![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
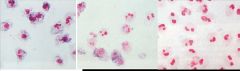
Nitroblue Tetrazolium Test
|
Chronic Granulomatous Disease
(L) Normal PMNs NBT converted to formazon (blue/black precipitate) (C) X-linked CGD carrier PMNs (R) CGD patient PMNs |
|

Poorly demarcated skin, no pus
|
Leukocyte Adhesion Deficiency, Type I
leukocytosis + History of delayed separation of the umbilical cord (>3 weeks post partum) Deficiency in the beta2 integrin (CD18) which is a subunit of adhesion molecules LFA-1 Diagnosis: Flow cytometry for CD18 family integrins Leukocyte Adhesion Deficiency, Type II Longer lifespan than LAD-I Leukocytosis. Do not have delayed umbilical cord separation. Absent sialylated Lewis X (SLeX, CD15s) required for initial binding of PMNs to vascular endothelium via selectins. Patients have "Bombay phenotype" due to lack of expression of blood group H antigen (precursor of blood groups A,B,O). RBCs “non-typeable”. |
|
|
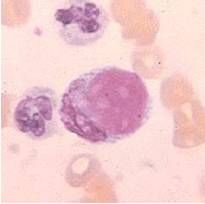
LE cell is a PMN that has ingested the nuclear
debris of a dead cell. The debris is ingested due to anti-DNA antibodies (anti-DNP, antigen is DNAhistone complex) coating the material. |
|
|
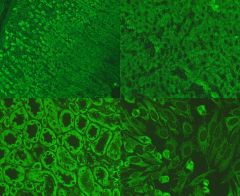
ANA Patterns Speckled
Mitoses: negative Antigens: SSA (Ro) (Sjogren’s,) SSB (La) (Sjogren’s,) Smith (SLE) U1-RNP (MCTD) Scl-70 (fine speckling) (scleroderma) PCNA (ki-67) (SLE) |
|

|
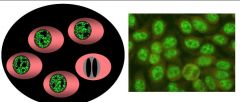
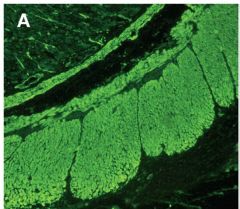
ANA Patterns Homogeneous
Mitoses: Positive Antigens: DNA (SLE) Histone (Medication-induced SLE) dsDNA (SLE) ssDNA |
|

|
ANA Patterns Nucleolar
Mitoses: Negative Antigens: RNA polymerase U3-RNP (fibrillarin) (Polymyositis/Scleroderma overlap) PM-Scl (Scleroderma) |
|
|
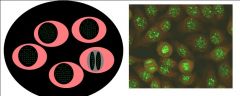
ANA Patterns Centromere
Mitoses: Positive Antigen: CENP- A, B, and C Associations: Scleroderma (CREST syndrome) Raynaud’s |
|
|
ANA Patterns Peripheral (Rim)
Mitoses: Negative Antigen: dsDNA = SLE |
|
|
Anti-Smooth muscle (SMA)
Autoimmune hepatitis. Followup with SMA specific test (e.g. IIF with rat stomach for detection of smooth muscle antibodies) |
|
|
Anti-mitochondrial antibody (AMA)
Primary Biliary Cirrhosis 90% Female, usually age 30-35 Associated with CREST and PSS Anti-mitochondrial antibodies – Also in app 10-15% of CAH IgM polyclonally increased in 80-90% Plasma cells in portal region of liver Cause unknown, but not associated with Hepatitis Viruses |
|

|
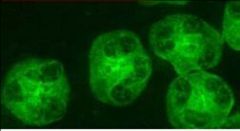
Anti-dsDNA quantification with Crithidia luciliae
• Antibodies directed against native DNA • Assays – ELISA or indirect immunofluorescence on Crithidia – Older assay (Farr assay) quantitates binding of radiolabelled native DNA to sera • Antibodies target deoxyribose backbone or are specific to helical conformation • Present in 40% of SLE patients, rarely found in other diseases – In active, untreated SLE, found in 75-90% – dsDNA antibodies one of 11 criteria for SLE • May be pathogenic: anti-dsDNA containing immune complexes are found in lesions in SLE nephritis, vasculitis, and serositis • In SLE, the anti-dsDNA titer – Correlates with degree of lupus nephritis, may predict flares – Can be used to monitor disease activity (ANA titer not helpful) |
|
|
Neonatal Lupus
|
• Passively transferred autoimmune disease
• Mothers with anti-Ro (SSA) and/or anti-La (SSB) • Clinical: Complete heart block (third degree AV block) and mild rash – Heart block due to AV node damage, may persist – Rash resolves as maternal antibody wanes • Nearly 100% of neonates with complete heart block have anti-Ro (70-90% also have anti-La) • Risk of syndrome in pregnant women with anti-Ro and/or anti-La is 1-2%. Can be diagnosed and treated in utero. |
|
|
cANCA
Antigen: Proteinase (PR3) •Wegener’s (90% in generalized, active disease) • Churg-Strauss (10%) • Microscopic Polyangiitis (30%) • If cytoplasmic staining on ethanol fixed PMNs: cANCA (Proteinase 3, PR3). Confirm with PR3 ELISA. |
|
|
pANCA
Antigen: Myeloperoxidase (MPO) • Microscopic Polyangiitis (50%) •Wegener’s (5%) • Drug induced ANCA + vasculitis –Propylthiouracil, hydralazine, minocycline • Churg-Strauss (60%) • If perinuclear staining on ethanol fixed PMNs pANCA or atypical pANCA FORMALIN FIXED PMNs – If cytoplasmic staining on formalin fixed PMNs pANCA. Confirm with MPO ELISA – If no or weak cytoplasmic staining of formalin fixed PMNs “Atypical pANCA” termed “atypical pANCA . Also ANCA” (antigens are other than MPO). xANCA • IBD (UC 60%, Crohn’s 20%) • Primary Sclerosing Cholangitis (60%) • Autoimmune hepatitis (30-50%) • Up to 5% of healthy controls |
|
|
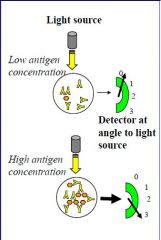
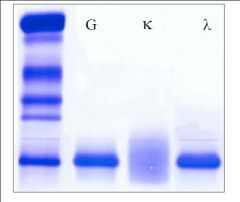
Nephelometry
Example: Immunoglobulin Quantitation Based on light scatter Principle: Light directed through a solution of immune complexes is deflected in proportion to the density of the complexes Detector in nephelometry at an angle to light source. In turbidometic assays, concentration detector is in line with light source. Requires antibody specific to analyte of interest Not accurate at low concentrations (use other methods, e.g. ELISA, for low concentration analytes) Used to measure: IgG, IgA, IgM, C3, C4, CRP, A1AT, haptoglobin, RF |
|

|

|
|
|
|
|
|
|
|
|
Waldenström's Macroglobulinemia
Clinical Presentation – Weakness, fatigue (anemia), weight loss, bleeding – Hepatosplenomegaly (20%), and lymphadenopathy (15%) – Hypercalcemia and bone pain are RARE (suggestive of IgM myeloma, rather than WM) • Differentiate based on immunophenotype and cellular morphology – Neurologic abnormalities (10%): peripheral neuropathy (distal, symmetric) with paresthesias and weakness – Hyperviscosity syndrome • Immunophenotype – Surface Ig positive – CD19+, CD20+, CD22+ – CD5(-)CD10(-)CD23(-) |
|
|
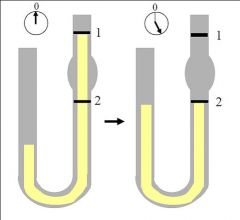
• Measure at 37 oC with
Oswald viscometer 1 1 • Measure time it takes column of liquid to flow from line 1 to line 2 2 2 using water (Tw) and patient sera (Ts) • Viscosity = Ts/Tw • Normal 1.4-1.8 |
|
|
Heavy Chain Disease (HCD)
|
Monoclonal proteins composed of an incomplete
immunoglobulin heavy chain 3 main types: α, γ, and μ SPEP/Immunofixation: Heavy chain identified without an associated light chain α Heavy Chain Disease • 2nd or 3rd decade, most patients from Mediterranean region or Middle East • GI tract involvement common – malabsorption, diarrhea, weight loss – infiltration of the lamina propria by plasma cells • Appears to be a form of MALT lymphoma with increased plasma cells • GI biopsy: villous atrophy and massive infiltration of the lamina propria of the intestine by lymphocytes, plasma cells, or immunoblasts • Bone marrow usually normal, no lytic lesions |
|
|
Bence Jones Proteinuria
• Bence Jones proteins are monoclonal, free immunoglobulin light chains (not associated with heavy chains) • Examination of the urine (and/or serum) for Bence Jones proteins is an important part of a plasma cell dyscrasia workup – Presence of BJP associated with myeloma, not MGUS – Present in 30-60% of MM patients, rarely in MGUS – BJP may also be seen in WM, amyloidosis, CLL, lymphoma – Urine Bence Jones testing more sensitive than serum Bence Jones testing – Urine dipstick insensitive to proteins besides albumin. Patients with high level BJP may be negative on urine dipstick for protein |
|

|
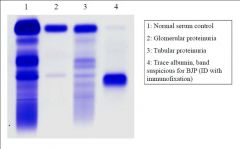
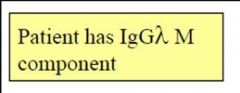
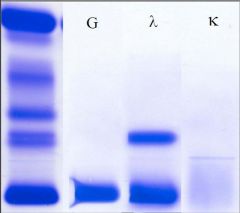
Urine Protein Electrophoresis
(Urine Concentrated 80x) |
|
|
Anti-saccharomyces cerevisiae antibodies
|
Anti-Saccharomyces cerevisiae antibodies (ASCA), along with perinuclear antineutrophil cytoplasmic antibodies (pANCA), are among the two most useful and often discriminating markers for colitis.[1] ASCA tends to recognize Crohn's disease more frequently, whereas pANCA tend to recognize ulcerative colitis.[2]
ASCA antibodies react to the following yeast proteins Mannans[3] 200 kDA glycoprotein.[4] Diseases in which ASCA are found: Behçet's disease[5] - The association with ASCA is not generally strong, but increased in patients with gastrointestinal symptoms.[6] Celiac disease[7][8] Colitis[7] Ulcerative colitis-familial.[9] Microscopic colitis Collagenous colitis[10] Crohn's disease[11][12] |

