![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
7 Cards in this Set
- Front
- Back
|
What is tolerance? Why is it important?
|
Tolerance - is the specific immune unresponsiveness to an antigen that is induced by previous exposure of lymphocytes to that antigen
-a molecule inducing tolerance is a tolerogen -it is important in the discrimination between self & non-self -the failure of tolerance to self-molecules leads to autoimmunity |
|
|
What are the 2 levels of immune tolerance?
|
❤CENTRAL TOLERANCE:
-occurs during thymic education, T cells that react with antigens present before birth are deleted (also those that do not have any affinity with self MHC) -this is done via negative & positive selection -central tolerance is not sufficient because not all self molecules are present at birth (ie. mammary tissue) -yet these are not rejected & this is explained by peripheral tolerance & the danger signal hypothesis eg. pathogens and damaged tissues have molecules that signal to the immune system that there is something going on (e.g. Toll-like receptors) ❤PERIPHERAL TOLERNCE: -loss of T & B cell function after exposure to antigens in the absence of mandatory co-stimulatory signals (e.g. B7-CD28 binding), or following exposure to cells lacking major histocompatibility complex (MHC) class II molecules -leads to anergy or inactivation of the cell -the induction of co-stimulatory molecules is dependent on the presence of "danger signals" such as those provided by recognition of pathogen associated molecules by toll like receptors -in addition regulatory T cell - T cells that suppress the immune response of other cells -regulatory T cells are a range of specialized cells that inhibit the immune responses -the most important one is the natural T reg cell, which expresses CD4+, CD25+, and Foxp3+ |
|
|
What factors contribute to autoimmunity?
|
❤Genetic predisposition: some individuals are more prone to autoimmunity than others, in general terms if one is predisposed to autoimmune disorder one is likely to be predisposed to several autoimmune diseases
❤Environmental stimulus - the presence of foreign antigens that cross react with self antigens can trigger autoimmunity (ie. these antigens share some characteristics with the body's own molecules) ❤Breakdown in immune regulation - for autoimmunity to occur there has to be some defect in the immune regulation leading to the presence of auto-reactive immune cells -these cells will attack the organ that expresses the antigen and likely succeed in its destruction over time |
|
|
What are some treatments for autoimmunity & specific examples?
|
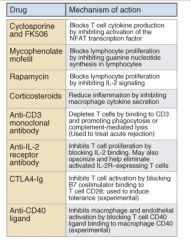
❤Rapamycin: blocks IL-2 signalling
❤Anti-CD3 antibodies: deplete T cells ❤Anti-IL-2 antibodies - inhibit IL-2 effect ❤Cyclosporine: blocks cytokine production by T cells |
|
|
What antigens do tumor cells express?
|

❤Mutated self: Self proteins have been mutated and are not seen as self any longer
❤Oncogene products: Oncogenes encode proteins that transform normal cells into tumor cells. Since these are generally not produced in normal cells they can be seen by the immune system as non-self ❤Over-expression of self proteins: Tumor cells can express self antigens at a very high level and become a target for the immune system ❤Oncogenic viruses: Some tumors are the result of viral transformation and carry remnant of the original virus. These viral proteins can be recognised by the immune system leading to the destruction of the tumor cell. |
|
|
How do tumor cells evade the immune system?
|
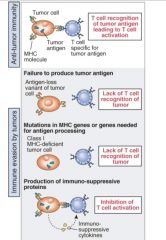
❤Loss of antigen recognized by the immune system: If the molecule is not essential for cell survival and a variant develops by random mutation, this variant will be selected and the tumor will develop
❤Loss of MHC class I: By reducing the amount of MHC class I on its surface, tumor cells can avoid recognition by T cells ❤Production of Immunosuppressive proteins by tumor cells |
|
|
How can we combat tumors?
|

❤Pulsing or transfecting dendritic cells with tumor antigens will increased the immunogenicity of poorly immunogenic tumor antigens. Once activated, T cells have been generated that may recognise the very low amounts of tumor antigen present on the tumor cells
❤Transfect the tumor cells with B7 and IL-2 encoding genes. The B7 molecule will provide the costimulatory signal to the T cells (interaction with CD28), while the IL-2 will help the T cell proliferation |

