![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
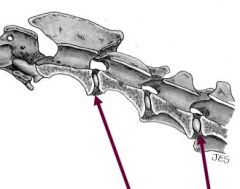
What is the Vertebral formula = # of vertebrae in each region for cat and dog?
|

For dog & cat = C7, T13, L7, S3, Cd ≈ 20
|
|
|
Signs assoc. with C1-6' Cervical lesion?
|
no "head signs"
UMN signs to all 4 limbs |
|
|
Signs assoc. with C6 _ T2 : cervicothoracic lesion?
|
Tetraparesis/paralysis.
(bipedal gait) - LMN signs to thoracic limbs - UMN signs to pelvic limbs • ± Horner's syndrome |
|
|
Signs assoc. with L4-S2: lumbosacral & cauda equina lesion?
|
• LMN signs to rear limb
• Normal thoracic limbs • UMN signs: bladder, anus & urethra |
|
|
Signs assoc. with T 3- L3, Thoracolumbar cervicothoracic lesion?
|
• UMN signs to rear limbs
• ± Cutaneous trunci • Nonnal thoracic limb (+/- Schitf-Sherrington) |
|
|
What is Schiff-Sherrington syndrome?
|
Hyperextension of forelimbs with damage/lesions to thoracic spinal cord (T3-L3 / area 3)
Only time a spinal cord injury causes signs cranial to damage/injury LMN and UMN are still intact to thoracic limb, so this is neither UMN or LMN neuron sign. (hindlimb may show UMN signs) From Online: Extensor hypertonia (increased muscle tone ) of the thoracic limbs and paraplegia resulting from acute, severe, compressive lesions of the thoracolumbar spinal cord that REMOVE the inhibitory effects of neurons in the lumbar spinal cord. Seen in dogs, usually caused by trauma or herniated intervertebral disk. Border cells in L1-4 ascend to inhibit extensors of forelimb to coordinate movement |
|
Intervertebral Disk or fibrocartilaginous disks consists of inner jelly like part and outer part known as the _____ and ______?
|
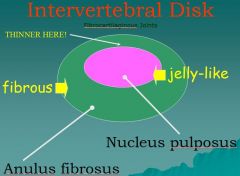
nucleus pulposus
anulus fibrosus |
|
|
What is responsible for consciousness and arousal? Where is it located?
|
Reticular activation system (RAS), brainstem
|
|
|
for tards:
difference between vertebral column and spinal cord |
- vertebrae are actual bone
- protect the spinal cord |
|
|
Intrathecal injection
|
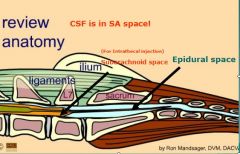
in Lumbar cistern- between L4-5 or L5-6
access to CSF (subarachnoid space) |
|
|
Epidural anesthesia goes where?
|
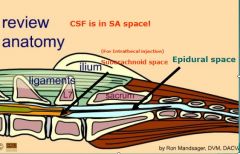
lumbosacral junction (in small animals) in epidural space
Epidural space: between the dura mater & vertebrae Filled with fat Epidural anesthesia is performed within this space |
|
|
Where are upper motor neurons (UMN) located?
|
In the CNS (brain and spinal cord), descending to synapses on LMN (check second portion)
|
|
|
List the spaces that are related to the meninges
|
* Epidural: between dura mater and periosteum
* Subdural: potential space between the dura mater and arachnoid * Subarachnoid space: between the arachnoid and pia (CSF) |
|
|
Cr N 7 Facial
|
Motor to muscle of facial expression
ANS motor to lacrimal gland, salivary glands |
|
|
What is the disease of the cervical vertebrae in large breeds causing STENOSIS of the vertebral canal resulting in ataxia (unsteady gait)?
|
Cervical spondylomyelopathy, canine wobbler disease
|
|
|
What is excessive ventral lumbar curvature?
|
Lordosis (swayback)
|
|
|
CrN 8
|
Vestibulocochlear
Special sensory Hearing & equilibrium |
|
|
What is spina bifida?
|
Failure of 1 or more vertebral arches to close
|
|
|
Causes dropped jaw
|
Paralysis CrN 5 trigeminal
|
|
|
A slipped disc results when the soft ___ ___ is squeezed to one side of the disc, causing the firm ___ ___ to protrude and possibly rupture.
|
* Nucleus pulposus
* Annulus fibrosus |
|
|
Where are CSF taps performed?
~looking for name of region or place, not the layer |
Cisterna magna or lumbar cistern (subarachnoid space)
|
|
|
What is the lumbosacral space?
|
Interarcuate space between last lumbar vertebrae (L7) & sacrum
(where insert needle when giving epidural injection) |
|
|
How is proprioception evaluated clinically?
|
Postural reactions (e.g. knuckle paw)
|
|
|
identify thoracolumbar spinal cord
(what is located here?) |
Of or relating to the thoracic AND lumbar parts of the spinal column.
sympathetic division of the autonomic nervous system (specifically thoracolumbar: T3 to L3) |
|
|
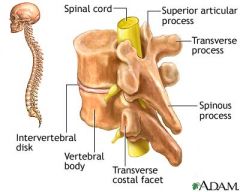
What arises from spinal cord to FORM a spinal nerve?
What arises from spinal nerve? |
dorsal and ventral roots (NOT branches)
dorsal and ventral branches; these are formed when spinal nerve "branches" |
|
|
What is the function of most UMN (upper motor neurons)?
|
Inhibit spontaneous activity of LMN until an action is desired
|
|
|
Pupils of different size?
|
Anisocoria
|
|
|
Are spinal nerves LMN or UMN?
|
LMN (somatic)
|
|
|
What is the function of proprioceptive fibers?
|
Sense position of body parts to each other and to the environment
|
|
|
Where are the cell bodies of a UMN and LMN located?
What are axons of upper and lower motor neurons? |
in brain and spinal cord respectively
UMN: brain and spinal c. LMN: periphery |
|
|
What are the motor parts of reflex arcs?
|
LMN
|
|
|
Is musculocutaneous nerve an upper or lower motor neuron?
|
LMN
|
|
|
What is the enlargement of the subarachnoid space between the medulla oblongata and cerebellum?
|
Cisterna magna (cerebellomedullary cistern)
|
|
|
List three clinically significant parts/region of the BRAIN STEM.
|
1. Cranial nerves 3-12
2. vital centers (in medulla which control heartbeat, rate of breathing, coughing, swallowing and diameter of blood vessels) 3. reticular activation system |
|
|
What is the function of the cerebellum?
|
Coordinate movements, maintain equilibrium and maintain posture
|
|
|
Weakness?
Lack of coordination or irregularitys of muscular activity |
Paresis
Ataxia |
|
|
What does the trigeminal nerve (CrN 5) innervate?
|
Sensory to most of the head by the 3 branches, and motor to the muscles of masticulation.
|
|
|
What are the two lower motor neurons of the autonomic nervous system?
|
Preganglionic and postganglionic
|
|
|
How does the ANS differ structurally from the somatic nervous system?
|
2 lower motor (efferent) neurons instead of one
|
|
|
Spacticity? (what is this a sign of)
|
spastic/altered skeletal muscle performance is one of UMN signs (UMN down), also known as ataxia, can be accompanied by paresis (partial paralysis)
|
|
|
Horner’s Syndrome
|
is a clinical syndrome caused by damage to the sympathetic nervous system (e.g. of the eye).
Signs found in all patients on affected side of face include; ptosis (which is drooping of the upper eyelid from loss of sympathetic function), and miosis (constricted pupil), The site of lesion to the sympathetic outflow is on the ipsilateral side of the symptoms. * First-order neuron disorder: Central lesions that involve the hypothalamospinal pathway (e.g. transection of the cervical spinal cord). * Second-order neuron disorder: Preganglionic lesions (e.g. compression of the sympathetic chain by a lung tumor). * Third-order neuron disorder: Postganglionic lesions at the level of the internal carotid artery (e.g. a tumor in the cavernous sinus). If someone has impaired sweating above the waist affecting only one side of the body, yet they do not have a clinically apparent Horner's syndrome, then the lesion is just below the stellate ganglion in the sympathetic chain. Pupillary Light Reflex, Salivation, etc. |
|
|
Cerebral lesions
|
-changed behavior
- seizures - normal gait w/abnormal postural reactions -loss of vision |
|
|
Diencephalon (hypothalmus + thalmus) lesions produce what signs?
|
-cerebral signs (similar)
-autonomic and endocrine abnormalities (e.g. polyuria, polydipsia (excessive thirst), altered sleep patterns also possible |
|
|
Brainstem lesions
|
-decreased levels of consiousness from R.A.S.
-deficits in CN's III-XII as they arise from brainstem -proprioreceptive deficits and gait signs (this gets complicated) |
|
|
Brainstem includes?
|
midbrain, pons, medulla obl.
|
|
|
Cerebellar lesions:
|
-incoordination of mov't (ataxia), initiation tremors, and abnormal mov't of head
-vestibular disease signs: including nystagmus and head tilt |
|
|
preganglionic and postganglionic fibers are associated with thoracolumbar spinal nerves of ____?
|
Thoracolumbar spinal nerves of sympathetic NS
|
|
|
Vestibular system lesions:
|
-affects posture in relation to gravity, eye mov't in relation to head
-head tilt, nystagumus, asymmetric ataxia, w/possibly circling and vestibular strabismus IF central vestibular disease in addition to above will have -paresis/weakness, UMN -depression IF have peripheral disease, besides head tilt with NOT produce UMN signs (NO paresis) -will have postural deficits b/c of balance NOT proprioreceptive disruption |
|
|
Where does PS arise?
|
craniosacral
|
|
|
What is autonomic function of oculomotor nerve?
|
-Motor involuntary/smooth mm. of eye (near focus lens & constrict pupil)
|
|
|
What nerve is required to bear weight on the pelvic limb?
|
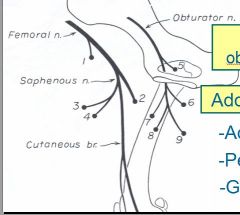
Femoral n. (L4-6) extends the stifle
|
|
|
With what does the vestibular branch of the vestibulocochlear nerve deal ?
With what does the cochlear branch of the vestibulocochlear nerve deal ? |
Special Sensory: equilibrium/ motion
Special Sensory: hearing - so sensory to auditory portion of the inner ear. - core component is the Organ of Corti, the sensory organ of hearing |
|
|
Where are the cell bodies of a UMN and LMN located?
What are axons of upper and lower motor neurons? |
in brain and spinal cord respectively
UMN: brain and spinal c. LMN: periphery |
|
|
What is path of LMN?
|
Leave CNS over VENTRAL roots (only one motor neuron) & spinal n. or cranial n. to periphery
|
|
|
Outline the pathway of the sympathetic innervation to the head.
|
Nerves from hypothalamus (UMN) down cervical cord to lateral (intermediolateral) gray column to T1-T4, preganglionic fibers over communicating branches & up SNS trunk to cranial cervical ganglion; Postganglionic fibers through middle ear, cranial cavity & orbit over CrNs
|
|
|
What are the most clinically important ANS fibers in the head?
|
CrN7 to lacrimal gland & sympathetic to eye (Horner's syndrome)
~see page 483 |
|
|
What are the signs of Horner's Syndrome? Horner's Syndrome
The classic signs of Horner's Syndrome occur on the same side of the face as the injury, and include: |
(1)Small pupil size (miosis) (2)Protrusion of 3rd eyelid
(3)Drooping of upper eyelid (ptosis) (4)Sunken appearance to the eye (enophthalmos) (5)Dilation of blood vessels on affected side of the face, which makes the area feel warmer to the touch >caused by loss of sympathetic innervation to eye, so parasympathetic NS takes over. >eye constrict, muscle around eye go limp |
|
|
General somatic afferent (GSA) carried over what nerves?
|
spinal nerves (body) and CN5 (head)
|

