![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
cell-mediated immunity |
-acquired/adaptive/specific immunity -third line of defense -INTRACELLULAR pathogens -"housekeeping" -T cells and NK cells -kill: altered cells, infected cells (w viruses, fungi, bacteria, etc), cancer cells |
|
|
humoral immunity |
-acquired/adaptive/specific immunity -third line of defense -EXTRACELLULAR pathogens -B cells --> antibodies and memory cells |
|
|
lymphatic system |
-lymphatic organs and lymphatic vessel that run parallel to the circulatory system -liquid portion of blood that seeps out of the capillaries -exact composition of blood except RBCs (too large to leak out) |
|
|
primary lymphatic tissues and organs |
1. bone marrow 2. thymus -production, maturation, differentiation of lymphocytes |
|
|
secondary lymphatic tissues and organs |
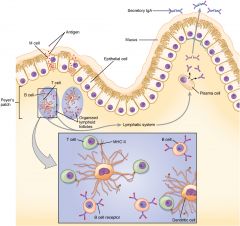
1. lymph nodes: "one way streets" that filter lymph for antigens; B and T cells interact 2. spleen: filters blood for antigens; white pulp = lymphocytes that filter blood for infection, red pulp = processing dead red blood cells (does NOT filter blood for infection) 3. tonsils: fight inhaled foreign pathogens 4. lymphoid tissues: network of loosely attached and connected lymphatic vessels; GALT, BALT, MALT, SALT 5. Peyer's patches: organized aggregations of lymphoid tissue found in intestine/lungs covered with epithelium that contains microfold M cells that get infected by antigen and then pass along to underlying immune cells; on-the-spot 6. appendix -adaptive immune response by encounter and binding antigens |
|
|
immune cells origins/lineages |
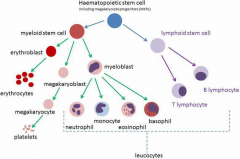
-originate in the bone marrow -BM contains hematopoietic stem cells -hematopoietic stem cells differentiate into lymphoid stem cells (B cells and T cells) + myeloid stem cells (RBCs, platelets, neutrophils, basophils, eosinophils, mast cells, monocytes, macrophages, dendritic cells) -leukocytes play a role in both innate and acquired immunity |
|
|
lymphocytes |
-lymphoid line from hematopoietic -not phagocytic -lymphocytes: B cells + T cells + NK cells 1. B cells: produced in BM; mature in BM; activated in lymph nodes; differentiate into plasma cells (produce Igs) + memory cells; antigen-presenting cells (APCs) 2. T cells: produced in bone marrow; mature in thymus; differentiate into help T cells, cytotoxic T cells, memory T cells 3. NK cells: kill malignant and infected cells; are part of acquired/specific and innate/nonspecific immunity --> B and T cells are morphologically similar (both agranular) but have different surface receptors |
|
|
monocytes/macrophages |
-myeloid line from hematopoietic -phagocytic -agranular 1. monocytes: circulate around whole body for 8 hours before mature into macrophages 2. macrophages: localized to specific tissues, antigen-presenting cells (APCs) to helper T cells, produce cytokines, and have numerous different surface receptors -receptors for toll-like structures (pili, fimbriae, LPS, etc) -receptors for Fc region of antibodies: can bind to antibodies that are bound to pathogens/infected cells and can then phagocytose |
|
|
dendritic cells |
-myeloid line from hematopoietic -phagocytic: not main job -professional antigen-presenting cells (APCs): main job -under skin, in mucous membranes, in lungs/intestines |
|
|
antigen-presenting cells (APCs) |
-B cells -macrophages -dendritic cells |
|
|
phagocytic cells |
-macrophages -dendritic cells -neutrophils |
|
|
neutrophils |
-myeloid line from hematopoietic -phagocytic -defend against extracellular infections (especially bacterial and fungal) |
|
|
neutropenia |
-abnormally low neutrophil count -highly vulnerable to bacterial infection (neutrophils phagocytose extracellular bacteria) |
|
|
eosinophils |
-myeloid line from hematopoietic -inflammatory cells in allergic reactions -deal with parasitic infections (e.g. by microscopic worms) |
|
|
mast cells |
-myeloid line from hematopoietic -contain granules rich in histamine -cause allergies |
|
|
basophils |
-myeloid line from hematopoietic -play role in allergic response and hypersensitivity -release histamine, prostaglandins, serotonin, and leukotriences |
|
|
agranular cells |
-lymphocytes (B/T/NK) -monocytes/macrophages |
|
|
granular cells |
-neutrophils -eosinophils -mast cells -basophils |
|
|
polymorphonuclear neutrophils |
-doctors can diagnose a bacterial infection by looking at heightened levels of PMNs (polys) -? specifically neutrophils because those are the ones that are good with extracellular bacteria ? |
|
|
first line of defense |
-barrier defense -nonspecific 1. skin 2. mucous membranes |
|
|
second line of defense |
-nonspecific -if pathogen enters the body and barrier method fails 1. phagocytosis 2. inflammation 3. extracellular killing 4. fever 5. complement system |
|
|
skin |
-dry, cool, salty (perspiration), and low pH (oil from sebaceous glands) -perspiration contains lysozyme and other antimicrobials -normal skin flora compete with pathogens for space/food and synthesize vitamins that help with host growth/metabolism -epidermis is constantly regenerated -mucociliary blanket/mucociliary escalator: prevents microbes from entering the lungs; once microbes and been brought up respiratory tract, can be sneezed/coughed/swallowed |
|
|
mucous membranes |
-mucous membranes of respiratory/digestive/urogenital tracts are most frequently used portals of entry for pathogens -mucous = sealant that covers and protects cells of the membrane -mucous membranes sometimes contain specialized cells that kill foreign invaders before enter body -epithelium = outermost layer of mucous membrane; constantly regenerated and microbes get shed away with epithelium |
|
|
difference between epithelium and epidermis |
-epidermis = dead cells -epithelium = living cells |
|
|
phagocytosis |
-phagocytic cells binds to microbe, engulfs and forms phagosome inside cell body, fuses with lysosome to make phagolysosome, microbial debris is exocytosed -lysosomes contain: lipases, proteases, lysozyme (breaks down bacterial cell walls), nucleases, and toxic reactive oxygen/nitrogen intermediaries (e.g. H2O2) -respiratory burst reactions: when oxygen consumption is increased to produce more toxic oxygen metabolites; occurs with phagosome is formed |
|
|
phagocytic failure |
1. failure of phagosome to fuse with lysosome 2. failure of chemicals in lysosome to kill all of the bacteria caused by: -capsules (make it difficult for phagocytes to grab bacterial cells) -carotenoids (antioxidants that neutralize oxidizing agents in lysozyme like peroxide/superoxide) -catalase (converts H2O2 to H2O + O2) -leukocidins (kill phagocytic WBCs) |
|
|
inflammation |
-when cells of inflammation produce cardinal signs of infection: redness, warmth, swelling, pain, altered function -increases blood flow to affected tissue to expedite repair 1. acute inflammatory response: quickly after injury; chemical mediators promote vasodilation, diapedesis (passage of blood cells through capillary walls bc porous), restriction of pathogen movement, recruiting phagocytes, increasing the temperature (positive feedback, further stimulates the inflammatory response) 2. chronic inflammatory response: slower, longer lasting, maladaptive, permanent tissue damage |
|
|
diapedesis |
-passage of blood cells (especially WBCs) through intact capillary walls into surrounding body tissue |
|
|
extracellular killing************* |
-natural killer cells kill abnormal cells using perforin and phagocytes remove from the body |
|
|
fever |
-body's core temp = 37C or 98.6F -increase metabolic activity, muscle contractions, reduce blood flow to skin -low-grade fever is beneficial to fighting infections -pyrogens = fever-inducing compounds that trigger the hypothalamus to increase core body temp 1. interleukin-1: body's natural pyrogen; produced by the body in response to an infection; acts on hypothalamus which induces fever 2. bacterial components: bacterial toxins and components of bacteria's cytoplasm can act as pyrogens 3. antibody-antigen complexes/immune complexes: result in inflammation and fever |
|
|
the complement system |
-part of both second and third lines of defense: innate and acquired -complement proteins circulate in blood; normally inactivated but become active via complement fixation Active complement proteins do the following: 2. opsonization: CPs cover surface of a microbe and facilitate phagocytosis 3. inflammation: CPs trigger production of inflammatory compounds 4. chemotaxis: CPs act as chemicals to attract immune cells like phagocytes |
|
|
complement fixation |
1. classical pathway (antigen-antibody interactions) 2. alternative pathway (doesn't rely on antibodies) 3. lectin complement pathway (activated by binding of mannose-binding lectin to mannose on pathogen surface) |
|
|
things that play a role in second and third lines of defense***************** |
-complement system -NK cells -phagocytic cells |
|
|
if you put RBCs, antibodies against the RBCs, and complement proteins in a test tube, what would you observe? |
-lysis of the RBCs -classical pathway: antigen-antibody complexes activate CPs, which can form MACs and lyse |
|
|
antigens |
-large and complex -any part of the bacterium: cell wall, capsule, flagella, pili, LPS, surface sugars/lipids/carbs/proteins -fungi, protozoans, viruses, food particles, dust, etc |
|
|
haptens |
-small organic molecule that only elicits immune response if attached to a large carrier protein (too small to be recognized otherwise) -many drugs (e.g. penicillin reacts with blood proteins) |
|
|
epitopes |
-aka antigenic determinants -what B cells, T cells, and antibodies recognize and bind to -proteins = most antigenic of the major polymers (why most vaccines are proteinaceous) -a single bacterium can have several types of epitopes, but antibodies can only recognize one type of epitope |
|
|
opsonization |
-marks microbe for phagocytosis by coating 1. antibodies 2. complement proteins 3. C-reactive protein (CRP) and mannan-binding lectin (MBL): acute phase proteins, act as opsonins, whose plasma [ ]s change due to infection --> bacterial infection activates macrophages and cytokines are released to act on liver to make more MBL/CRP |
|
|
cytokines |
-soluble proteins or glycoproteins -autocrine, paracrine, or endocrine -monokines: released from mononuclear phagocytes (monocytes/macrophages) -lymphokines: released from T lymphocytes -colony stimulating factors (CSFs): stimulate differentiation of immature WBCs in the bone marrow --> lets body respond to infection quickly -interferons: interfere with viral replication/assembly once enter cell |
|
|
third line of defense characteristics******* |
1. tolerance and recognition of self vs non-self: negative selection (B/T cells that would react against body's tissues are apoptosed leading to aenergy) 2. specificity: B and T cells have receptors that recognize specific antigenic determinants 3. heterogeneity: produces a unique response to a variety of different antigens 4. memory: memory cells after primary infection |
|
|
clonal expansion |
-when specific B cells that fight against the present infection are replicated |
|
|
plasma cells vs memory cells |
-plasma cells: short lived and produce antibodies -memory cells: long lived and do not produce antibodies |
|
|
antibodies |
-Y shaped molecules made of 4 polypeptide chains (two heavy and two light) held together by strong disulfide bonds -Fab (nonspecific defense like opsonization) and Fc fragments (what immune molecules bind to) -more diversity in Fab that Fc -bivalent bc two forks (but each fork recognizes identical antigen) |
|
|
classes of antibodies |
1. IgA: secretions (saliva, vaginal fluids, tears, milk) 2. IgE: allergies 3. IgM: primary infection 4. IgG: major circulating antibody, can cross placenta and enter fetus 5. IgD: co-expressed with IgM, activates B cells and basophils |
|
|
why we can have so many different antibodies |
-proteins are assembled in pieces so can mix and match -DNA rearrangement/recombination |
|
|
clonal selection theory |
-how body can generate a large # of immune cells that specifically recognize and attack a pathogen -unique cell receptors of B cells are formed early in lymphocytic development, and genes are shuffled around with lots of combinations -then when cells encounter pathogens they engage in clonal expansion |
|
|
cell-mediated immunity |
-intracellular |
|
|
helpter t cells |
-aka CD4 cells -identify infected cells and release cytokines to amplify immune response -have CD4 receptors that recognize info from antigen-presenting cells -HIV virus neutralizes CD4 receptors |
|
|
cytotoxic T cells |
-aka CD8 cells (CD8 receptors recognize MHC-1 proteins on human cells) -produces perforin: protein that inserts itself into target cell's PM and forms a pore that kills the cell -kills cancer cells, abnormal cells, tumor cells, and infected cells |
|
|
MHC molecules |
-coded for by group of genes: HLA: human leukocyte antigen complex -all human cells except RBCs have MHC-1 -when a human cell is infected it produces abnormal MHC-1 molecules and CD8 cells destruct -two classes: MHC-I and MHC-II |
|
|
natural killer cells |
-kill abnormal cells using perforin but do not have CD8/MHC-1 interaction |
|
|
MHC-1 |
-on surface of almost all kinds of nucleated cells -bind to peptides that come from cytoplasm (unlike MHC-II which come from outside the cell) -normally present "self" antigen -when cell is infected by a virus/intracellular pathogen, MHC-1 molecule presents a foreign antigen, and T cells can come kill |
|
|
MHC-II |
-only on APCs: macrophages, dendritic cells, B cells -bind to fragments that come from outside the cell (unlike MHC-I which come from inside the cell) -can bind to a portion of a foreign bacteria digested by a macrophage, then helper T cells will recognize and initiate immune response via clonal selection |
|
|
T-dependent vs T-independent antigens |
-T-dependent antigens: small with inaccessible antigenic determinants (epitopes); antigen-presenting cells process the antigen and present it to helper T cells which make more accessible --> clonal selection of B cells -T-independent antigens: large and have readily accessible epitopes; can bind to B cells without helper T cells |

