
The more the ventricle stretches, the more O2 it uses |
|
|
How does Heart rate affect myocarcial O2 demand?
|
increase HR, increase O2
|
|
|
How does contractility affect myocarcial O2 demand?
|
increase contractility, increase O2 demand
|
|
|
What does exercise do to myocardial O2 demand and how does it do it?
|
Increase O2 demand by sympathetic NS activation
SNS activation increases HR and increases contractility |
|
|
Atherosclerosis Defn
|
Progressive accumulation of oxidized lipoproteins(LDL) and inflammatory cells under endothelium
-->atherosclerotic plaque -->vessel stenosis (narrowing) |
|
|
Damage of endothelium on Plaque Leads to:
|
plaque rupture -->
thrombus formation--> occlusion of the blood vessels |
|
|
T/F
Angina is a disease |
False, angina is a SYMPTOM
chest pain caused by myocardial ischemia |
|
|
Diseases caused by myocardial ischemia that angina is a symptom of:
|
coronary artery disease
ischemic heart disease |
|
|
spectrum of coronary disease:
from least to most severe |
silent ischemia
stable angina unstable angina non-Q wave MI Q wave MI |
|
|
Define silent ischemia
|
asymptomatic myocardial ischemia
imbalance in O2 supply and demand, but need ECG to diagnose decrease O2 demand, if ischemia, it can be seen on ECG -no overt signs to the patient |
|
|
Define stable angina:
|
includes classic and variant angina
|
|
|
characteristics of unstable angina:
|
Newly diagnosed angina--> until can define type of angina
change in anginal pattern (trigger for pain has changed) (variant angina) |
|
|
features of angina:
|
pain caused when coronary blood flow is inadequate to supply O2 required by myocardium
--> myocardial ischemia Pain caused by: 1. substances released during hypoxia 2. normal metabolites not removed by decreased coronary blood flow |
|
|
Define classic angina
|
(exertional angina, angina of effort)
• associated with atherosclerotic disease of coronary arteries • occurs when metabolic needs of myocardium exceeds ability of occluded coronary vessels to deliver adequate blood flow • precipitated by factors that increase work demands on the heart e.g., exercise exposure to cold emotional stress • diagnosis = pain relieved by rest or NTG |
|
|
Define Variant angina
|
(vasospastic angina, Printzmetal's angina)
• associated with spasm of coronary arteries (mainly in presence of stenosis) - hyperactive sympathetic nervous system - defective Ca2+ handing by coronary vascular smooth muscle - altered endothelium-derived factors favoring vasoconstriction - ↑ endothelin or AII - ↓ PGI2 or nitric oxide • occurs during rest or with minimal exercise - frequently nocturnal - cyclic or regular occurrence |
|
|
Define Unstable Angina
|
(preinfarction angina, crescendo angina)
• associated with obstructive coronary artery disease (+ coronary vasospasm?) - thrombotic occlusion of coronary artery at site of atherosclerotic plaque - initiated by platelet aggregation • pain characterized by changing pattern • occurs during rest, appears more frequently and lasts longer • accelerated form of angina |
|
|
What can be done to decrease O2 demand?
|
increase aortic DBP
increase diastole duration (decrease HR) decrease resistance (dilate vessels) |
|
|
What can be done to increase O2 supply?
|
decrease ventrilcular filling
decrease HR decrease contractility |
|
|
Therapeutic objective for myocardial ischemia:
|
balance O2 supply and demand
- improve coronary blood flow - reduce myocardial O2 requirement |
|
|
List the NITRATES
|
nitroglycerin
isosorbide mononitrate isosorbide dinitrate |
|
|
MOA of nitrates:
|
relax blood vessels by:
release of nitrite → NO formation → activation of guanylate cyclase → smooth muscle relaxation (Veins > Arterioles) Relaxation of epicardial coronary vessels total coronary blood flow is not increased -> not a generalized vasodilation coronary flow redistributed from normal to ischemic area via collateral vessels |
|
|
What are the beneficial Effects of dilating veins?
|
increase endocardial blood flow
decrease myocardial O2 consumption |
|
|
What are the beneficial effects of dilating arterioles?
|
coronary vessel dilation
decreased myocardial O2 consumption |
|
|
What disadvantageous effect can occur by dilating veins?
|
Increased contractility, increased HR = NOT GOOD
If decreased BP too much, reflex tachycardia offsets the beneficial effect |
|
|
Side Effects of Nitrates
|
• orthostatic hypotension, dizziness, syncope (b/c vasodilation)
NOTE: If ↓ VR too much → decrease aortic DBP, decrease coronary perfusion pressure • throbbing headache • flushing • ↑ sympathetic discharge-reflex (increase HR and contractility, increase O2 demand) • tolerance- dilator effect wears off w/ continual use -8 hr abstinence period each day or lose effectiveness e.g., explosives factory workers • dependence continual exposure to nitrates ⇒ if remove nitrates for 1-2 days →coronary vasospasm ∴ in chronic users, taper dosing when w/drawing nitrate |
|
|
Indications for Nitrates
|
• used acutely or prophylactically
- sublingual NTG (quick, 1-2 min) - buccal, oral, transdermal (maintenance) ->TOLERANCE SE, must give 8 hr break |
|
|
Administration of a nitrate to a patient who has taken sildenafil (Viagra®), vardenafil (Cialis®) or
tadalafil (Levitra®) can lead to a precipitous drop in blood pressure. What mechanism underlies this effect? |
They act by blocking PDE5
normally: nitrate->NO->guanylate cyclase->cGMP->vasodilation cGMP is metabolized by PDE5, and this is blocked by ED drugs, so cGMP levels increase because not being metabolized by PDE5, increase vasodilation, and decrease BP! |
|
|
Calcium Channel Blockers
|
verapamil
diltiazem amlodipine nifedipine nicardipine felodipine |
|
|
MOA CCBs:
|
Arteriolar selective
• inhibit voltage-dependent calcium channels (see previous section) → ↓ Ca2+ influx → smooth muscle relaxation • vasodilation → ↓ peripheral vascular resistance → decrease afterload → decrease cardiac work → O2 demand (good for classic angina) • ↓ coronary artery tone → increase coronary perfusion → increase blood flow → O2 supply good for variant angina • ↓ Ca2+ influx in to myocardial cells (verapamil > diltiazem=cardiac suppressive effects) → decrease contractility → decrease O2 demand • slows SA node (verapamil, diltiazem) → ↓ HR → decrease O2 demand |
|
|
Side Effects CCBs:
|
hypotension
dizziness fatigue cardiac depression (verapamil and diltiazem + beta blocker b/c decrease AV block and decrease ventricular function) CCB drugs can be contraindicated in heart failure |
|
|
Beta blockers
|
atenolol
metoprolol propanolal nadolol timolol |
|
|
beta blocker MOA
|
β-blockers inhibit effects of catecholamines on heart
exercise, stress → increase sympathetic drive OVER THE LONG TERM, β-blockers ↓ BP by ↓ PVR → decrease afterload, decrease O2 demand |
|
|
Side Effects beta blockers
|
• ↓ heart rate → ↑ end-diastolic volume → ↑ wall stress
→ increase O2 demand (partially offset beneficial effects) ->combine with nitrate to decrease VR • withdrawal of chonically-administered β-blocker → exacerbation of angina and ventricular dysrhythmias b/c upregulated beta-receptors can now be activated |

