![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
What is Infective Endocarditis?
|
Infective endocarditis: infection involving the endocardial surface of the heart, most commonly the heart valves.
|
|
|
Describe Acute endocarditis:
|
Acute endocarditis has a rapid fulminant course, and is often fatal within several weeks after onset; affects normal valves.
|
|
|
Describe subacute endocarditis:
|
Subacute endocarditis usually affects previously damaged valves, and may cause symptoms for weeks or months prior to admission.
|
|
|
Epidemiology of endocarditis:
|
*Infective endocarditis is a relatively uncommon infection: accounts for about 1 case/1000 hospital admissions.
*More likely with artificial valves *Overall, over 50% of cases occur in persons over age 50. |
|
|
Predisposing conditions for endocarditis:
|
-Prosthetic heart valves
-Previous infective endocarditis -Intravenous drug use -Degenerative conditions involving heart valves -Hypertrophic cardiomyopathy -Congenital heart disease (& repair) -Rheumatic heart disease -Mitral valve prolapse |
|
|
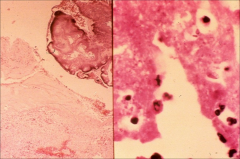
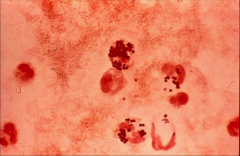
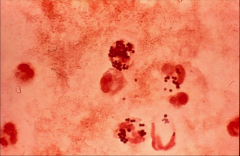
left: strep visible
right: gram neg diplococci (gonorrhea) *both on heart valves |
|
|
Pathogenesis of endocarditis:
|
*Damage due to trauma, turbulence and underlying disease provides a suitable site for bacterial attachment.
*Platelets and fibrin form a thrombus on damaged endothelium. *Transient bacteremia results in colonization of the platelet-fibrin thrombus; Forms a "vegetation." *The vegetation enlarges and growth or organisms proceeds within the thrombus. |
|
|
Describe the deposition of ICs in the development of endocarditis:
|
*Persistent bacteremia leads to septic emboli, formation of immune complexes and formation of rheumatoid factor antibodies.
*Septic emboli can affect any organ; may cause Osler’s nodes or Janeway lesions. *Immune complex deposition may produce focal or diffuse glomerulonephritis, arthralgias, fever, pleuritic pain. |
|
|
What kind of pathology in the heart do you see in endocarditis?
|
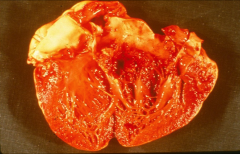
*Valves affected: mitral 85% of cases, aortic 55%, tricuspid 15%, pulmonic <1%.
*Infection may cause perforation of valve leaflets, valve ring abscesses, rupture of chordae tendinae, or disruption of the conduction system. *Occasionally, myocarditis or pericarditis accompany IE. *Myocardial infarction may result if emboli lodge in the coronary arteries. *Vegetations may occlude valve orifice. |
|
|
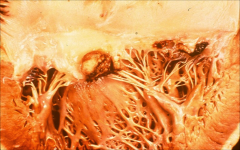
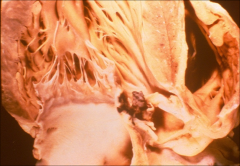
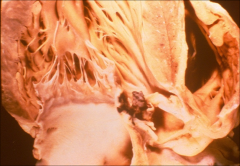
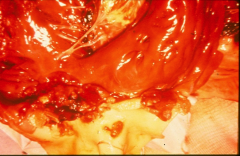
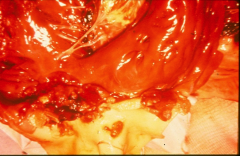
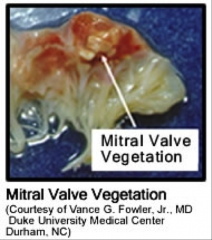
*mitral valve showing large vegetation damaging flow of blood thru the valve.
*Valve itself appears fibrotic |
|
|
*Right sided endocarditis
*pulmonic valve affected |
|
|
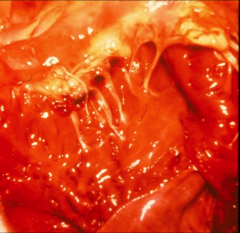
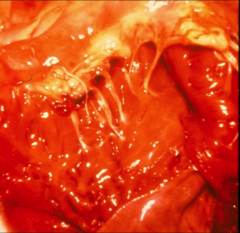
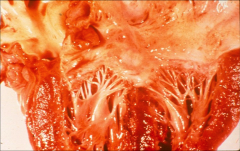
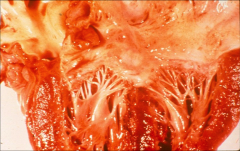
*tricuspid
*a ruptured chordae tendinae |
|
|
*Aortic valve destroyed by staph aureus
|
|
|
*fibrotic valve affected by rheumatic heart disease
|
|

|
-Vegetation is calcified
|
|
|
What kinds of systemic effects do you see related to endocarditis?
|
*Splenic infarctions are common, but are often not diagnosed clinically.
*Renal infarcts; seldom cause renal failure. *Diffuse glomerulonephritis (GN) or immune complex GN may result in renal failure. *Cerebral emboli usually involve the MCA; mycotic (arterial wall) aneurysms may develop. *Pulmonary emboli, infarction, effusions and empyema common with right-sided endocarditis. |
|
|
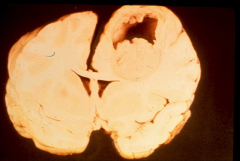
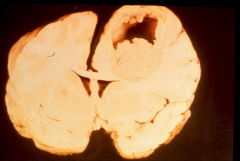
*Brain abscess 2˚ to endocarditis
*Many endocarditis pts (80%) will have SOME kind of brain effects, but this is extreme and uncommon. |
|

|

*mycotic aneurysm
*vegetation visible |
|
|
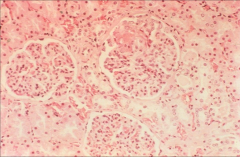
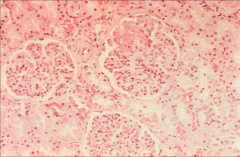
*glomerulonephritis 2˚ to endocarditis
|
|
|
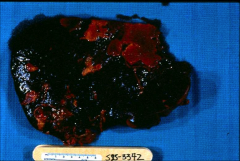
*lighter colored scabs are infarcts to the spleen, 2˚ to endocarditis.
|
|
|
What bugs cause Endocarditis?
|
*Streptococci and enterococci: 40-50% of cases
*Staphylococci: 40-50% of cases *Gram-negative bacilli: 2-10% of cases *Fastidious Gram-negative organisms: (“HACEK”) group and other “Culture-negative” endocarditis (Q fever, Coxiella burnetii) *Gram-positive bacilli: uncommon *Anaerobic bacteria and fungi: uncommon |
|
|
What is the HACEK group?
|
Haemophilus
Aggregatibacter aphrophilus Cardiobacterium hominis Eikenella corrodens Kingella (Kingella kingae) *less common causes of endocarditis |
|
|
Clinical manifestations of endocarditis:
|
*Infective endocarditis often causes fever, anemia, murmur & emboli (FAME).
*Murmur is present in 85-95% of cases. “Changing” murmurs and new murmurs are relatively uncommon. *Fever occurs in 80% of patients. *Chills, night sweats, weight loss and malaise are common. *Arthralgias (including nonspecific back pain) and myalgias are common, and may be chief complaint. *Splenomegaly occurs mainly in subacute form. |
|
|
Describe Embolic phenomena in Endocarditis patients:
|
*Embolic phenomena occur in 25-35% of patients.
-Splinter hemorrhages in 15% of cases. -Petechiae are relatively uncommon. -Osler’s nodes (nodular lesions usually in the finger pads) -Janeway lesions (hemorrhagic skin lesions on palms or soles) -Roth spots (red lesions with a white center, involve the retina) -Cerebral emboli occur in 10-30% of patients. -Major artery emboli due to bulky vegetations more common with fungi and Haemophilus species. |
|
|
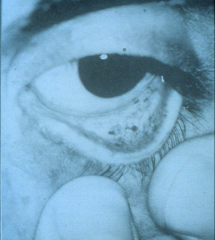
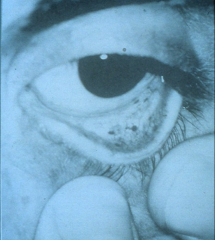
*conjunctival hemorrhage due to endocarditis
|
|

|
*scleral hemorrhage due to endocarditis
|
|

|

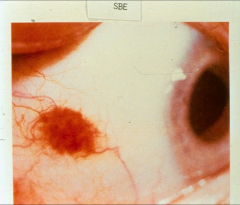
*roth spot in endocarditis
|
|
|
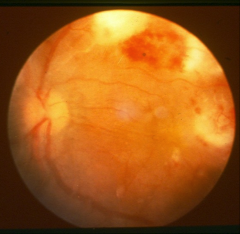
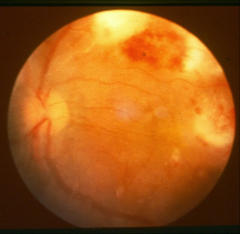
*flame hemorrhages in endocarditis.
|
|

|

*Janeway lesion in endocarditis; subtle
|
|

|

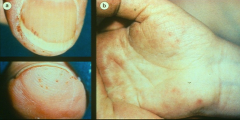
*splinter hemorrhages on left
*osler's nodes on right *both due to endocarditis |
|
|

*left: petechiae, splinter hemorrhages
*right: janeway lesions |
|

|
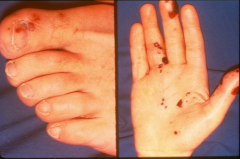
*embolic spots related to endocarditis
|
|

|

*embolic spots related to endocarditis
|
|

|

*clubbing and a splinter hemorrhage
*seen in subacute endocarditis as well as COPD |
|
|
Describe staph aureus left-sided endocarditis:
|
*40% mortality in younger patients; 80% mortality in older persons.
*1/3 of patients will have “normal valves”. *High incidence of complications. -CHF, embolic phenomena, myocardial abscess -Neurological complications |
|
|
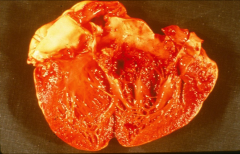
*aortic valve completely destroyed by s. aureus
|
|
|
Describe right-sided endocarditis:
|
*Associated with IV drug use; 75% of infective endocarditis in IV drug users is right-sided, 10% of infective endocarditis in non-IV drug users is right-sided.
*Fever with multiple pulmonary infarcts. *Staph auerus bacteremia. |
|
|
-Staph aureus in right sided endocarditis.
|
|
|
ORGANISMS CAUSING INFECTIVE ENDOCARDITIS IN INTRAVENOUS DRUG USERS:
|
*S. aureus is most common.
*Pseudomonas much more common than in other patients. *Candida and Aspergillus fungi more common than in other risk groups. |
|
|
LABORATORY FINDINGS in endocarditis:
|
*Erythrocyte sedimentation rates are elevated in almost all cases.
*Anemic of chronic disease is present in 70-90% of cases. *Microscopic hematuria is relatively common. *Rheumatoid factor antibodies often present in patients with subacute endocarditis. |
|
|
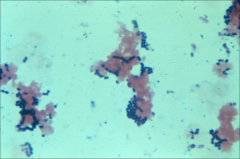
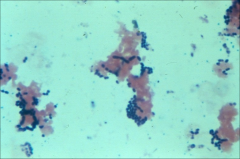
*example of a positive blood culture in endocarditis
*gram + diplococci --> strep |
|
|
How do you diagnose endocarditis?
|
*Blood cultures are the most important diagnostic test for diagnosing infective endocarditis.
*Draw blood cultures before starting empiric antibiotics. *In patients who have not been on antibiotics, 2 sets of timed blood cultures will yield the causative organism in >90% of cases. *Ideally, 3 sets of cultures before antibiotics. |
|
|
Describe the role of echo in diagnosing endocarditis:
|
*Echocardiogram (ECHO) may be useful.
*Sensitivity and specificity for detecting vegetations vary with ultrasound technique used Transthoracic (TTE) Transesophageal (TEE) Sensitivity 60-70% 90-95% Specificity 90-95% 95-98% *Negative predictive value of a single TEE is about 90%. |
|

|

*echo showing a large embolus in endocarditis
|
|
|
LOCAL COMPLICATIONS OF INFECTIVE ENDOCARDITIS:
|
*ECHO can identify perivalvular extension of infection, valvular dysfunction or instability, degree of aortic insufficiency.
*ECHOs are seldom useful if blood cultures are negative (don't screen for no reason; must be suspicious of endocarditis or valve dysfunction first) |
|
|
Therapy for Endocarditis:
|
*Long-term intravenous antibiotics with bactericidal agents required.
*Monitoring the efficacy of antibiotic therapy by determining the MIC of the organism is often necessary. *Surgery is needed in a significant number of patients. |
|
|
When should you perform surgical therapy for endocarditis?
|
*Refractory CHF
*Perivalvular or myocardial abscess, conduction abnormalities on EKG *Fungal endocarditis *More than one serious embolic episode *Persistent bacteremia despite appropriate antibiotics |
|
|
Who should receive prophylactic treatment for endocarditis?
|
*Prosthetic cardiac valve
*Previous IE *Congenital heart disease -unrepaired cyanotic CHD -repaired with prosthetic materials during first 6 months after procedure -repaired with residual defects at site *Cardiac transplantation recipients who develop valvulopathy |

