![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
Common sites |
- heart valves - septal defect - chordea tendinea - mural endocardium |
|
|
Classification |
- acute bacterial E: virulent organisms, days-weeks - subacute bacterial E: low virulence, weeks-months IE on prothesis: early or late prosthetic |
|
|
Characteristic pathological leasion of IE |
-vegetation -composed of platelets -fibrin -microorganisms -inflammatory cells |
|
|
Susceptible host for IE |
- any age but median age onset is 50 - male/female ratio 2:1 - prexisting cardiac condition that affects valves - i.v. drug abusers at high risk (high frequency of tricuspid valve infection cause by Staphylococcus aureus) |
|
|
Risk factors of IE |
-IVDA can be associated with HIV, resolves with antibiotics but reccurance is common -RF -MVP -aortic sclerosis -bicuspid aortic valvular disease -prosthetic valvular heart disease (1/3rd of all cases of endocarditis) occures in 1-3% after valvular heart surgery -intravascular catheter (25% associated with bacteremia caused by S. aureus) -infected surgical wound |
|
|
Pacemaker endocarditis |
•Microorganisms migrate across a broken skin barrier from eroding battery pack or generator pocket wound •early cases: S. aureus •late cases: S. epidermidis |
|
|
Pathology of IE |
• endocardial surfaces previously damaged from VHD, endocarditis, surgery or pacemaker wires provide a favorable enviroment for thrombus formation • overtime microorganisms proliferate in the thrombus resulting in a classic vegetation • small platelet aggregates causes endothelial damage leading to fibrin organization and formation of vegetation = friable masses that may embolise + attachment of microorganisms that multiply rapidly may progress to frank abcess that extend into the valve structure or into the myocardium |
|
|
Signs & symptoms of IE |
- begins as flu-like illnes with dry cough, body aches, fatigue - most patients dont seek advice until fatigue or fever aggrevates or appearance of complications like embolic events or HF |
|
|
Signs & symptoms of IE |
- begins as flu-like illnes with dry cough, body aches, fatigue - most patients dont seek advice until fatigue or fever aggrevates or appearance of complications like embolic events or HF |
|
|
Cardinal manifestations of IE |
- low-graded fewer - night sweats - weight loss |
|
|
Roths spots |
- retinal hemorrhage with pale center - flame shaped hemorrhage - coagulated fibrin, ischemia, inflammation, infection - infective endocarditis - SLE, leukemia, HIV, retinopathy |
|
|
Symptoms of IE |
- mycotic aneurism - heart: infected embolus/clot - kidney: infarction, hematuria - brain: stroke - eye: Roth spots - skin: petechiae, red nodules (Osler’s nodes), purpura (Janeway lesions) - spleen: infarction, abscess - fingernail beds: splinter hemorrhage |
|
|
Symptoms of IE |
- mycotic aneurism - heart: infected embolus/clot - kidney: infarction, hematuria - brain: stroke - eye: Roth spots - skin: petechiae, red nodules (Osler’s nodes), purpura (Janeway lesions) - spleen: infarction, abscess - fingernail beds: splinter hemorrhage |
|
|
Clinical findings in IE |
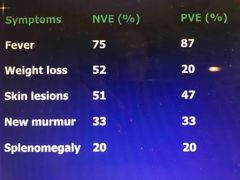
Back (Definition) |
|
|
Symptoms of IE |
- mycotic aneurism - heart: infected embolus/clot - kidney: infarction, hematuria - brain: stroke - eye: Roth spots - skin: petechiae, red nodules (Osler’s nodes), purpura (Janeway lesions) - spleen: infarction, abscess - fingernail beds: splinter hemorrhage - painfull embolic leasions on the fingers or toes |
|
|
Physical findings in IE |
- regurgitant murmur (mitral or aortic) - new or changing murmur (30%) - widening of pulse pressure - bradicardia progressing to complete heart block can be cause by septal abcess, requires open surgical débriderment and drainage - splenomegaly (20%) |
|
|
HIGH suspicion raising criterias of IE |
- new valve lesion - embolic events - sepsis - hematuria - glomerulonephritis - renal infarction - fever |
|
|
Low clinical suspicion of IE |
Fever |
|
|
Duke criteria |
- predisposing factors - blood culture isolates or persistence of bacteremia - ECHO with other lab findings |
|
|
Lab tests of IE |
- anemia - leukocytosis - elevated ESR - abnormal urinalysis (hematuria, proteinuria) - blood culture (+ in 90%) |
|
|
Lab tests of IE |
- anemia - leukocytosis - elevated ESR & CRP - abnormal urinalysis (hematuria, proteinuria, azotemia, high creatinine) - blood culture (+ in 90%) - hypergammaglobulinemia - hypocomplementemia |
|
|
Blood culture in IE |
- positive in 90% of the cases within 2 day period - most important diagnostic test - less sensitive if drawn after abx - obtain 3 sets in first 24h, hold for 3 weeks |
|
|
Major criteria of IE |
- persistent bacteremia - new regurgitant heart murmur - valvular heart disease with vasculitis - negative or intermittent bacteremia with fever - new regurgitant heart murmur with vasculitis |
|
|
ECHO in IE |
- vegetation - abscess - pseudoaneurysm - intracardiac fistula - valvular perforation - new partial dehiscence of prostetic valve |
|
|
Definite IE |
• 2 major criteria • 1 major + 3 minor • 5 minor |
|
|
Definite IE |
• 2 major criteria • 1 major + 3 minor • 5 minor |
|
|
Possible IE |
• 1 major criteria + 1 minor • 3 minor criteria |
|
|
Definite IE |
• 2 major criteria • 1 major + 3 minor • 5 minor |
|
|
Possible IE |
• 1 major criteria + 1 minor • 3 minor criteria |
|
|
Rejected IE |
• firm alternate diagnosis • resolution of symptoms suggestion IE with abx therapy for < 4days • no pathological evidence of IE at surgery or autopsy with abx therapy of < 4 days • does not meet criteria |
|
|
Chest radiography |
- bilateral infiltrates - pleural effusion |
|
|
Osler triad |
- pneumonia - meningitis - endocarditis |
|
|
Beta hemolytic streptococci |
-Occasional cause -Often manifest with major embolic events |
|
|
Beta hemolytic streptococci |
-Occasional cause -Often manifest with major embolic events |
|
|
Streptococcus pneumoniae |
-might manifest with Oslres triad -often associated with alcohol abuse -mortality is extremly high |
|
|
Beta hemolytic streptococci |
-Occasional cause -Often manifest with major embolic events |
|
|
Streptococcus pneumoniae |
-might manifest with Oslres triad -often associated with alcohol abuse -mortality is extremly high |
|
|
Staphylococcus aureus |
-may result severe sepsis syndrome with a fulminating coagulopathy -metastatic foci of infection spread to the brain, lungs, kidneys -high mortality -can be a cause of PVE but not as common as Staphy epidermidis |
|
|
Staphylococcus epidermidis |
-occures within 1y after surgery - results from inoperative contamination by skin bacteria -vascular catheters & surgical wounds are frequent sources -almost always resistant to methicilin or oxacilin |
|
|
Staphylococcus epidermidis |
-occures within 1y after surgery - results from inoperative contamination by skin bacteria -vascular catheters & surgical wounds are frequent sources -almost always resistant to methicilin or oxacilin |
|
|
HACEK stands for |
Haemophilius Actinobacillus Cardiobacterium hominis Eikenella corrodens Kingella |
|
|
Staphylococcus epidermidis |
-occures within 1y after surgery - results from inoperative contamination by skin bacteria -vascular catheters & surgical wounds are frequent sources -almost always resistant to methicilin or oxacilin |
|
|
HACEK stands for |
Haemophilius Actinobacillus Cardiobacterium hominis Eikenella corrodens Kingella |
|
|
HACEK group |
• Group of slow-growing, gram-negative bacteria • 5-10% of community aquired E • can last for months • may be present with painful embolic lesion to an extremity |
|
|
Staphylococcus epidermidis |
-occures within 1y after surgery - results from inoperative contamination by skin bacteria -vascular catheters & surgical wounds are frequent sources -almost always resistant to methicilin or oxacilin |
|
|
HACEK stands for |
Haemophilius Actinobacillus Cardiobacterium hominis Eikenella corrodens Kingella |
|
|
HACEK group |
• Group of slow-growing, gram-negative bacteria • 5-10% of community aquired E • can last for months • may be present with painful embolic lesion to an extremity |
|
|
Fungal endocarditis |
Caused by - prolonged ab use - parenteral nutrition through central vascular catheters - immunocompromized patients - Candida albican/ parapsilosis |
|
|
Coxiella burnetti |
• Q fever endocarditis • patients are in immunosuppressant therapy and have underlying valvular disease |
|
|
Bartonella henselae |
-inf often seen in homeless and alcoholics - blood cultures are negative but serology may be helpfull - identification by polymerase chain reaction (PCR) assay on resected valve tissue has been reported |
|
|
Antimicrobal selection guidelines |
• penicilin + gentamicin is the cornerstone of therapy • vancomycin for penicilin-allergic patients & methiciline-resistant (with gentamicin in first 3-5days) • IV ceftriaxone (Rocephin) + gentamicine [1/d for 2 or 4weeks] good combo • short therapy is not indicated in PVE, major embolic complications, symptoms for longer than 2 months • for relatively penicilin-insensitive Strep (minimal inhibitory conc% is higher than 0.1-0.5mg/mL) • for enterococci peni+genta for 6weeks • for NVE caused by methicilin-susceptible Staphy: oxacilin or cefazolin for 4-6w • PVE Staphy treatment must be more aggressive • IVDA caused by S. aureus responsive to short therapy: IV cloxacilin for 2w • HACEK: ceftriaxone for 4w or ampicilin-sulbactam or ciprofloxacin • fungal E has poor prognosis, surgery + IV amphotericin B (Fungizone) & lifelong antifungals |
|
|
Empirical trial |
1. Ampicilin-sulbactam + gentamicin for NVE 2. Vancomycin + ciprofloxacin + gentamicin for PVE |
|
|
Surgical treatment |
- CHF — agressive surgery - valve failure causing NYHA class III or IV — urgent surgery - endocardial abscess, which can involve aortic root/valve ring/ventricular septum — urgent surgery - vegetations >1cm - major embolic event - failure or relapse |
|
|
Persistent fever causes |
•worrisome during the treatment of IE - annular or ring abcess (requires surgery) - myocarditis - pulmonary emboli - systolic emboli - i.v. catherter sites - drug fever without any manifestation |
|
|
Persistent fever causes |
•worrisome during the treatment of IE - annular or ring abcess (requires surgery) - myocarditis - pulmonary emboli - systolic emboli - i.v. catherter sites - drug fever without any manifestation |
|
|
Neurologic complications |
•common (vexing management dilemma) •anticoagulation should be avoided bcz of increased risk of intracranial bleeding |
|
|
Persistent fever causes |
•worrisome during the treatment of IE - annular or ring abcess (requires surgery) - myocarditis - pulmonary emboli - systolic emboli - i.v. catherter sites - drug fever without any manifestation |
|
|
Neurologic complications |
•common (vexing management dilemma) •anticoagulation should be avoided bcz of increased risk of intracranial bleeding |
|
|
Causes of nezrologic complications |
- stroke - encephalopathy - retinal emboli • brain abcess • mycotic aneurism are infrequent |
|
|
Survival |
• mortality around 20% (bcz of PVE and IVDA) • frequent cause of death is CHF, major embolic events, mycotic aneurism |
|
|
Survival |
• mortality around 20% (bcz of PVE and IVDA) • frequent cause of death is CHF, major embolic events, mycotic aneurism |
|
|
Prevention |
- antibiotic prophylaxis - presumed dental portal of entry in less than 20% of well studied cases - only in higher risk patients - diagnostic studies - drainage of infected spaces where Strep, enterococci or S. aureus are proven or likly pathogens |
|
|
Patients at higher risk for adverse outcomes from Endocarditis |
1. Prosthetic cardiac valve disease 2. Previous IE 3. Congenital heart diseases - unrepaired cyanotic CHD - completely repaired CHD with prostetic materials - incompletely repaired CHD with residual defects at prosthetic patches or devices 4. Cardiac transplantation with vulvular defects |
|
|
Prophylaxis guidelines |
- amoxicillin or ampicillin A:2g P:50mg/kg oral or iv (30-60 mins before procedure) - Clindamycin A:600mg P:20mg/kg oral or iv (30-60 mins before in case of allergy to penicilin) - penicilinase-resistant penicilin (oxacilin/nafcilin) or first generation cephalosporin (cefazolin) in case of drainage ordiagnostic studies - vancomycin for resistant strains MRSA - first or second generation cefalosporin (30mins before) in case of cardiac valve surgery. If the operation is >4h 2nd dose should be given intraoperativly before closure |
|
|
Prophylaxis guidelines |
- amoxicillin or ampicillin A:2g P:50mg/kg oral or iv (30-60 mins before procedure) - Clindamycin A:600mg P:20mg/kg oral or iv (30-60 mins before in case of allergy to penicilin) - penicilinase-resistant penicilin (oxacilin/nafcilin) or first generation cephalosporin (cefazolin) in case of drainage ordiagnostic studies - vancomycin for resistant strains MRSA - first or second generation cefalosporin (30mins before) in case of cardiac valve surgery. If the operation is >4h 2nd dose should be given intraoperativly before closure |
|
|
Factors associated with and increased rate of relapse |
•inadequate ab treatment •resistant microorganisms •polymicrobial inf in IVDA •empirical antimicrobial therapy for BCNIE •periannular extention •prosthetic valve IE •persistent metastatic foci of inf (abcess) •resistance to conventional ab regimens •positive valve culture •persistence of fever at the 7th postoperative day •chronic dialysis |
|
|
Resistant microorganisms |
-Brucella -Legionella -Chlamydia -Mycoplasma -Mycobacterium -Bartonella -Coxiella -Burnetii -fungi |
|
|
Resistant microorganisms |
-Brucella -Legionella -Chlamydia -Mycoplasma -Mycobacterium -Bartonella -Coxiella -Burnetii -fungi |
|
|
Mycotic aneurysms |
All extra-cardiac aneurysms of infective etiology except for syphilitic aotitis - hematogenous seeding of damaged atherosclerotic vessel - associated with endocarditis - affects elderly more male than female - etiology is wide - treatment is surgery & prolonged antimicrobial therapy |
|
|
Resistant microorganisms |
-Brucella -Legionella -Chlamydia -Mycoplasma -Mycobacterium -Bartonella -Coxiella -Burnetii -fungi |
|
|
Mycotic aneurysms |
All extra-cardiac aneurysms of infective etiology except for syphilitic aotitis - hematogenous seeding of damaged atherosclerotic vessel - associated with endocarditis - affects elderly more male than female - etiology is wide - treatment is surgery & prolonged antimicrobial therapy |
|
|
Vessels affected in mycotic aneurysm |
- intracranial - proximal thoracic aorta - pre-existing aortic aneurysm - pseudoaneurysm - infection complicating arterial injury |

