![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
Types of phagocyte |
Neutrophils Macrophages |
|
|
Types of lymphocytes |
All white blood cells are made in bone marrow T cells - mature in thymus gland B cells - mature in bone marrow |
|
|
Types of T cells |
T helper cells T killer cells (cytotoxic T cells)
((T memory cells T regulator cells)) |
|
|
Cytokines |
Substance/ proteins secreted by T helper cells to promote phagocytosis |
|
|
Physical barriers preventing entry of pathogens |
Skin Mucus Blood clotting Wax |
|
|
Antigen |
Molecules (proteins, polysaccharides or immunoglobulin/ glycoprotein) on the surface of a cell recognised as non-self which trigger an immune response |
|
|
Would glucose be likely to act as antigen? |
No - glucose is present in all cells so cannot be used to identify cell as foreign |
|
|
Antibody |
Complex protein (4° str) produced by B lymphocytes in response to particular antigen. Have specific binding sites and can act against pathogens. |
|
|
Non specific immune response |
Fever, inflammation and phagocytosis |
|
|
Specific immune response |
Immune systen producing specific antibody after recognising type of pathogen that has entered |
|
|
Pathogen |
Disease cause organism such as virus or bacteria |
|
|
Substances the immune system would recognise as non self due to proteins or glycoprotein on cell surface |
1.Pathogen 2.Toxins (potentially dangerous products of the metabolism of pathogens) 3.Cells from other organisms- transplant rejections 4. Abnormal body cells- cancerous cells/ prevent tumour |
|
|
Antibodies can only be made my white blood cells-wht can't be made in lab like aspirin? |
Complex proteins so too large and complex to be made in lab |
|
|
How does antigen-antibody complex neutralise/ destroy a pathogen |
- label pathogen as foreign- for phagocytosis - coat pathogen so can't invade host cell - make pathogens stick together - agglutination (possible as each antibody has two antigen binding sites) - easy locate for phagocytes |
|
|
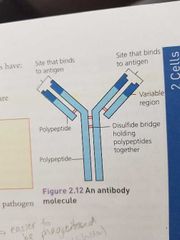
Draw antobody molecule and label |
|
|
|
List components of antibody molecule |
4 polypeptide chains (2 long, 2 short) Variable region on ends of chains Two antigen binding sites (at variable regions) |
|
|
Types of white blood cells |
Lymphocytes and phagocytes |
|
|
Phagocytes:draw appearance and what is role |
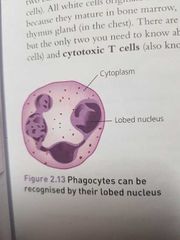
Carry out phagocytosis Lobed nucleus |
|
|
Lymphocytes role and draw appearance |
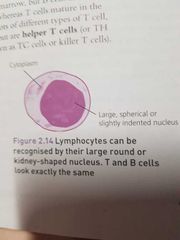
Make antibodies All lymphocytes have large round nucleus |
|
|
Phagocytosis definition |
Phagocytes engulfs and destroys a pathogen |
|
|
Phagocytosis |
- Phagocytes recognises and engulfs pathogen: - membrane folds inwards and pathogen is trapped in vacuole called phagosome. - lysosomes fuse with phagosome forming phago-lysosome. Releasing hydrolytic enzymes -enzymes digest phagocyte - remains/ nutrients ejected from cell via exocytosis or absorbed into cytoplasm |
|
|
Lysosomes |
Small vesicles containing hydrolytic enzymes: lysozymes |
|
|
Compare two types of defence mechanisms |
1. Non-specific: - immediate - same for all pathogens - physical barrier - phagocytosis 2. Specific: - slower response - specific to each pathogen - cell mediated: T lymphocytes - humoral: B lymphocytes |
|
|
Active immunity |
Immune system activated and produces own antibodies -slow -long lasting 1. Natural - immunity from antibodies made after infection - immune response, will be immune to disease after 2. Artificial - antibodies made after vaccine injection (Weak/ attenuated strand of virus, activate immune system to produce own antibodies) |
|
|
Passive immunity |
Antibodies made from outside source are injected/ ingested Immunity acquired immediately, no lasting immunity (no memory cells, antibodies not replaced when broken down) 1. Natural: Antibodies to babies via placenta or breast milk - useful yr 1 baby's immune system still developing 2. Artificial Injection of antibodies made by another individual |
|
|
Heard immunity concept |
Majority of population are vaccinated so hard for pathogen to spread within the pop. Unlikely susceptible individual will come into contact with infected person. |
|
|
Why is herd immunity useful in society/ large population |
Not all can be vaccinated: - Babies and young children- not fully functional immune system - dangerous to vaccinate ill ppl or with compromised immune system |
|
|
How best to achieve herd immunity? |
Vaccinate all at one time so in certain period, only few people have the disease, transmission of pathogen interrupted |
|
|
Reasons vaccination may not eliminate disease |
-antigenic variability - pathogen mutate frequently, antigen change- no longer recognised by immune system - individuals pass devleop disease in gap between being vaccinated and immune response so pass on disease - individuals object to vaccine - individuals have defective immune system - immunity not induced - too many varieties of a pathogen to develop vaccine against all |
|
|
Cellular response/ cell mediated response: |
1. Recognition: pathogen invades body cell or engulfed by phagocytes 2. Cell becomes antigen presenting cell - presents the antigens on cell membrane 3. Receptors on specific Helper T cell fit onto antigen (complimentary) 4. Attachment activates T cells to ÷ mitosis = clones (same receptors) 5. The cloned T cells: - activate cytotoxic T cells - develop into memory cells - stimulate B cells to ÷ and secrete antibodies (humoral) - stimulate phagocytosis |
|
|
How do killer t cells work |
Produce perforin (protein) - makes holes in cell membrane No control over membrane transport = cell death |
|
|
How T lymphocytes can distinguish different invader cells (to then carry out cellular response) |
- phagocyte engulfs pathogen = APC - virus invades body cell --> cell presents viral antibodies -transplanted cells have diff antigens on surf mem -cancer cells differ from normal cells so have diff antigens |
|
|
How Lymphocytes don't kill other self/host cells |
Don't have receptors that match other host cells |
|
|
Meaning behind humoral and cell mediated |
Humoral- involves b lymohocytes producing antibodies ( in plasma) Cell mediated - t lymphocytes only recognise antigens on cells |
|
|
Humoral response |
1. Endocytosis- antigen enters B cell B cells acts as APC 2. Helper T cells bind and stimulate B cell to ÷ mitosis (clonal selection) 3. Large no. Cloned PLASMA CELLS produced: all produce antibody specific to antigen 4. Antibody attaches to antigen on phagocytes = destroy (**see antigen-antibody complex card**) 5. Some B cells develop into memory cells (2° resp)
|
|
|
2° response vs 1° Also draw graph |
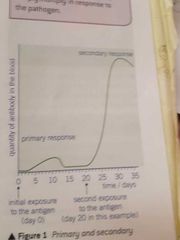
(2°) Memory cells live > plasma cells (1°)
2° no lag in immune response (destroyed before cause harm) Antibodies produced faster and in larger quantities & for longer (second exposure stimulates memory cells to ÷ rapidly develop into plasma cells --> secrete specific antibodies) Memory cells circulate in blood and tissue fluid waiting but dormant until |
|
|
Clonal selection and expansion |
Selction - Choose corresponding B cells to antigen Choose- selected cell proliferates and divides into memory cells and plasma cells |
|
|
Flu virus antigenic variability |
Mutate/ later surface proteins ∴ no immune response (new antibodies needed) |
|
|
Types of vaccines/immunizations may contain |
- dead pathogens -attenuated pathogens - purified antigens All trigger 1° real-->memory cells in place -->antibodies fight infection before symptoms appear |
|
|
How does having diff lymphocytes = able to fight several diff diseases |
Each lymphocyte has diff shaped receptors ob cell surface and so produce antibodies to bind to diff antigens. Each cell has one type of receptor or antibody so lots slighly genetically diff = respond to diff pathogens |
|
|
Every one pathogen has how many diff receptor on membrane? Monoclonal antibodies meaning |
Hundreds of diff receptors on membrane so hundreds of antibodies could be produced by B lymphocytes. One type of antigen specific antibody is isolated and cloned outside the body |
|
|
Ethics of vaccines and monoclonal antibodies |
Production involves mice -inducing cancer in them Deaths are a risk - early treatment of MS of treatment may be unsuccessful (overestimate immune system) Unexpected consequences ie patients 2006 organ failure from MA study
Vaccines: Ppl refuse religious - may put others at risk --- heard immunity not effective -- if % vaccinated pop low, may not stop chain of transmission |
|
|
Structure of HIV |

Glycoproteins/ attatchemnet proteins |
|
|
Why HIV belong to retrovirus classification |
Contain RNA so must convert RNA to DNA using reverse transcriptse |
|
|
Replication of HIV |
-HIV attatchemnt protein binds CD4 (protein) on T helper cells (though CD4 is present on other cells too) - HIV capsid fuse w/ cell surface mem: HIV's RNA and enzymes enter - rev tran: RNA --> DNA and inserted into cells DNA - uses cell's enzymes make mRNA coding for new viral proteins -- use cells protein synthesis - synthesized HIV particle moves away from T cell - uses it's cell membrane for lipid envelope |
|
|
How HIV causes symptoms of AIDS |
AID suffered have low T cell counts - When invade and replicate in helper T cells, the pop of T cells decrease (can't reproduce/ killed) - were important in cell mediated immunity -can't stimulate B cells into antibody production or T killer cells to kill pathogen -immune response not effective ---> suseptable to infections |
|
|
Why antibiotics ineffective HIV 3 reasons Vs against bacteria |
Damage prokaryotic organelles, (not eukaryotic): inhibit enzymes required for synthesis of peptide cross linkages in bacterial cell walls (murein) Not viruses: 1. No internal organelles or metabolism to target (since rely on host to carry out metabolic activities) 2. Have protein coat not murein - not sites for antibiotics 3. Virus are within the own organelles cells so antibodies can't reach them |
|
|
ELISA test Purpose |
Detect presence and quanitiy of protein in sample |
|
|
ELISA steps |
1. Add sample to surface where will attach e g slide 2. Wash surface - remove unattached molecules 3. Add antibody spec to target protein 4. Wash -remove unattached antibodies 5. Add antibody (+enzyme) which attaches to other antibodies 6. Add colourless substrate--enzyme--> coloured products 7. Amount relative to intensity of colour |
|
|
Uses monoclonal antibodies |
1. Pregnancy tests: detects hCG (prod placenta) in urine. On test strip: monoclonal antibodies linked to colour compounds - hCG-antibody-colour complex = colour change 2. Medical diagnosis: blood sample and use monoclonal antibodies that interact with the antigen |
|
|
Monoclonal antibodies and targeted medication |
Monoclonal antibodies produced that are spec to antigens on cancer cells Attatch to receptor then block chemical signals that stimulate uncontrolled growth |

