![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
What specifically is the first line of defense against microbial invasion? (not just the type of immune system, but the mechanism also)
|
Acute inflammation is the first line of defense in the innate immune system
|
|
|
How long does it take a single bacteria to double?
|
40-50 minutes
|
|
|
What is the function of inflammation? (2)
|
Inflammation provides a mechanism by which defensive cells and molecules are focused rapidly at sites of microbial invasion.
After eliminating the invaders, they initiate tissue repair. |
|
|
In what three ways do microbial invasions stimulate proliferation of mast cells and macrophages?
|
Through TLRs. Through tissue damage that results in lysed cells and neuronal stimulation (pain), both of which stimulate macrophage and mast cells.
|
|
|
How are invaders recognized by the immune system?
What general term is used for host cells that recognize them? |
PAMPs - pathogen associated molecular patterns
Unique molecules present only on microbes, not on animal tissues. Sentinel cells recognize PAMPs |
|
|
What are examples of PAMPs? (7 - 5 bacterial; 2 - viral)
|
Lipopolysaccharide (LPS) (endotoxin) of gram-negative bacteria
Lipoteichoic acids of gram-positive bacteria Glycolipids of mycobacteria (Tuberculosis) Flagellin of bacterial flagella Bacterial DNA (CpG islands) Viral double stranded RNA (dsRNA) Small antiviral molecules |
|
|
What are examples of sentinel cells? (3)
Through what mechanism do they recognize them? |
Macrophages, dendritic cells, mast cells.
The toll-like receptors recognize the PAMPs. |
|
|
What is the function of the toll-like receptors?
|
These receptors on the sentinel cells recognize the PAMPs and trigger inflammation by "turning on" the acquired immune system.
|
|
|
How many toll-like receptors are there?
|
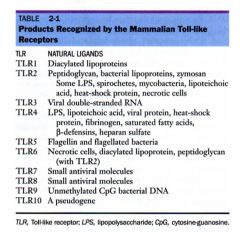
10
|
|
|
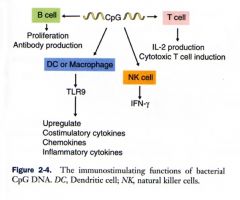
which TLR binds to LPS?
|
TLR4
|
|
|
Which TLR binds to dsRNA?
|
TLR3
|
|
|
Which TLR binds to flagellin?
|
TLR5
|
|
|
What ligand-binding mechanism do TLRs turn on? What are the effects of that?
|

When TLRs bind to PAMPs, they activate NF-kB (nuclear factor kappa B). This is like turning the key to start the cellular machinery.
TNFa and IL-1 are produced to make inflammation. Nitric oxide is produced to kill the bacteria. |
|
|
What four TLRs activate the NF-kB pathway?
|

TLR2, TLR4, TLR5, TLR9
|
|
|
What TLR binds to CpG bacterial DNA?
|
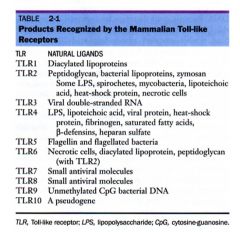
TLR9
|
|
|
What TLR binds to mycobacteria and lipteichoic acid?
|
TLR2
|
|
|
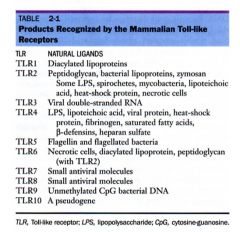
Why is CpG DNA commonly included in vaccinations?
|
CpG is a bacterial DNA that stimulates T cells, B Cells, NK cells, and Macrophages.
(CpG is a PAMP) |
|
|
What is a receptor that is like TLR? What is the difference?
|
Nucleotide-binding oligomerization domain (NOD)
it picks up intercellular bacteria, the only difference is that the receptor is intracellular |
|
|
What's the difference between a monocyte and a macrophage?
|
Monocytes are in the blood, macrophages are in the tissues.
Monocytes have bean-shaped nuclei. |
|
|
Why do some pathogens target monocytes? what are some examples?
|
Monocytes travel through the blood and systemically distribute, in this way, the pathogen can rapidly spread.
Many retroviruses, like FIV and canine distemper, and bacteria, like TB, do this. |
|

What is the round structure at the top of this slide?
|

A phagosome of a macrophage.
|
|
|
What are macrophages called in their different locations?
|
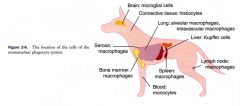
Brain: microglial cells
CT: histiocytes Blood: monocytes Liver: Kupffer cells Lung: alveolar cells All else: macrophages |
|
|
Where are mast cells found? What is their function?
|
Connective tissue, skin, around nerves, under mucosal surfaces
They are very important in immune/inflammatory response |
|
|
What inflammatory response cells are responsible for making you itch? Why?
|
Mast cells
|
|
|
How many types of mast cells are there? What are the differences?
|
Two - mucosal and connective tissue. Mucosal mast cells are small and live about 40 days.
Connective tissue mast cells are bigger and live more than 6 months. |
|
|
How do mast cells cause anaphylactic shock?
|
All mast cells have IgE antibodies. If they are triggered, then they result in a rapid degeneration and release of cytokines. In the lungs (or liver - dog), where the connective tissue mast cells are, they are large and numerous and the rapid degeneration in the vital organ can cause anaphylactic shock. The mucosal mast cells, in the skin are smaller and fewer, and the rapid degeneration only results in itchiness.
|
|
|
What are the three products of sentinel cells?
|
Cytokines, chemokines, vasoactive molecules
|
|
|
What are cytokines?
|
Released by sentinel cells, these are the communicators between cells - proteins that mediate cellular interactions and regulate cell growth and secretion.
|
|
|
What are chemokines?
|
Released by sentinel cells, these are special kind of cytokines that attract neutrophils to sites of damage through chemotaxis. They regulate the emigration of leukocytes from blood to the tissues.
|
|
|
What are vasoactive molecules?
|
Released by sentinel cells, these molecules affect blood vessel walls through changing permeabilities or dilation.
|
|
|
There are going to be many cytokines that we'll learn about. What are the three biggies that he mentioned?
|
TNFa
IL1 IL6 |
|
|
Which cytokines are released by macrohpages? Which by mast cells?
|
Macrophages release all TNFa, IL1 and IL6.
Mast cells release TNFa and IL6. |
|
|
What are the local effects of TNFa?
|
Causes the cardinal signs of inflammation: heat, swelling, pain and redness
|
|
|
What are the system effects of TNFa?
|
Activates leukocytes, enhances toxic effects, and inflammation.
|
|
|
What are the effects of IL1 and IL6?
|

Mediate inflammation, acquired immunity, acute-phase reaction and septic shock. Really, more effects than he described.
|
|
|
What sort of things stimulate the release of IL1? (6)
|

Cell adherence
Inflammatory agents Cytokines Organisms Lectins Immune complexes |
|
|
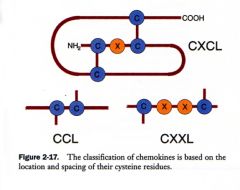
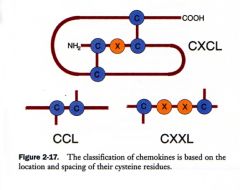
How many classes of chemokines are there? What are the differences between them?
|
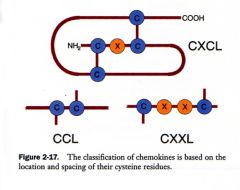
4
They are distinguished by the spacing of the cysteine residues. |
|
|
What is the function of IL8? What is IL8? What else is IL8 known by?
|
IL8 is a chemokine, it is also known as CXCL8. Its function is to attract and activate neutrophils.
|
|
|
What are CC chemokines?
|
They are chemokines that act predominantly on macrophages and dendritic cells (to attract them).
|
|
|
What leukocytes contain vasoactive molecules?
|
Mast cells
|
|
|
What are the important molecules of vasoactive molecules? (6)
|
Histamine and serotonin, primarily.
They also have vasoactive lipids: leukotrienes and prostaglandins and vasoactive polypeptides: anaphylatoxins and kinins. |
|
|
What is a major important source of vasoactive molecules?
|
arachidonic acid
|
|
|
What are the cardinal signs of acute inflammation?
|
Redness, heat, pain, swelling
|
|
|
What causes the heat of inflammation?
|
vasodilation, from vasoactive factors, from tissue damage.
|
|
|
What causes the redness of inflammation?
|
vasodilation, from vasoactive factors, from tissue damage.
|
|
|
What causes the pain of inflammation?
|
Vasoactive factors from tissue damage
|
|
|
What causes the swelling of inflammation?
|
Increased vascular permeability from vasoactive factors from tissue damage and emigration from neutrophi margination triggered by tissue damage.
|
|
|
Where do corticosteroids block the inflammation pathway?
|

They block way up top at the phospholipase step. This is why corticosteroids have so many (and some unwanted) side effects.
|
|
|
How do corticosteroids block the immune system?
|

Corticosteroids block the release of NFkB, which is necessary for long-term immune system function.
|
|
|
Where do NSAIDs block the inflammation pathway?
|

At the cyclooxygenase step
|
|
|
Where does singulair block the inflammation pathway?
|

At the leukotriene step.
|
|
|
What 3 cytokines cause sickness behavior?
|
TNFa, IL1 and IL6
|

