![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
1. What is the significance of Plasmodium (Malaria) having 2 hosts?
2. What are the 4 species of Plasmodium and how can you tell them apart? |
1. Both sexual and asexual reproduction
2a. P. vivax (benign tertian) 2b. P. ovale (benign tertian) 2c. P. malariae (Quartan or malarial) 2d. P. falciparum (Malignant tertian) 2e. Each species has a different number of hours b/w each cycle of clinical disease |
|
|
1. What is the host for sexual reproduction (Gametogeny) of Plasmodium?
2. What is the host for asexual reproduction (schozogeny) of Plasmodium? 3. What disease does Plasmodium cause? |

1. Sexual Repro - Anopheles Mosquito
2. Asexual Repro - Humans/Animals |
|
|
1. Would malaria exist without mosquitos? Why or why not?
2. Why do we not have malaria in the US currently? |
1. No. Mosquitos are necessary for SEXUAL REPRODUCTION (gametogeny). The human host is not suitable for this.
2. Anophales Mosquitos cannot survive in US climate conditions |
|
|
Where is each Plasmodium species predominant, geographically?
What is a common co-infection for P. falcifarum and what does it lead to? |
P. vivax - Bangladesh, Central America, India, Pakistan, Sri Lanks
P. ovale - Africa (less common species) P. malariae - most malarious areas P. falcifarum - Tropical and Subtropical regions - Co-infection with HIV is common there --> Severe Malaria |
|
|
How can Plasmodium (malaria) be transmitted?
|
1. Mosquitos
2. Transfusions 3. Sharing needles 4. Vertical Transmission - Pregnant woman to fetus |
|
|
What are the 3 cycles that Plasmodium goes through in reproduction?
1. In Mosquito 2. In Human Part I 3. In Human Part 2 |
1a. Gametes are taken up into the gut of the mosquito from the blood of an infected individual
1b. Gametes go through sexual reproduction and morphological changes of the Oocyst 1c. Sporozoites are produced 2a. Mosquito injects Sporozoite 2b. Sporozoite infects Hepatocytes 2c. Changes to produce Schizoint 2d. Hepatocyte ruptures and releases Mirazoites into the blood 3a. Mirazoites infect RBCs 3b. Undergo changes: Mirazoite --> Ring --> Mature Trophozoite --> Schizoint 3c. Cell ruptures and releases Mirazoite (Repeat) OR immature Trophozoites will develop into M and F gametes 3d. Gametes flow through blood 3e. Female Anopheles Mosquito takes a blood meal and takes up gametes |
|
|
1. How does a Sporozoite of Plasmodium (malaria) get into the Hepatocytes?
2. How long does the liver stage last? 3. What is the implication of the length of the liver stage, medically? |
1. It has a circumsporozoite protein (CSP) that binds Heparan Sulfate Proteoglycans (HSPG) on hepatocytes
2. 2 weeks 3. You have to stay on antimalarials for 2 weeks after leaving a malaria zone |
|
|
1. What is a Hypnozoite?
2. Why are these made? 3. What happens when the disease relapses? 4. What is the medical implication concerning Hypnozoites and their timespan? |
1. Dormant phase of P. vivax and P. ovale
2. Some sporozoites don't immediately undergo asexual replication 3. Hypnozoites reactivate and undergo schizogeny for up to a year 4. You cannot give blood for 1 year after leaving a malaria zone because of the possibility of having Hypnozoites in your system |
|
|
1. What is Recrudescence?
2. Which Plasmodium species does this apply to? 3. What is the medical implication of Recrudescence? |
1. The situation in which parasitemia falls below detectable levels and then later increases to a patent parasitemia
2. P. vivax and P. ovale 3. Makes it difficult to tell if you're actually infected |
|
|
1. What is the function a Mirazoite Surface Protein (MSP)?
2. What surface antigen can people lack that will protect them against a strain of malaria and which strain will it protect against? |
1. Selects certain features/proteins on the surface of RBCs that Plasmodium Mirazoites will infect.
2. People who lack the Duffy Coat Antigen will be resistant to P. vivax |
|
|
Which RBCs will each strain of Plasmodium preferentially invade?
1. P. vivax 2. P. ovale 3. P. malariae 4. P. falciparum 5. Which strain is most deadly? Why? |
1. P. vivax - Duffy Coat Antigen on Young, immature RBCs
2. P. ovale - Young, immature RBCs 3. P. malariae - Mature RBCs 4. P. falciparum - ALL RBCs 5. P. falciparum - They are very sticky and can stick to endothelium as well. This can narrow capillary spaces causing Cerebral Malaria and Thrombi that can turn into Emboli |
|
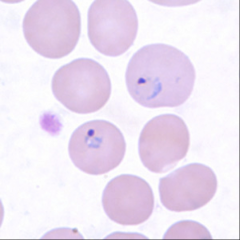
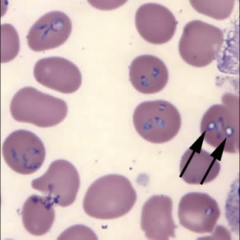
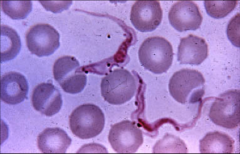
1. What is pictured here and in what stage?
|
1. Plasmodium in Ring Form inside an RBC
|
|
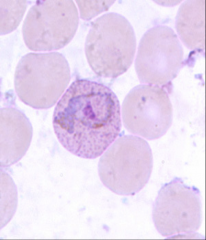
1. What is the amoeboid figure pictured here and in what phase?
2. What becomes of the cytoplasm in this cell? 3. What test would we do to visualize this? |
1. Trophozoite phase of Plasmodium inside an RBC
2. Parasite eats the host cell cytoplasm and breaks down the Hb into AAs 3. Blood smear |
|
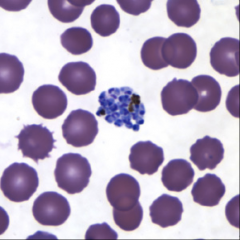
1. What is pictured here and in what stage?
2. How many round of nuclear replication does this undergo? 3. What accounts for the intermittent fever paroxysms associated with malaria? What is a paroxysm? |
1. Plasmodium in an RBC in schizoint form
2. 3-5 rounds 3. Synchronous schizogeny - Simultaneous rupture of RBCs and release of Mirazoites - Paroxysm is a typical pattern of fever, chills, and malarial rigors that reappear periodically |
|
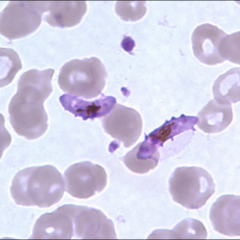
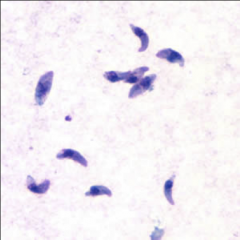
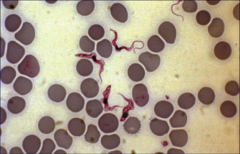
1. What is pictured here and in what stage?
2. Describe the morphology. 3. What will become of this form? |
1. Plasmodium Gametocyte that was released from an RBC
2. Banana-shaped 3. It will be taken up by a mosquito and undergo sexual reproduction there |
|

1. What pigment accumulates in the RBC infected with Plasmodium? What is it comprised of?
2. Why does Plasmodium break down Hb? 3. What part of Malaria causes Anemia? 4. What is are the white arrows in the picture pointing to? |
1. Hemozoin pigment - Hb breakdown products
2. Hb is poisonous to Plasmodium 3. The synchronous rupture of the trophozoites that release Mirazoints. 4. Hemozoin pigment |
|
|
1. How does Cloroquin work?
2. How can Plasmodium cause agglutination of infected RBCs? What is an example of this? |
1. Interferes with Heme polymerization, so the Hb poisons the Schizoint
2. Modification of the RBC membrane - P. Falciparum causes CNS complications |
|
|
1. What is a paroxysm and how often does it last?
2. How long does it last? What is the progression of symptoms? 3. How severe is it? |
1. Typical pattern of chills, fever, and malarial rigors
2. 4-8 hours - Cold Stage (shivers and fever), Hot Stage (HA, Fatigue, dizzy, anorexia, myalgia), Profuse sweating and declining fever, Exhaustion and weakness. No more symptoms until the next Paroxysm 3. Depends on the Plasmodium species |
|
|
1. How can you tell which Plasmodium strain your patient is infected with?
4. What can rupture (aside from RBCs)? |
1. P. vivax and P. ovale - Paroxysms every 2 days
2. P. malariae - Paroxysms every 3 days 3. P. falciparum - Irregular schedule of paroxysms 4. Spleen - you have splenomegaly b/c of the RBC processing |
|
|
1. What is the incubation period for Plasmodium vivax and ovale?
2. What are the initial symptoms? 3. Where is dormancy for P. vivax and P. ovale? |
1. 10-17 days
2. Flu-like illness w/ muscle pains, anorexia, HA, photophobia 3. Hypnozoite form stays in the Liver |
|
|
1. What is the incubation period for Plasmodium malariae?
2. What are the initial symptoms? 3. What is characteristic of the attacks? 4. Is this associated with Hynozoites? |
1. Incubation 18-40 days, possibly months
2. Flu-like symptoms 3. Attacks are moderate to severe and last several hours 4. No association with Hypnozoites. P. malariae is just slow growing |
|
|
1. What is the incubation period for Plasmodium falciparum?
2. What are the symptoms of infection? 3. What are the possible complications of P. falciparum? 4. What will happen if this is left untreated? 5. How does this lead to multiple organ failure? 6. What other malarial form is associated with P. falciparum? |
1. 7-10 days
2. Flu-like initially, but then daily attacks of chills, fever, nausea, vomiting and diarrhea 3a. Cerebral malaria 3b. Blackwater Fever - Kidney damage 3c. Thrombosis 4. Death if untreated 5. Acidosis and hypoglycemia lead to multiple organ failure 6. Malaria of Pregnancy |
|
|
1. How is Plasmodium diagnosed?
2. What are the 3 methods? 3. What is the problem with the Thick Film method? |
1. Demonstration of parasite in RBC
2a. Thick film - RBCs lysed and WBC, platelets and parasites are visible 2b. Thin film - Thin blood layer. Morphologic features are visible for differentiation for definitive species ID 2c. Plasmodium species can be determined by Confirmatory molecular diagnostic tests (PCR) if morphology doesn't cut it 3. Doesn't allow you to differentiate b/w Plasmodium and Bebesia |
|

1. Which strain of Plasmodium and form is pictured here?
2. Why does it appear this way? 3. How can you tell which strain this is? |
1. P. falciparum - ring form
2. Trophozoites and Schizonts are sequestered in the microvasculature 3. Thinner Ring = P. falciparum |
|

1. Which strain of Plasmodium and form is pictured here?
2. How can you tell? |
1. P. vivax and P. ovale - Ring form
2a. The rings are thicker than P. falciparum's ring form, there are more Trophozoites and more Schizonts. 2b. There is also red cell enlargement and Schuffner's dots |
|

1. Which strain of Plasmodium and form is pictured here?
|
1. P. malariae - Band form
|
|
|
What mutations can protect you against Malaria?
|
1. Lack of Duffy Coat Antigen
2. Sickle Cell Anemia 3. G6PD Deficiency |
|
|
What is Chloroquine and what does it do?
Why can't we use this against P. falciparum? What drug should we use against P. falciparum that is immune to Chloroquine? |
1. Treatment of choice for non-falciparum malaria
2. Forms a toxic complex with heme molecules and stops them from crystalizine 3. P. falciparum can reduce the amount of drug that accumulates 4. Mefloquine |
|
|
What is Primaquine and what do we use it for?
How does it work? What do you do if the patient shows symptoms? |
1. Anti-malarial drug used against P. vivax and P. ovale
2. Eradicates Hypnozoites to prevent relapse 3. Symptoms means there is no longer Hypnozoint form, but Mirazoint - Use Chloroquine |
|
|
How to anti-malarial vaccines work?
|
1. Target Sporozoite antigens which are expressed on the surface of infected hepatocytes. Enhances T-cell response
2. Target Merozoite surface molecules |
|
|
1. What is the vector for Babesia microti?
2. What is the significance of this vector? 3. Where do we find Babesia microti, geographically? 4. What is the reservoir? |
1. Ixodes Tick (scapularis)
2. You can have Lyme disease AND Babesia simultaneously 3. Along the eastern seaboard of the US 4. Field mouse and small rodents |
|
|
Describe the lifecycle of Babesia microti.
What makes Babesia's life cycle different from that of Plasmodium? |
1. Infectious pyriform bodies are introduced into the bloodstream and infect RBCs
2. Trophozoites multiply via Binary Fission, formind Tetrads 3. Tetrads lyse the RBC, and are released as Merozoites 4. Merozoites reinfect other cells 5. Ixodes (scapularis) tick takes a bloodmeal and ingests Gametocytes 6. There is NO LIVER PHASE WITH BABESIA and there is NO PERIODICITY TO THE FEVER |
|
|
1. What are the clinical consequences of Babesia?
2. What is the incubation period? 3. What can develop in advanced cases? 4. Who is at risk for developing symptoms from Babesia Microti? |
1a. Asymptomatic in most people
1b. General malaise, FEVER WITHOUT PERIODICITY, HA, chills, sweating fatigue, weakness 2. 1-4 weeks 3. Hepatomegaly and Splenomegaly 4. Immunosuppressed, Elderly, SPLENECTOMY |
|
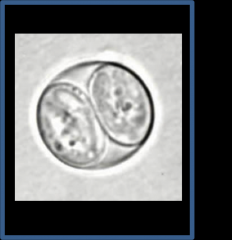
1. What are the black arrows pointing to? Why is this significant?
2. When you Giemsa stain a blood sample infected with this, what will you see? 3. What else will help you diagnose this? 4. How do you treat this? |
1. Maltese Cross characteristic of Babesia Microti
2. Maltese Crosses and Ring Forms 3. Lack of response to anti-malarials 4. Quinine and Clindamycin |
|
|
1. Name a coccidian Blood and Tissue protozoan intracellular parasite
2. What is this organisms definitive host? 3. What is a definitive host? 4. What is an intermediate host? 5. What is this organism's intermediate host? 6. How do we get this parasite? |
1. Toxoplasma gondii
2. Cat and other Feline 3. Definitive host - Essential Reservoir where the parasite passes its adult and sexual existence 4. Intermediate Host - Hosts that the parasite passes its LARVAL or NON-SEXUAL EXISTENCE 5. Toxoplasma gondii - Poultry, rodents, cattle, PORK 6. Eating cysts |
|
|
1. How do people contract Toxoplasma gondi?
2. What percentage of people in the US are seropositive? Europe? |
1a. Ingestion of undercooked PORK contaminated with cysts
1b. Contact with cat feces 2. 20-40%. 90% in Europe because they eat raw meat |
|
|
1. Why are pregnant women supposed to stay away from cat litter?
2. What happens if they don't? |
1. Toxoplasma gondii cysts can be in cat feces and it can cross the placents
2. Hydrocephaly, Retinitis, Developmental problems |
|
|
Describe the lifecycle of Toxoplasma gondii
|
1. Oocysts are ingested (pictured)
2. They mature into Tachyzoites - Responsible for the initial infection and tissue damage - They spread via the blood and lymphatics 3. Tachyzoites from the blood localize in NEURAL AND MUSCLE TISSUE, causing symptoms 4. Develop into Tissue Cyst BRADYZOITES 5. Form dominant tissue cysts in different parts of the body. 6. Chronically and intermittently reactivate, but your body fights off the Tachyzoites that emerge because the body is used to them 7. Host cells are destroyed by multiplication of Toxoplasma gondii |
|
1. What is pictured above?
2. What is its function? 3. What happens in an immunocompromised host? |
1. Tachyzoite of Toxoplasma gondii
2. Responsible for initial infection and tissue damage 3. Infection is activated and disseminated to the CNS |
|
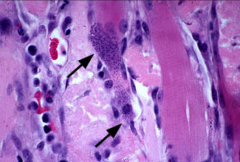
1. What are the black arrows pointing to in the picture?
2. When do tissue symptoms occur? 3. What happens after these symptoms occur? 4. How are Tachyzoites spread throughout the body? |
1. Toxoplasma gondii tissue cysts
2. When the parasite moves from blood to tissues. 3. There is reproduction of more organisms and then cyst formation 4. Tachyzoites are disseminated throughout the body via the Blood and Lymphatics |
|
|
What are the symptoms that are possible for Toxoplasma gondii infection in the following groups:
1. Healthy people 2. Pregnant women 3. Immunocompromised |
1. Asymptomatic with possible Fever, Flu-like illness with lymphadenopathy. Bradyzoite cysts will still be present
2. Fetus may get infected --> Severe congenital infection 3. Primary reactivation can result in CNS disease |
|
|
1. How is Toxoplasma gondii diagnosed?
2. Why is antibody testing difficult to use for an immunocompromised patient? |
1a. Immunocompromised - RING SHAPED LESION ON MRI
1b. Serology for IgM/IgG 1c. CSF, blood, tissue --> Histology and PCR 2. It is likely a re-infection, so there would be no IgM |
|
|
Where are Trypanosomas found and in what form? What are the physical characteristics of each form?
|
1. Human blood - Trypomastigotes with flagellum and undulating membrane
2. Tissues as Amastigotes - oval cells with neither a flagellum NOR an undulating membrane |
|
1. What is pictured here? Describe the morphology.
2. What do they infect and what form do they take? |
1. Trypanosomastrigotes - Ropy with flagellum and an undulating membrane
2. Infect Macrophages and become Amastagotes |
|

1. What is pictured?
2. What is it a vector for? 3. What does this protozoa cause? 4. What is the other name for this disease? |
1. Reduviid aka "Kissing Bug"
2. Trypanosoma cruzi 3. Chagas disease - Most common cause of Myocarditis in the world 4. American Trypanosomiasis |
|
|
1. How does Chagas Disease present?
2. Where is this disease most often found? 5. How does transmission of this disease work? |
1. Acute myocarditis or Chronic cardiomyopathy
2. South and Central America 3. Reduviid kissing bug takes a blood meal and then poops on you and rubs it into the stab wound |
|
|
Describe the lifecycle of Trypanosoma cruzi
|
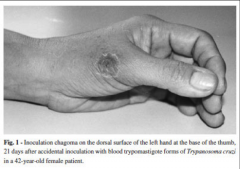
1. Reduviid bites you and poops the virus into the bite site
2. Trypomastigote (infective form) enters the wound 3. Infects and reproduces in cells at the Inoculation site 4. Forms a localized nodular inflammatory lesion (CHAGOMA) (Pictured) 5. Migrates to tissues (cardiac muscle, liver, brain) where it produces the MOST SIGNIFICANT DISEASE 6. Grows via binary fission 7. Amastagotes are intracellular |
|

What is Romana sign?
What is it a sign of? What are other symptoms? Where is it mostly localized? What does the heart look like in fatal cases? |

Swelling around the eye (pictured on front card)
Early Chagas Disease from Trypanosoma Cruzi Myocarditis, Achalasia, Megacolon, Megaureter Localizes in the Heart and Nerve Cells of the Myenteric Plexus Pathology - Heart is enlarged (Pictured) and dilated with PALE, FOCALLY HEMORRHAGIC MYOCARDIUM and Numerous Parasites are found in the heart |
|
|
What are the symptoms of chronic disease with Tryponosoma cruzi (Chagas disease)?
|
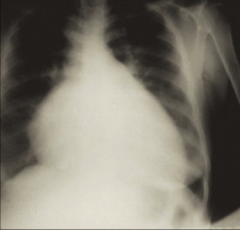
1. Cardiac Failure and GI disease
2. Chronic progressive inflammation 3. Dilated heart, interventricular septum deviated to the right 4. Immobilized tricuspid leaflet 5. Progressive fibrosis causes dysrhythmia or CHF 6. GI - Destruction of Parasympathetic Connections --> No digestion |
|
|
1. How is Triponosoma cruzi diagnosed?
2. How is it treated? 3. Is this treatment curative? |
1a. Blood films - Easiest in the acute stage
1b. Biopsy - organisms in amastigote stage 1c. RT-PCR - looking for amastigote 2. Antiparasitic agents (Nifutimox and Benznidazole) eradicate the parasitemia during the acute phase 3. Curative - YES |
|
1. What is Trypanosoma b. gambiense?
2. What is Trypanosoma b. rhosescience? 3. How is the Trypamastigote infection transmitted in the above infections? 4. What is the pathogenesis? 5. How is it diagnosed? 6. What is the treatment? |

1. West African Sleeping Sickness
2. East African Sleeping Sickness 3. Tsetse Fly (pictured) 4. Surface glycoproteins undergo antigenic variation, so our body will stop recognizing them 5. Blood smears 6a. Acute - Suramin 6b. Chronic - Melarsoprol |
|
|
1. If a patient had something that looked like malaria, but it had Lymphadenopathy as a symptom, what would you suspect?
2. What is this disease, clinically? 3. What are the symptoms? 4. What happens if the patient is not treated? |
1. T. b. gambiense: West African Sleeping Sickness
2. More chronic form of WASS. 3a. PAINFUL CHANCRE DEVELOPS AT THE BITE SITE 3b. Dissemination --> Intermittent spiking fever, headaches, lymphadenopathy (LIKE MALARIA, BUT MALARIA DOES NOT HAVE LYMPHADENOPATHY) 3c. Late stage --> Daytime somnolence, neuropsychiatric features, confusion, disruption of normal circadian rhythm. NOCTURNAL IRRITABILITY 4. Death |
|

1. What is pictured above and what causes it?
2. What is the difference between this and West African Sleeping Sickness? 3. What are the symptoms? 4. What happens if the patient is not treated? |
1. Painful Chancre at the bite site from a TseTse Fly - T. b. Rhodesiense - East African Sleeping Sickness
2. Progresses more rapidly, leading to coma and death within weeks to months 3a. Painful chancre at bite site. 3b. Severe intermittent fever, rash, cardiac manifestations, anemia, DIC 3c. Late Stage - Daytime Somnolence, Nighttime Irritability 4. Death |
|
|
1. How will you be able to tell if you are looking at Leishmania species?
2. What is the vector? |
1. AMASTIGOTES are ALWAYS IN MACROPHAGES
2. Sandfly |
|
|
1. What is caused by Leishmania donovani?
2. What are the symptoms? 3. What causes the Hepatosplenomegaly? 4. What is a major risk factor for Leishmania Donovani? 5. How is Leishmania Donovani diagnosed? |

1. Visceral Leishmania
2a. Asymptomatic 2b. Classic VL (kala-azar): Prolonged fever, weight loss, HEPATOSPLENOMEGALY (pictured), pancytopenia 3. Amastigote-infected macrophages in the liver and spleen causing progressive hypertrophy 4. Malnutrition 5. Amastigotes in Macrophages and PCR |
|

1. Which Leishmania species causes the pictured symptom?
2. What is distinctive about cutaneous Leishmaniasis? 3. What is the cause of the ulcers? 4. How is Cutaneous Leishmaniasis diagnosed? |
1. A variety of species cause Cutaneous Leishmaniasis EXCEPT Leishmania Donovani and Leishmania Braziliensis
2. Localized or diffuse cutaneous lesions and/or ULCERS 3. Bite of a Sandfly 4. Clinical diagnosis and by identifying amastagotes in Macrophages and doing PCR |
|

1. What is pictured above?
2. What causes this? 3. What is this patient at increased risk for? 4. How is this diagnosed? 5. How is it treated? |
1. Ulceration to the point of perforation and tissue destruction due to association of LEISHMANIA BRAZILIENSIS deeper into the mucous membranes
2. Leishmania Braziliensis 3. Secondary bacterial infections 4. Diagnosed - Clinical, Amastigotes in Tissue, PCR 5. Treated - Sulfate Drugs from the CDC |

