![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
157 Cards in this Set
- Front
- Back
|
Example of something that can cause type 1 , type 2, and type 4 hypersensitivity?
|

penicillin:
T1: if ur allergic T2: penicillin acts as hapten, binds to cell, and you attack ur own cell (autoimmune) T4: if applied topically, again acts as hapten and binds skin proteins; Th1 get's pis sed off and releases cytokines to recruit CTLs |
|
|
During FIP infection (caused by feline corona virus), what determines type of disease animal gets (wet vs. dry form), and whether or not protective immunity develops?
|
Determined by type of IMMUNE RESPONSE infected animal mounts
* with dry form, see mild Th1 response * with wet form, see strong Th2 response, along with intense αB production note: both forms are fatal |
|
|
IgG is in highest conc where?
|
in blood
|
|
|
Which Ab is dominant overall in blood?
|
Often IgM, sometimes IgG
|
|
|
Which Ab made during primary response to antigen? What does this mean diagnostically if present in high concentration?
Which Ab dominates secondary response? |
IgM, often indicates recent exposure
IgG |
|
|
Review question:
what are opsonins? |
proteins that promotes binding of pathogens to phagocytes
e.g. some αβ and complement protein act as opsonins |
|
|
In wet form of FIP why wud strong Th2 response (intense αB production) be problematic?
|
* αB/Ag aggregations adhere to vessel walls
* complexes initiate hypersensitivity rxn or immune complex disease * have inflammation and vasculitis, (vessels are leaky) * high protein and cell.effusion into peritoneal cavity |
|
|
Review question:
Th2 secrete ? |
* Interleukin-4 and-5
stimulate B cell proliferation and antibody secretion… Thus, promote resistance to extracellular pathogens *Think Humoral Immunity when you think of Th2 cells |
|
|
Pentanmeric Ab?
What Ab does not have Fc region? |
IgM
IgM (so will not help with opsinization!!!) |
|
|
Review question:
Th1 secrete? |
IL-2. Activates other T-cells, B cells and NK cells
* Interferon-y: also made by some other cells; activate macrophages primarily and thus promotes cell-mediated response.. Thus, promotes resistance to intracellular pathogens. ~Think CMI when you think of Th1 cells |
|
|
Which Ab's good at triggering complement?
|
IgG, IgM <- best b/c have 5 Fc sites
CC does not get activated until these bind to antigen |
|
|
Review question:
Another name for CD8+ ? Another name for CD4+ ? |
cytotoxic T cell
helper T cell |
|
|
Review question:
What binds Fc part of αβ? |
NK cells, macrophages, neutrophils <- cells of innate immune system have receptor for Fc part of ANTIBODY
(antibodies tag the antigen so these phagocytic can do their job) |
|
|
Review question:
structure of antibodies? |
identical to BCR from parent plasma B cell from which it is secreted, but enclosed in membrane,
2 light chains 2 heavy chains variable region (attaches to antigen) Fc region (attaches to cell e.g. neutrophil) |
|
|
Review question: (erase after midterm)
Endogenous antigen Where made? Processed by? MHC molecule presented with? |
made by intracellular pathogen inside inf.host cell e.g. virus replicates and makes viral protein inside host cell expressing MHC-I
Inf. cell lysed cytotoxic T cell (CD8+) |
|
|
gamma globulin
|
Most significant gamma globulins are immunoglobulins (Ig), aka αB, although some Ig's are not γ-globulins, and some γ-globulins are not Ig's.
|
|
|
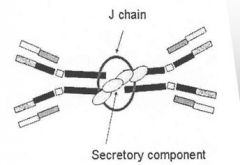
Which αB usually associated with mucosa?
|
Secretory IgA
• Secretory component makes resistant to proteases of GI • Major role is to bind antigen and prevent from binding epithelium – called “Immune exclusion” note: serum IgA is monomeric |
|
|
How many Fc regions does IgA have?
|
• Usually exists as a dimer (J-chain)
|
|
|
Which species have placenta that allows passive transfer of IgG in utero?
|
primate, dog, cat?
|
|
|
Antibody-dependent-cell cytotoxicity (ADCC)
|
The killing of antibody-coated target cells by cytotoxic cells (NK cells usually) with surface Fc receptors for the antibody.
|
|
|
What can mediate lysis of cells, bacteria, viruses, parasites by binding to αB or directly to microrobes (w/o αB)?
|
complement proteins
|
|
|
What can facilitate phagocytosis via opsonization ?
|
complement proteins
|
|
|
What else can complement system do?
|
* induce inflammation in tissue
* promote mast cell degran. * clear immune complexes from circulation and deposits them in spleen and liver |
|
|
How do complement proteins induce inflammation in tissue?
|
* chemotaxis of neutrophils,
* increase vascular permeability, * induce contraction of smooth muscles |
|
|
What is the complement system?
|
* Over 20 diff. proteins in blood
* No cells in the Complement System * With infection, system of molecules is activated leading to sequence of events that ultimately targets surface of pathogens that help to destroy pathogen and eliminate infection. |
|
|
Which αB passes from breast tissue into milk (also found in tears, saliva, & bile)?
|
secretory IgA, dimeric form
* Passes from breast tissue into milk to protect newborn * also crosses mucosal surfaces (gut, urogenital tracts, respiratory for mucosal protection) |
|
|
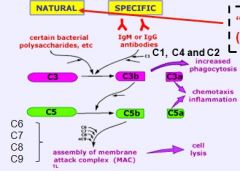
How is complement system activated?
|
Sequence of events referred to as “Complement Cascade”
“Alternate/Natural pathway” vs. Specific/Classical pathway |
|
|
Alternate/Natural pathway
|
* CP activated (w/o αB), so this is example of innate immune response
* bind to microcrobes directly via C3 |
|
|
Lectin Pathway
|
* variation of "alternate pathway" group, again complement cascade activated w/o αB.
* lectin are glycoproteins on surface of microbes to which the complement proteins bind |
|
|
Specific Pathway
|
* requires αB (IgG, IgM) to bind antigen before CC can be triggered
* When Ab is bound to pathogen, Fc region can activate CP (C1) * this is example of specific immune response, so req. prior exposure or happens later in infection |
|
|
Which αB most efficient at triggering CC? Why?
|

IgM b/c has 5 binding sites (Fc) for comp.protein.
(to have IgG activate CC need at least 2 IgG in close proximity) |
|
|
C1 binds to ? (be specific)
what must occur first? |
C1 (complement protein) binds to the constant heavy region or Fc portion of either IgM or IgG (subclasses) BUT only after antibody binds antigen!!
|
|
|
two "forms" of IgM
|
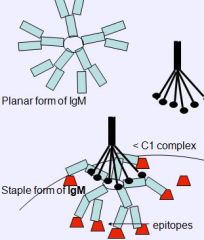
planar form (unbound)
staple form (bound Ag and waiting for C1 to come along) |
|
|
Next CP to bind after C1?
(in specific/active pthwy) |
C3
|
|
|
What happens when complement cascade is activated?
(in specific/active pthwy) *skip until know all other flashcards, because we don't have to memorize individual steps |
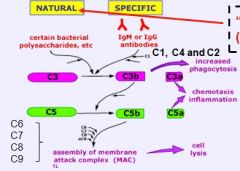
* binding of C1 (becomes enzymatic) allows binding of C3
* C3 bound to complex on pathogen surface * C3 cleaved into C3b and C3a * C3b also activates next step w/C5 blas and is a good opsonin (pro.phag) * C3a (small peptide diffuses away and is a chemtacic factor and promotes inflammation) |
|
|
What is different in Natural/Lectin/Alt. pathway?
(aside from lack of αB) |
C1 not involved, basically C3 binds directly to polysaccharides (e.g. lectin) of bacterial surface
|
|
|
What happens when complement cascade is activated?
|
* Just know that cascade continues and at some point a final complex forms on pathogen surface that causes cell lysis.
* This complex is called the Membrane Attack Complex (MAC) |
|
|
have anaphylatoxin activity, directly triggering degranulation of mast cells as well as increasing vascular permeability and smooth muscle contraction.
|
Both C3a and C5a
(these are complement proteins) |
|
|
How do some bacteria develop resistance or evade the complement system?
|
* Capsule prevents MAC insertion (Streptococcus)
* Capsule prevents C3b deposition (Streptococcus) * Some bacteria possess ELASTASE that inactivates some complement components |
|
|
How do some viruses evade complement system?
|
* Some viruses interrupt CC due to proteins that mimic regulatory proteins
|
|
|
How do some tumor cells evade complement system?
|
* Some tumor cells can endocytose MAC then seal up the membrane
|
|
|
What are the Molecules that bind antigen?
|
MHC
TCR BCR Antibody |
|
|
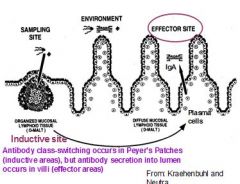
Two categories of mucosal lymphoid tissues:
|
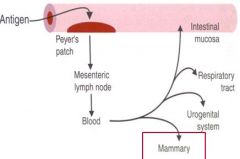
Inductive Sites
Effector Sites |
|
|
Inductive Sites
|
Sites where Ag encountered and immune responses (humoral and CMI) are initiated.
Examples: Tonsils; Appendix; GALT; BALT; Peyer’s patches; |
|
|
Effector Sites
|
Mucosal sites where αβ and cell-mediated responses are carried out… are doing their job (diffuse lymphoid tissues at mucosal surfaces).
|
|
|
Why is it important to distinguish between Inductive Sites and Effector Sites?
(give example of their relationship) |
B/c some B cells may encounter antigen in GI tract, and then release αB in mammary glands (to be secreted into milk); so milk will have αB (primarly IgA inducted at mucosal surfaces) against intestinal Ag and microbes..important to new born.
|
|
|
Where does IgA end up, after newborn has ingested it with milk?
|
Unlike IgG (in colostrum) which is absorbed in blood stream, this IgA remains in GI to protect mucosal surface; this is good thing b/c IgA (mentioned in previous flashcard) is specific for intestinal microbes!
|
|
|
what in meant by immune exclusion?
|
IgA is particularly important in this
- prevents microbes or Ag from binding to mucosa "prevent adherence of bacteria and viruses to epithelial surfaces" |
|
|
Where is IgA made?
How does it get to luminal surface? |
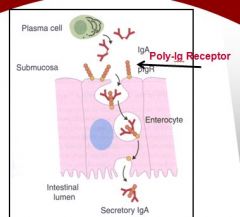
where ever plasma cells are like lymph node, *submucosal surface*
secreted from plasma cell as dimer (attached by J-chain), on submucosal surface have polyimmunoglobulin receptor binds IgA dimer, brings into epithelial cell via pinocytosis, shuttled to luminal surface, released in lumen of GI (still attached to polyiummunoglobulin receptor) |
|
|
What is meant by Secretory Piece?
What is function? |
* Part of the Poly-Ig receptor molecule is cleaved off leaving the receptor peptide chain still attached to the IgA.
* Receptor peptide chain is called the <> * dimeric IgA now known as Secretory IgA and has resistance to proteases |
|
|
What is most important antibody in Immune Elimination? e.g. if it has infected enterocyte or adhered to mucosal lining?
|
Mediated by IgE primarily…
(IgG to lesser extent) If invading organisms evade IgA and gain access to tissues, IgE-mediated responses are triggered. |
|
|
IgE attaches to ____ within walls of intestine, respiratory tract and skin. ..
|
mast cells
|
|
|
What part of IgE binds to mast cell?!
|
Fc region of the antibody attaches to the mast cell
|
|
|
Mast cell is part of what immune system?
|
innate
|
|
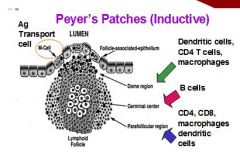
Peyer's patches would example of ?
|
Inductive Sites
|
|
|
exception to the rule that antibody does not get into cells
|
* B/c IgA is transported through enterocytes, it can act inside these cells
* can bind viral proteins inside these cells and interrupt viral replication. * example of antibody acting in an intracellular location. |
|
|
Rapid degranulation of mast cells with release of ____ into the tissues leading to ______(3)?
|
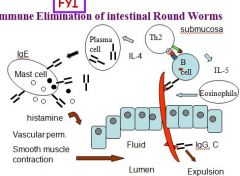
Rapid degranulation of mast cells with release of into the tissues leading to:
inflammation, increased vascular permeability, fluid leakage between enterocytes and thus fluid entering the lumen. ~ goal if for parasite to disengage and be flushed out. |
|
|
Antibody dependent cell cytotoxicity (ADCC)
Killer cells that have Fc receptors (monocytes, eosinophils, neutrophils, NK cells) to bind Ab...what class Ab? |
Mainly IgG, also IgA
|
|
|
What is part of Ab that determines its biological class?
What determines specificity? |
Fc (Fc region of IgA diff. from Fc region of IgG)
Fab |
|
|
Which part of Ab known as constant region?
What part of Ab determines class of Ab (e.g. IgG, IgE)? |
Fc
Fc |
|
|
Example of protective immunity without sterile immunity (without completely removing antigen)?
|
HIV, Ag bound up but not completely removed
|
|
|
Can compliment proteins bind Fc region of Ab?
|
Yes (what does this is trigger)
|
|
|
What is cells present in germinal center of Peyer's patches?
|
B cells
|
|
|
Which Ab present in highest conc. in colostrum?
Does it contain other antibodies? |
IgG (to lesser extend IgA, IgE present)
|
|
|
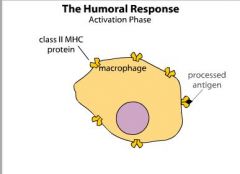
What are the two routes of B-cell activation by antigen?
|
T-dependent activation
T-independent activation |
|
|
Are T-dependent antigen usually big or small?
Why are they T dependent? |
small, soluble antigen
Require T cell to fully activate B cell |
|
|
Type of antibody B cells makes depends on types of cytokines it gets from T helper cells:
Which T cell directs B cell towards more cell mediated response? |
Th1 cell , get Ab to help mostly with cell mediated response, e.g. involve mostly opsonization, etc
|
|
|
What Ab made by T independent antigen?
What type immune response? What absent? |
IgM only, short lived
only primary immune response, no secondary (or memory) response, NO class switching |
|
|
What type of hypersensitivity reactions does IgE mediate?
|
Type I hypersensitivity reactions
|
|
|
If class switching occurs, what changes about antibodies B cell will make?
What drives class switching? |
Fc region
cytokines and repetitive |
|
|
Th1 cytokines (IFN-gamma, IL-2) will primarily cause which classes of antibody to be made?
|
IgG
IgM |
|
|
Th2 cytokines (IL-4, IL-5, IL-6) will primarily cause which classes of antibody to be made?
|
IgE
IgA |
|
|
Titer measures ?
|
total Ab in blood
|
|
|
Lag phase in primary response? Why slow?
|
primary response slow, hasn't seen Ag before, B cell has to proliferate and differentiate
|
|
|
phase characterized by rapid increase in production of Ab, because plasma cells have proliferated
|
Log phase
|
|
|
What changes in secondary immune response?
|
lag phase shorter
log phase higher, longer |
|
|
Antibody secretion into lumen occurring in the villi is an example of what kind of site?
|
Effector site
|
|
|
What receptor does dimeric IgA bind to on the basal surface of the enterocytes?
|
Poly-Ig receptor
|
|
|
What part of the Poly-Ig receptor chain is cleaved off and still attached to the IgA when it enters the lumen? What is this IgA called?
|
Secretory piece
Secretory IgA |
|
|
What antibody mediates immune elimination?
|
IgE
|
|
|
Which antibody is 65-90% of total antibody content in most major domestic animals?
|
IgG
|
|
|
In pigs and horses what is the dominate antibody in milk?
|
IgA
|
|
|
When is the optimal time for absorption of antibodies from colostrum?
|
First 6 hours
|
|
|
What are some reasons of failure of passive transfer of antibodies in newborns?
|
Production failure
Ingestion failure Absorption failure |
|
|
What are some ways that antibody in the serum of the neonate can be evaluated?
|
Salt precipitation or Turbidity tests
Measure total serum protein ELISA Radial immunodiffusion |
|
|
How does radial immunodiffusion work?
|
Precipitation ring (serum immunoglobulin reacts with anti-equine immunoglobulin)
|
|
|
How long should treatment of failure of passive transfer in the neonate be treated?
|
3 weeks
|
|
|
What is the earliest age to vaccinate a puppy or kitten with reasonable expectation of a response?
|
Between 6 and 9 weeks
|
|
|
When should you vaccinate calves and foals?
|
Before 6 months (about 4 months0
Re-vaccinate at 6 months or after weaning |
|
|
What Ab most numerous in ruminant milk?
|
1. IgG!!!! = ruminant milk
2. IgA 3. IgE |
|
|
What Ab dominant in non-ruminant milk?
|
1. IgA = non-ruminant milk!!
2. IgG 3. IgE |
|
|
How does neonate internalize IgG present in colostrum?
|
* Maternal IgG binds to Fc Receptor (FcRn) on intestinal epithelial cells of newborn
* Internalized by pinocytosis * FYI enters lacteals (lymphatic cap.) and intestinal capillaries |
|
|
Why can't neonate take up IgG after 24 hours?
|
After 24 hours a new layer of enterocytes form that prevent absorption because they lack FcRn
|
|
|
FIP causes what type of hypersensitivity?
|
Type III
|
|
|
Which types of hypersensitivities are mediated by antibody?
|
Type I, II, III
|
|
|
Which types of hypersensitivities are mediated by T-cells?
|
Type IV
|
|
|
What is a genetically determined predisposition to develop clinical (type-1) allergies?
|
Atopy
|
|
|
What is an immediate (type1) hypersensitivity reaction?
|
Allergy
|
|
|
What type of allergic reaction is caused by contact with antigen against which the host has pre-existing IgE antibody for?
|
Type I hypersensitivity
|
|
|
What are some products released by mast cell granules in type I hypersensitivity reactions?
|
Histamine
Heparin |
|
|
What are the two distinct inflammatory reactions that may occur in type I hypersensitivity reactions?
|
Early phase
Late phase |
|
|
What phase of (type I) inflammatory reactions occur within 10-20 mins of repeat exposure, mediated by histamine and heparin, and sometimes called the "wheel and flare" (on skin!) phase?
|
Early phase
~inhibits clotting allergist does instigates early phase of type I H.S. |
|
|
What phase of inflammatory reaction peaks at 6-12 hours, associated with redness, edema, mucus production and pruritis, and is mediated by chemotactic factors from mast cells?
|
LATE PHASE: this is much more SEVERE swelling that occurs later
e.g. after Walter ate nuts, severe smooth muscle contraction in respiratory tissue e.g. Asthma attacks |
|
|
What type of hypersensitivity reaction is asthma?
|
Type I hypersensitivity
|
|
|
What is the meaning of a "localized" type I reaction?
|
Localized to one organ system
|
|
|
Type I hypersensitivity is mediated by what antibody?
Key cell involved? |
IgE
Mast cell Also basophil, eosinophils |
|
|
Which animals mainly show liver signs in anaphylactic shock?
|
Dog
|
|
|
What is usually the cause of an allergic reaction when given vaccines?
|
Aluminum adjuvants
(acts as hapten?) |
|
|
In Type I hypersensitivity, ___ trigger B cells to make IgE which is inappropriate response for these condition.
|
In Type I hypersensitivity, TH2 cells trigger B cells to make IgE which is inappropriate response.
|
|
|
What is a type of skin rash consisting of red, edema, plaque-like eruptions which are often pruritic (itchy)?
|
Urticaria (hives), route of entry does not always indicate system involved in the response
|
|
|
What are some diagnostic tests used for Type-I allergies?
|
Measure total IgE in serum
Measure patient IgE specific to suspected allergen Intradermal skin test |
|
|
What are some treatments of allergic reactions?
|
Inhibit mast degranulation and effects
Inhibit histamines Corticosteroids Anti-IgE antibody to neutralize the IgE Hyposensitization |
|
|
What type of hypersensitivity response is mediated by IgG or IgM?
|
Type II Hypersensitivity
|
|
|
Are Type II hypersensitivity reactions cytolytic?
|
Yes
|
|
|
What type of hypersensitivity reaction may cause agglutination or hemolysis or stimulate opsonization and phagocytosis of the cells?
|
Type II hypersensitivity
|
|
|
What are some examples of type II hypersensitivity reactions?
|
Transfusion reactions
Hemolytic disease of Newborn (neonatal isoerythrolysis) Immune-mediated cytopenias |
|
|
Are Immune-mediated cytopenias (and Type II HS reactions) a product of autoimmune OR non-autoimmune problem?
|
Immune-mediated cytopenias can be caused by either
Hemolytic disease of Newborn (neonatal isoerythrolysis) is not autoimmune, b/c it's mother's Ab that is causing the problem. |
|
|
What type of hypersensitivity reaction may cause agglutination or hemolysis or stimulate opsonization and phagocytosis of the cells?
|
Type II hypersensitivity
|
|
|
If IMMUNE-COMPLEXES of type III hypersensitivity rxn form in TISSUES, what kind of type is it?
|
Local Type-III
|
|
|
What are the two types of type II hypersensitivity reactions?
|
Primary type II HS reaction
Secondary type II HS reaction |
|
|
What kind of type II HS reaction is an AUTOIMMUNE disease, where animal makes Ab to surface antigens of RBCs, platelets, or other cells?
|
Primary type II HS reaction
|
|
|
What type of type II reaction is when Ab are made to DRUG treatment or an infectious agent?
|
Secondary
|
|
|
What is a diagnostic test for an immune-mediated hemolytic anemia?
What would positive Coombs look like? |
Coombs Test
tests for Ab bound on surface of RBC - if Ab coating RBC, have a hemolytic situation - if positive, will see agglutination |
|
|
If an immune-mediated cytopenias (low RBC) is primary how would you treat it?
|
Immunosuppressive drugs
|
|
|
If an immune-mediated cytopenias (low RBC) is secondary how would you treat it?
|
Treat for underlying condition
|
|
|
What is the cause of a type III hypersensitivity reaction?
|
Formation of immune COMPLEXES b/t antibody (IgG or IgM) and SOLUBLE antigen
|
|
|
Which antibody is usually involved in type III hypersensitivity reactions?
|
IgG
|
|
|
If the complexes of a type III hypersensitivity reaction form in the tissues what kind of type is it?
|
Local Type-III
|
|
|
If the complexes of the a type III hypersensitivity reaction form in the circulation what type is it?
|
Generalized Type-III
= Ab-Ag complex in blood vessel ! |
|
|
What are the three mechanisms of Type-III hypersensitivity reactions?
|
Immune complex formation
Immune complex deposition Immune complex-mediated inflammation |
|
|
What are some examples of Localized type-III reactions?
|
Arthus reaction
Blue eye Heaves in horses ~localized occurs in TISSUE |
|
|
What are some examples of generalized type-III reactions?*
|

Serum sickness
Glomerulonephritis Streptococcus equi note: generalized type III are those that occur in circulation, and for whatever reason complexes frequently accumulate in vessels of kidney and joints |
|
|
How do you treat immune complex conditions?
|
* treat underlying condition (pathogen)
* suppress immune system (glucocorticoids & cyclophosphamide) |
|
|
What is a reaction to IV-injected proteins (usually in antiserum) derived from another species e.g. horse serum?
What type of hypersensitivity is this? |

Serum sickness - get major Ab-Ag complexes forming in vessels
* this is generalized type III h.s. rxn |
|
|
What do the lesions in serum sickness coincide with?
|
formation of large amounts of immune complexes in circulation
|
|
|
What is most of glomerulonephritis in our domestic animal species due to?
|
Immune complex disease
|
|
|
What is a hemorrhagic area in the skin?
|
Purpura
|
|
|
What is a purpura hemorrhagica due to reduction in circulating blood platelets?
|
Thrombocytopenic purpura
|
|
|
What type of purpura is the the purpura hemorrhagica associated with Strep equi?
|
Non-thrombocytopenic purpura
|
|
|
What are the general components of any Type-IV hypersensitivity?
|
Antigen sensitized Th1 CD4 lymphocytes and CD8 lymphocytes
Th1 cytokines Activated macrophages Response peaks at 72 hours |
|
|
What type of antigens are associated with Delayed-type (type IV) hypersensitivity?
|
Insect venom (proteins)
Mycobacterial proteins |
|
|
What type of antigens are associated with Contact-hypersensitivity (type IV)?
|
Haptens
Pentadecacatechol (poison ivy) Small metal ions (nickel and chromate) |
|
|
How does the new in vitro TB test work?
|
Based on the ability of mycobacterium tuberculosis antigens to stimulate host sensitized lymphocyte production of IFN-γ
If memory CD4 Th1 present are sensitive to Tb Ag, will proliferate and produce INF-γ which test will detect !!! |
|
|
What kind of type IV hypersensitivity reaction involves haptens binding to skin proteins?
|
Allergic contact dermatitis
|
|
|
How should allergic contact dermatitis be treated?
|
Avoid contact with chemical or substance
Anti-inflammatory drugs such as Glucocorticoids Antibiotics if secondary infection |
|
|
What is the mechanism behind HOST vs graft rejection?
|
Due to reaction against MHC molecules expressed by the tissue graft
|
|
|
What is the mechanism behind GRAFT vs host rejection?
|
Foreign lymphocytes in the transplanted bone marrow destroy cells and tissues of the recipient
|
|
|
Why may a graft from a male into a female be rejected?
|
HY antigen expressed by male Y chromosome (observed in skin grafts)
|
|
|
Ag like pollen, ragweed instigating hypersensitivity is example of what type?
|
Type I w/ IgE
|
|
|
Type of Ag that might trigger type 2 HS rxn?
|
Ag on surface of RBC's
|
|
|
ADCC is part of what type HS?
|
Type II HS
|
|
|
Heparin (chemical mediator causing type 1 hypersensitivity) causes what?
|
inhibition of clotting
|
|
|
Histamine causes what?
(aside from inflammation) |
- vasodilation
- smooth muscle contraction |
|
|
Is bee sting type 1 hypersensitibity?
|
No, that's just irritant
|
|
|
hapten
what type H.S. involved in? |
too small to cause immune response alone, so binds to larger protein (e.g. albumin) or cell and triggers immune response that way
> can cause type 2 or 4 hs.rxn |
|
|
What is Arthus Reaction?
(give example and describe what happens) |
Arthus reaction e.g. tetanus toxoid vaccine causes Type III hypers.
* If give subQ inj. into animal that already has Ab to antigen, can form complexes (usually IgG), then acute inflammation will develop, CC (Ab-dependent pathway aka specific/classical) |
|
|
Blue Eye in dogs
|
causes localized type III h.s. rxn
*some dogs infected with canine adenovirus type 1 or vaccinated with modified live CAV type 1 vaccine. Lesion: anterior uveitis leading to corneal edema and opacity. * Virus-antibody complexes, neutrophils present in lesion. |

