![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
goal of population health models |
- increasing health of population -eliminating disparities - decrease mortality rates |
|
|
Define determinants of health |
analyzing patterns or distribution of health between different groups of people in order to identify and understand the factors leading to poorer outcomes |
|
|
5 key determinants of health |
1. social & economic environment 2. physical environment 3. genetics & epi-genetics 4. medical care 5. personal health behaviors |
|
|
determinant of health: social and economic environment (explain) |
factors like income, education, employment, social support, and culture |
|
|
determinant of health: physical environment (explain) |
including urban design, housing, availability of healthy foods, air and water safety, exposure to environment toxins |
|
|
determinant of health: genetics & epigenetics (explain) |
the study of gene environment interactions |
|
|
determinant of health: medical care received (explain) |
including prevention, treatment, and disease management |
|
|
determinant of health: health related behavior (explain) |
such as smoking, exercise and diet, and drinking |
|
|
correlation vs. causation in studying health determinants |
- "web of causation" - different influences interact to produce good or poor health ex: outcome of being unhealthy can cause poor income, poor income can cause being unhealthy |
|
|
contrasting population health with traditional medical care system approach (health problem example) |
in medical model: when obese adolescent visits health care provider; provider will take family history, diet, physical history & may be followed with lab tests to rule out illnesses & recommendation will be made to reduce calories,etc. in population health model: identifies variety of causes that may have produced epidemic like: - presence of vending machines - school lunches --> high calorie & fat content -decrease in physical education -fewer children walking to school/outdoor playing due to unsafe neighborhoods & lack of sidewalks |
|
|
mortality |
- death rate by specific cause, specific age group, at a certain time, etc |
|
|
morbidity |
- level of sickness in a given population at a time & how it affects persons daily life |
|
|
recognize finds of Robert Woods Johnson Foundation research on race, education, and health |
-higher education = higher paying jobs with greater economic security, healthier workings conditions, better benefits, increased ability to purchase healthy foods, and live in a safe place - level of education influences lifestyle (page 87 in book, chart) |
|
|
gradient |
the steady increase of mortality rates - "gradient" = population health model - "dose-response effect" = medical model -taken as evidence of a robust relation between casual factor and outcome |
|
|
which determinants have the greatest/least weight in County Health Ranking model |
(outcome = morbidity) 1. social and environmental = 40% 2. health behaviors = 30% 3. medical care system = 20% 4. physical environment = 10% |
|
|
medical model vs. population health model |
medical model: focuses on individual, focuses on factors that are most immediately linked to the pathophysiology underlying a persons disease vs. population health model: seeks to explain and intervene in the causes of the systematic differences in health behavior between different groups |
|
|
World Health Organization definition of public health |
Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity |
|
|
10 great achievements of public health |
1. vaccinations 2. motor vehicle safety 3. safer workplaces 4. control of infectious disease 5. decline in deaths from coronary heart disease 6. safer and healthier foods 7. healthier mothers and babies 8. family planning 9. fluoridation of drinking water 10. recognition of tobacco as health hazard |
|
|
public health is decentralized & its different organizations |
- government is decentralized - states have authority for public health except when specified by federal gov. - rely heavily on outside organizations (that are issue specific) like: planned parenthood, Red Cross,etc. example: federal government requires seat belts and air bags in care but state laws mandate their use but local police enforce laws |
|
|
Primary health interventions |
helping people avoid the onset of a health condition, including injuries |
|
|
Secondary health interventions |
identifying and treating people who have risk factors or preclinical disease |
|
|
Tertiary prevention |
treating people with an established disease, in order to restore their highest functioning, minimize negative effects, and prevent complications |
|
|
Universal prevention |
universal prevention means that everyone receives an intervention equally -these are more effective in improving the health of populations |
|
|
Targeted prevention |
targeted prevention involves identifying and serving people at higher risk-important focus for public health when the risk is prevalent & there are effective means to identify and treat it |
|
|
3 core public health functions |
1. assessment 2. policy development 3. assurance |
|
|
Core public health function - assessment |
- monitoring health status to identify and solve community problems - diagnose and investigate health problems and health hazards in the community |
|
|
Core public health function - policy development |
- inform, educate, and empower people about health issues - create and advocate for solutions to achieve public health goals |
|
|
Core public health function - assurance |
- enforce laws and regulations that protect health and ensure safety - link people to needed personal health services and ensure the provision is health care when otherwise unavailable - involves enforcement of policy (inspection of restaurants, sanitation or nursing home safety, monitor legal compliance) |
|
|
Nongovernmental organizations and role in public health |
America relies heavily upon nongovernment organizations to achieve public health goals like: Planned Parenthood American Red Cross American Heart Association United Way Worldwide |
|
|
Zika virus as public health effort |
- Zika virus is spread to people by the bite of an infected mosquito, people can protect themselves by wearing long sleeves, having protected sex, sleeping under mosquito net, and using insect repellents -- not transmitted in Maine (only travel associated) |
|
|
Maine CDC Organizational Chart |
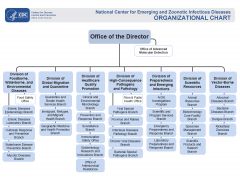
- do not need to memorize |
|
|
Health promotion |
the science and art of helping people change their lifestyles to move toward a state of optimal health* *optimal health: defined as balance of physical, emotional, social, spiritual and intellectual health |
|
|
Definition of behavioral risk factor |
- element of personal behavior such as unbalanced nutrition, use of tobacco products, or abuse of alcohol -- leads to increased risk of developing one or more diseases or negative health conditions |
|
|
Tobacco use |
- 19% in 2011 & 18% in 2012 - reduces life expectancy by 10 years - associated with low birth weight (20%) and preemie babies (8%) |
|
|
alcohol use definition of binge drinking |
binge drinking is indulging in 4 or more drinks within an hour for women, and 5 or more drinks within an hour for men - 20% of the population engages in risky alcohol use |
|
|
Exercise |
- 48% of population engages in 75 minutes per week of moderate exercise |
|
|
Diet and nutrition |
- 4 of the 10 leading causes of death are associated with unhealthy diet |
|
|
Obesity |
- 68.5% of adults are overweight or obese |
|
|
5-A model of physician assisted health behavior change |
- Assess - Advise - Agree - Assist - Arrange - used to help patient set and reach goals |
|
|
Chronic Care Model |
take people with known chronic condition (asthma, hypertension, high blood pressure, diabetes, etc.) and have check ins when they’re healthy before they get sick & actively reach out to monitor status of disease, track doctors entire patient population |
|
|
Stages of Change Model |
- Precontemplation - Contemplation - Preparation - Action - Maintenance - Relapse
|
|
|
Stages of change model - precontemplation |
- no plans to change behavior, behavior is not seen as a problem |
|
|
Stages of change model - contemplation |
serious plans to change behavior within the next 6 months, weighing the pros and cons, building support and confidence |
|
|
Stages of change model - preparation |
plans to change are still imminent, small initial steps are taken |
|
|
Stages of change model - action |
active attempts are made to quit smoking, drink less, become more active, or change to healthier diet and to sustain change up to 6 months |
|
|
Stages of change model - maintenance |
change is sustained beyond 6 months |
|
|
Stages of change model - relapse |
the individual returns to any earlier stage and begins to recycle through the earlier stages |
|
|
Social learning theory |
emphasized interactions between internal and external environmental influences on behavior - includes techniques such as modeling and behavioral practice to help people learn not just why but how to change unhealthy behaviors |
|
|
Social ecological models of change |
emphasize that a persons health behavior is affected by multiple levels of influence like -interpersonal factors (knowledge, skill, motivation) - social factors (cultural norms, support, network) -organizational and community factors - broader environmental influences - public policies |
|
|
Upstream interventions for health behavior change |
upstream: state and national pubic policy/ environmental interventions aim to strengthen social norms |
|
|
Midstream interventions for health behavior change |
midstream: population level interventions that target defined populations in order to change/prevent behavioral risk factors |
|
|
Downstream interventions for health behavior change |
downstream: individual level interventions aimed at those who possess a behavioral risk factor |
|
|
definition of a vulnerable population |
an umbrella term for all of the individuals who are at a greater risk for poorer health status and health care access |
|
|
Predisposing factors |
-can't do anything about them (like age, race, ethnicity, etc.) |
|
|
Enabling factors |
(eg. health insurance, social capital) |
|
|
Health need factor |
- physical illness, emotional illness |
|
|
Why are the numbers of people vulnerable for poor health increasing? |
1. rise in diseases like diabetes and cardiovascular disease 2. shifting demographics, growing income inequality between rich and poor and graying of baby boomer generation 3. shrinking and strained sector of supportive services in low income communities |
|
|
Types of healthcare agencies whose mission is to serve vulnerable people? |
- public hospitals - federally qualified health centers - rural health centers - migrant health centers |
|
|
Social Service Safety Net |
- food assistance - income assistance - housing assistance |

