![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
145 Cards in this Set
- Front
- Back
|
These 5 types of WBCs can be found circulating in the blood |
Monocytes, Neutrophils, Eosinophils, Basophils, Natural Killer Cells |
|
|
These are larger than average cells, have a prominent bean-shaped nucleus and are motile |
Monocytes |
|
|
These give rise to macrophages and dendritic cells |
Monocytes |
|
|
Are monocytes part of the innate or adaptive immune response? |
Innate |
|
|
What cytokines and other molecules are released by monocytes? |
IL1, IL6, IL10, TNFa, IFN-g |
|
|
These cells are also known as Kuppfer cells in the liver, and microglia in the brain. |
Macrophages |
|
|
This type of cell can be found in various tissues as well as the subepithelial space under tissues. |
Macrophages |
|
|
This type of cell is a large amorphous blob, has lots of vesicles, a prominent nucleus, and its motile |
Macrophages |
|
|
Macrophages are part of the innate or the adaptive immune response? |
Innate |
|
|
List the main surface molecules found on macrophages. (6) |
complement receptors, cytokine receptors, chemokine receptors, MHC I, MHC II, and Toll-like receptors |
|
|
What cytokines and other molecules are released from macrophages? |
IL1, IL6, IL10, TNFa |
|
|
The main functions of this type of cell include phagocytosis, endocytosis, pinocytosis, engulf opsonized cells, and release cytokines. |
Macrophages |
|
|
List the 5 main functions of macrophages. |
phagocytosis endocytosis pinocytosis engulf opsonized cells release cytokines |
|
|
The intake of fluid by the cell. "Cell drinking" |
pinocytosis |
|
|
The rendering of bacteria and other cells vulnerable to phagocytosis, i.e. the attachment of antibodies for identification |
opsonization |
|
|
This type of cell is known as Langerhans cells in epithelial layers. |
Dendritic cells |
|
|
The main locations of this type of cell is in the tissues and then moves to lymph vessels and lymph nodes when activated by a pathogen to activate B and T cells |
Dendritic Cells |
|
|
This type of cell is star shaped with lots of tentacles |
Dendritic cells |
|
|
The main functions of this type of cell are cross-presentation of antigen on MHC, activate T cells to bridge innate and adaptive immunity, phagocytosis, chemokine and cytokine release |
dendritic cells |
|
|
List the 4 functions of dendritic cells |
cross-presentation of antigens on MHC activate T cells to bridge innate and adaptive immunity phagocytosis chemokine and cytokine release |
|
|
Dendritic cells are part of the innate or the adaptive immune response? |
Innate (but a bridge between the two) |
|
|
List the main surface molecules of dendritic cells. (7) |
MHC I, MHC II, Toll-like receptors, complement receptors, chemokine receptors, cytokine receptors, CD86 |
|
|
List the cytokines and other molecules released by dendritic cells. (7) |
IL1, IL6, IL10, IL12, INFa, TGFB, TNFa |
|
|
These are usually found in the blood until summoned during an innate immune response |
Neutrophils |
|
|
This type of cell has a segmented nucleus and lots of granules. |
Neutrophils |
|
|
List the main functions of neutrophils. (4) |
The main phagocytic cells kill engulfed pathogens with proteolytic enzymes dead cells form pus chemokine and cytokine release |
|
|
Neutrophils are part of the innate or adaptive immune response? |
Innate |
|
|
List the main surface molecules of neutrophils. (8) |
CXCR8, selectin, integrin, cytokine and chemokine receptors, MHC I, MHC II, complement receptors, toll-like receptors |
|
|
These are proteins expressed by leukocytes, synthesized by helper CD4 T Lymphocytes, monocytes and macrophages. They help promote the development and differentiation of T and B lymphocytes and hematopoietic cells. |
interleukins |
|
|
List the cytokines and other molecules released by neutrophils. (2) |
Proteolytic proteins to kill pathogens pro-inflammatory cytokines |
|
|
This type of cell stains pink and has many granules. |
Eosinophils |
|
|
The main function of this type of cell is its involvement in the inflammatory response to allergies and parasite responses after binding IgE. |
Eosinophils |
|
|
Are eosinophils part of the innate or adaptive immune response? |
Innate |
|
|
List the main surface molecules located on eosinophils. (5) |
Fc receptors cytokine and chemokine receptors MHC I MHC II |
|
|
List the cytokines and other molecules released by eosinophils. (6) |
IL1 IL6 IL4 IL10 TNFa TGFB |
|
|
This cell stains blue, has lots of granules. |
Basophils |
|
|
The main functions of basophils are? |
involved in the inflammatory response to allergies and parasite responses after binding IgE |
|
|
Basophils are part of the innate or adaptive immune response? |
Innate |
|
|
List the main surface molecules present on basophils. (5) |
Fc receptors, cytokine and chemokine receptors, MHC I MHC II |
|
|
List the cytokines and other molecules released by basophils. (6) |
IL1, IL6, IL4, IL10, TNFa, TGFB |
|
|
This type of cell is found in the tissues and sub epithelial spaces of tissues. #2 |
Mast Cells |
|
|
This type of cell is round and full of granules. |
Mast cells |
|
|
What is the main function of a mast cell? |
It is the main cell to cause inflammatory response after binding to anaphylotoxins and degranulating, involved in allergic response in tissue after binding IgE |
|
|
List the 5 parts of the inflammatory response. |
heat, pain, swelling, redness, vasodilation |
|
|
Are mast cells part of the innate or adaptive immune response? |
Innate |
|
|
List the main surface molecules found on mast cells. (5) |
Fc receptors Complement receptors cytokine and chemokine receptors MHC I |
|
|
List the cytokines and other molecules released from mast cells. (5) |
histamine TNFa proteolytic proteins pro-inflammatory cytokines chemokines |
|
|
This type of cell is found in the blood circulation until it is summoned during the innate immune response. |
Natural Killer Cells |
|
|
This type of cell has a large, round nucleus, and its granular |
Natural Killer Cells |
|
|
The main function of this type of cell is to make interferons and to non-specifically kill virus-infected cells with proteolytic enzymes. |
Natural Killer Cells |
|
|
Are natural killer cells part of the innate or the adaptive immune response? |
Innate |
|
|
List the main surface molecules found on natural killer cells. (7) |
CXCR10 activating receptor inhibitory receptor MHC I toll-like receptors cytokine receptors chemokine receptors |
|
|
List the cytokines and other molecules released by natural killer cells. (3) |
interferons pro-inflammatory cytokines chemokines |
|
|
This type of cell is found in the lymph nodes and lymph vessels. they develop in the thymus, migrate to the blood circulation and tissues when their specific antigen is infecting the organism |
CD4/Helper T cells |
|
|
This type of cell is large, motile, with a few ragged edges and prominent nucleus. |
CD4/Helper T cells |
|
|
List the main functions of CD4/helper T cells. (4) |
helps CD8 T cells grow helps B cells isotype switch and somatic hypermutate remembers specific pathogens to make a stronger and faster secondary immune response variety of functions concerning specific pathogens |
|
|
Are CD4/helper T cells part of the innate or adaptive immune response? |
Adaptive |
|
|
List the main molecules found on the surface of CD4/T helper cells. (7) |
CD4 T cell receptor Cytokine receptors Chemokine receptors CD40 ligand CD28 (receptor for CD86) CD3 |
|
|
This type of cell releases a variety of pro and anti-inflammatory cytokines depending on the T cell type and chemokines |
CD4/Helper T cells |
|
|
This type of cell is found in lymph nodes, and lymph vessels. they develop in the thymus. migrate to blood circulation and tissues when their specific antigen is infecting the organism. |
CD8/cytotoxic/killer T cells |
|
|
This type of cell has a large, round, prominent nucleus and its motile. |
CD8/cytotoxic/killer T cells |
|
|
List the main functions of CD8/cytotoxic/killer T cells. (2) |
kills cells infected with a specific virus using proteolytic enzymes. remembers specific pathogens to cause a stronger and more rapid secondary response |
|
|
CD8/cytotoxic/killer T cells are part of the innate or adaptive immune response? |
Adaptive |
|
|
List the main molecules located on the surface of CD8/cytotoxic/killer T cells. (7) |
CD8 T cell receptor cytokine receptors chemokine receptors CD40 ligand CD28 CD3 |
|
|
List the molecules released by CD8/cytotoxic/killer T cells. (2) |
pro-inflammatory cytokines chemokines |
|
|
This type of cell develops in the bone marrow mostly and then is found in the lymph nodes and lymph vessels when maturing. Migrates the to blood when activated by an antigen |
B cells |
|
|
This type of cell has a round, prominent nucleus and is motile. |
B cells |
|
|
List the main functions of B cells. (2) |
Produce antibodies against specific pathogens which bind to their pathogen and cause them to be engulfed or neutralized remember specific pathogens to make a more rapid and stronger secondary response. |
|
|
List the types of antibodies produced by B cells. |
IgM IgD IgA IgG IgE |
|
|
Are B cells part of the innate or adaptive immune response? |
Adaptive |
|
|
List the molecules found on the surface of B cells. (4) |
B cell receptor (surface-bound immunoglobulin) CD28, CD40, MHC II |
|
|
List the cytokines and molecules released by B cells. (3) |
Antibodies (IgM,D,G,A,E) cytokines chemokines |
|
|
________ binds viral capsids, and ______ activates ________ to cut up viral dsRNA |
1) Mx 2) OAS 3) RNaseH |
|
|
______, ______, and ______ act locally on endothelial cells and incoming leukocytes AND globally |
IL-1beta, IL-6, TNFalpha |
|
|
IL-12 and the interferons act locally to activate ________, _________, and other cells to fight viruses. |
CD8+ T cells, NK cells |
|
|
___________________ can be made by all cells to alert other nearby cells to a virus too, increasing _________ expression and activating the immunoproteasome so more proteins will be cut in the Endogenous Pathway so viruses can be detected. |
Type I interferons (alpha & beta) MHC I |
|
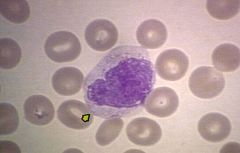
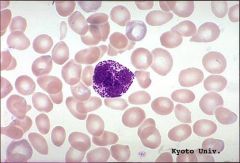
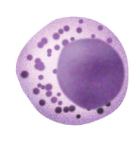
What's this? |
Monocyte |
|
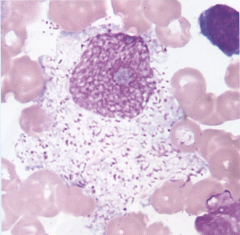
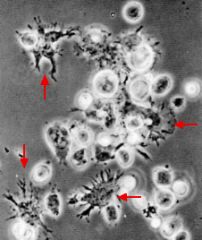
What's this? |
Macrophage |
|
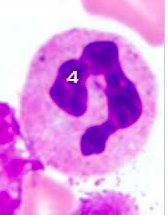
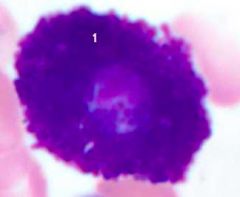
What is this? |
Neutrophil |
|
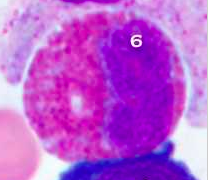
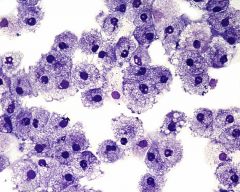
What's this? |
Eosinophil |
|
What's this? |
Basophil |
|
What's this? |
Dendritic Cells |
|
What's this? |
Mast Cell |
|
What's this? |
Helper T cell |
|
What's this? |
Natural Killer Cell |
|
|
Which three types of leukocytes have granules? |
Neutrophils, Eosinophils, Basophils |
|
|
Which two types of leukocytes do not have granules? |
Lymphocytes and monocytes |
|
|
What combination of dyes is generally used to stain leukocytes? |
Eosin and Methylene blue |
|
|
Which are the most common type of leukocyte and what percentage of the blood do they make up? |
Neutrophils, 60-70% |
|
|
What is the second most common type of leukocyte and what percentage does it make up? |
Lymphocytes (T and B cells), 20-50% |
|
|
What is the third most common type of leukocyte and what percentage does it make up? |
Monocytes, 2-10% |
|
|
What is the fourth most common type of leukocyte and what percentage does it make up? |
Eosinophils, 1-6% |
|
|
What is the fifth and most rare type of leukocyte and what percentage does it make up? |
Basophils, 1% |
|
|
List the 2 steps in humoral mediated immunity. |
1) A B cell binds to its specific antigen. Some B cells need T helper cells. B cell proliferates and become plasma cells or memory cells. 2) The plasma cells proliferate and produce antibodies against the antigen. |
|
|
List the 3 steps of cell-mediated immunity that takes place after exposure to the antigen and the display of foreign proteins on the cell surface. |
1) A T cell binds to MHC-antigen complexes on the surface of the cell, activating the T cell with it's cytokine receptors. 2a) Cytokines activate macrophages. 2b) CD8 T cell becomes cytotoxic T lymphocyte able to induce apoptosis in target cell. 2c) T cells activate TH cells that activate B cells. 3) Some T cells become memory cells. |
|
|
What is humoral immunity designed to control? |
Freely circulating pathogens |
|
|
What is cell-mediated immunity designed to control? |
intracellular pathogens |
|
|
What and where is the thymus and what happens in it? |
Near the heart. Immune system organ where T cells and T lymphocytes mature from hematopoietic cells. |
|
|
Answer for the primary immune response: antigen type, responding cells,
|
Both T dependent and T independent B cells Naive B or T cells |
|
|
Answer for the secondary immune response: antigen type, responding cells, |
Only T dependent cells Memory B or T cells |
|
|
Answer for primary immune response: lag period, peak response, magnitude, |
Longer: 4-7 days Occurs in 7-10 days Low |
|
|
Answer for primary immune response: antibody isotype, antibody affinity |
IgM predominates Lower |
|
|
Answer for secondary immune response: Lag period peak response magnitude |
Shorter: 1-3 days Occurs in 3-5 days High: 100-1000x |
|
|
Answer for secondary immune response: Antibody isotype antibody affinity |
IgG predominates Higher |
|
|
This antibody is the main antibody in blood. It is transferred from mother to baby. It is widely distributed throughout the blood and tissues. |

IgG |
|
|
This antibody is made up of five antibodies. It has a key role in the initial immune system. It circulates in the blood. |

IgM |
|
|
This antibody is made up of 2 antibodies. It is distributed to serum, nasal discharge, saliva, breast milk and bowel fluid. Breast milk protects the gastrointestinal tract of newborns from bacterial and viral infection (maternal immunity). |

IgA |
|
|
This antibody is present on the surface of B cells and plays a role in the induction of antibody production. |

IgD |
|
|
This antibody is believed to be related to immunity reactions to parasites, and has recently become known as a key factor of allergies. |

IgE |
|
|
List in order of reaction the major components of complement activation in the Classical Pathway. |
C1 activated when it binds to antigen/antibody complex. C1 cleaves C2 into C2a and C2b; and C4 into C4a and C4b. C2b and C4b combine to form C3 convertase which cleaves C3 into C3a and C3b. Classical and alternative now merge. |
|
|
List in order of reaction the major components of complement activation in the alternative pathway. |
C3b interacts with endotoxins, cell walls, and polysaccharides. C3b the reacts with Factor B, D, and Properdin to make C3 convertase which cleaves C3 Classical and alternative now merge. |
|
|
What are the 3 anaphylotoxins in the complement cascade and what do they do? |
C3a, C4a, C5a They cause smooth muscle contraction, histamine release from mast cells, and enhanced vascular permeability. They also mediate chemotaxis, inflammation. |
|
|
What is required to activate the lectin pathway? |
carbohydrates (D-mannose and L-fucose residues) found on the surfaces of many pathogens. |
|
|
In classical complement cascade, C1 has three parts: C1q, C1r, C1s. What is their functions? |
C1q: binds directly to pathogens surface or indirectly to antibody-bound pathogens, activating Cr C1r: Cleaves C1s to activate protease C1s: Cleaves C2 and C4. |
|
|
In classical complement cascade, C4 is split into C4a and C4b. What is their function? |
C4a: peptide mediator of inflammation C4b: covalently binds to pathogen and opsonizes it. Binds C2 for cleavage by C1. |
|
|
In classical complement cascade, C2 is split into C2a and C2b. What is their function? |
C2a: precursor of vasoactive C2 kinin C2b: active enzyme of classical pathway of C3/C5 convertase: cleaves C3 and C5 |
|
|
In classical complement cascade, C3 is split into C3a and C3b. What is their function? |
C3a: peptide intermediator of inflammation C3b: Binds to pathogen surface and acts as opsonins, initiates amplification via the alternative pathway, binds C5 for cleavage by C2b. |
|
|
In the alternative complement cascade, what is the function of C3b? |
binds to pathogen surface, binds B for cleavage by D, C3bBb is C3 convertase; C3b2Bb is C5 convertase |
|
|
In the alternative complement cascade, Factor B is split into Ba and Bb. What is the function of Bb? |
Active enzyme of the C3 and C5 convertases. |
|
|
In the alternative complement cascade, what is the role of Factor D? |
plasma serine protease, cleaves B when it is bound to C3b to Ba and Bb |
|
|
In the alternative complement cascade, what is the role of Properdin? |
plasma protein that binds to bacterial surfaces and stabilizes the C3bBb convertase |
|
|
In complement regulation, what binds to C3b to inactivate it? |
CR1, H, DAF, and MCP |
|
|
In the complement cascade, C5 is cleaved by what to produce C5a and C5b? |
C2a or Bb |
|
|
What needs to bind to a bacteria and macrophage in order for phagocytosis to occur? |
C3b binds to bacteria binds to CR1while C5a |
|
|
What is a respiratory burst? |
the rapid release of reactive oxygen species (superoxide radical and hydrogen peroxide) from different types of cells. |
|
|
Name the three common types of phagocytic receptors. |
Toll-like receptors, scavenger receptors, opsonin receptors |
|
|
what is the function of toll-like receptors? |
bind to more specific molecules, increases phagocytosis and causes the phagocyte to release a group of hormones that cause inflammation. |
|
|
What is the function of Opsonin receptors? |
increase the phagocytosis of bacteria that have been coated with immunoglobulin G (IgG) antibodies or with complementw |
|
|
What is the function of scavenger receptors? |
bind to a large range of molecules on the surface of bacterial cells |
|
|
In the terminal complement cascade, what is the role of C5b? |
initiates assembly of the membrane attack system |
|
|
In the terminal complement cascade, what is the role of C6, C7, C8 and C9? |
C6: binds C5b, forms acceptor for C7 C7: Binds C5b6, amphiphilic complex inserts into lipid bilayer C8: Binds C5b67, initiates C9 polymerization C9: polymerizes to C5b678 to form a membrane-spanning channel, lysing cell |
|
|
What are the 4 main steps in extravasation? |
Chemoattraction rolling adhesion tight adhesion transmigration |
|
|
What happens during the chemoattraction step of extravasation? |
Endothelial cells of the blood vessels express cellular adhesion molecules and selectin, leukocytes are attracted to the area by chemokines. |
|
|
What happens during the rolling adhesion step of extravasation? |
bonds between the leukocyte and the selectins cause the leukocyte to slow down and roll along the vessel wall. |
|
|
What happens during the tight adhesion step of extravasation? |
chemokines cause the cells to switch from selectins to integrins which have a higher affinity. This causes the leukocyte to stay in place. |
|
|
What happens during the transmigration step of extravasation? |
leukocytes flatten out and pass between the endothelial cells |
|
|
What is the definition of autocrine, paracrine, and endocrine in terms of cytokines? |
autocrine: cell signaling itself paracrine: cell signaling other cells endocrine: signals entire body |
|
|
What does TLR4 specifically interact with? |
LPS, MD2, LPB |
|
|
____________, also known as antigenic determinant, is the part of _______ that is recognized by the immune system, specifically by antibodies, B cells, or T cells. |
epitope antigen |
|
|
Whats the difference between polyclonal and monoclonal antibodies? |
Monoclonal antibodies are clones of one B cell, polyclonal antibodies are different antibodies that all react to one antigen, just different pieces of it. |
|
|
What do CD4 cells do and what do CD8 cells do? |
CD4: t helper cell CD8: cytotoxic t cell |
|
|
As the most variable parts of the molecules, _____________________________ are crucial to the diversity of antigen specificities generated by lymphocytes |
complementarity determining regions |
|
|
The light chains and the heavy chains of immunoglobulins are held together by what? |
disulfide bonds |
|
|
Review the differences between TCR and BCR |

|
|
|
What is the difference between MHC 1 and MHC 2? |

|

