![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
intramembranous
|
starts as fibrous tissue. osteoblasts in the periosteum secrete osteoid. bone grows circumferentially
|
|
|
endochondral
|
starts as cartilage - influx of vessels, osteoblasts, osteoclasts - mineralization of osteoid
|
|
|
Unique physes
|
- wings of ilium do not fuse completely in some dogs
- radial physis - normal undulating shape - ulnar physis - conical shape |
|
|
technique for skeletal rads
|
high contrast (low kVp, high mAs)
slow film-screen combo, more detail motion is usually a problem intensifying screen position over area of concern * always do orthogonal view! |
|
|
land marks of cervical spine
|
C1 - wings
C2 - dens, spinous processes C6 - transverse processes disk spaces get larger caudally |
|
|
land marks in thoracic spine
|
intercapital lgaments
T11 - anticlinal vertebra (no slope) T10-11 disk space is always narrow |
|
|
Approach to spinal rads
|
A - alignment
S - soft tissues P - processes I - internal; size, margin, opacity N - nerves/spinal cord; intervertebral foramina E - external margins - shape, size, margin and opacity of vertebral bodies and disc spaces |
|
|
why do imaging?
|
"the big D's"
- Detection - Description - Differentials - Diagnosis |
|
|
cutting cone
|
subunit of bone responsible for resorptino and formation of mature lamellar bone
makes new osteons |
|
|
normal blood supply to bone
|
- nutrient artery through nutrient foramen
- entheses (muscle attachment) - periosteum (minor in normal state) |
|
|
how does blood leave bone?
|
entheses
- damage to entheses can significantly affect circulation to bone - congestion causes inc in intramedullary pressure - very painful! |
|
|
approach to appendicular skeleton interpretation
|
A - alignment
B - bone (periosteum, cortex, medullary cavity) C - cartilage/joints (ligaments, spaces, periarticular margins) S - soft tissue (intra vs extracapsulare enlargement, gas or mineralization) |
|
|
causes of extracapsular soft tissue enlargement
|
edema
hemorrhage inflammation tumor |
|
|
cuases of soft tissue mineralization
|
dystrophic mineralization
metastatic mineralization neoplastic mineralization |
|
|
causes of gas in the soft tissues?
|
septic process
open wound (big dog-little dog syndrome) recent surgery |
|
|
bone response to infection or trauma
|
"ARF"
A - activation R - resorption F - formation Juvenile bone reacts in 5-7 days Adult bone reacts in 7-10 days |
|
|
endosteal proliferation of bone
|
sclerosis
|
|
|
classification of periosteal reactions
|
- active/aggressive - indistinct margins (spiculated, amorphous, etc)
- inactive/non-aggressive - well-defined margins, smooth older lesions are smoother and more opaque |
|
|
causes of generalized bone loss
|
meatbolic disease
nutritional disease disuse |
|
|
how much bone loss is required to notice radiographic changes
|
30-60%
|
|
|
causes of localized bone lysis
|
trauma
infection tumor |
|
|
parts of the joint to evaluate
|
ligamentous and capsular attachments
joint space periarticular margins |
|
|
characteristics of a non-aggressive lesion
|
- found anywhere
- solid, smooth periosteal reaction - geographic bone lysis (>10 mm area, well defined margins; usually medullary - may displace cortex, but does not destroy it) - short and distinct zone of transition - changes slowly over time |
|
|
causes of non-aggressive bone lesions
|
bone cyst - cause unknown
benign tumor cartilaginous exostoses |
|
|
characteristics of an aggressive lesion
|
- located in meatphysis (sometimes diaphysis)
- periosteal reaction - rough/spiculated (lamellar, sunburst, amorphous), codman's triangle - moth eaten or permeative lysis - cortical destruction - changes rapidly - long, indistinct zone of transition |
|
|
causes of aggressive bone lesions
|
Primary neoplasia
Metastatic neoplasia Fungal infection Bacterial infection Protazoal infection |
|
|
fracture classification
|
L - location
E - external communication (open or closed) G - general direction (transverse, oblique) E - extent of damage (complete or incomplete?) N - number (simple or comminuted) D - displacement (of the distal piece) |
|
|
how can you tell that a fracture is open (on a radiograph)?
|
look at the soft tissues
- gas adjacent to the fracture segments |
|
|
A single fracture appears to have several different fracture lines going in different directions. What direction is this fracture?
|
Spiral
|
|
|
complications of salter harris fractures
|
bone foreshortening
angular limb deformities |
|

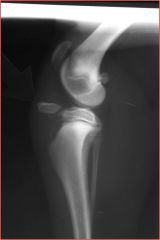
Classify this fracture
|
distal diaphysis of the right humerus
closed oblique complete comminuted (see more than one piece) cranial (can't see this with one view), lateral, proximal |
|

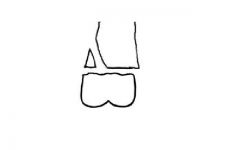
Salter-Harris type?
|

Type 1
|
|
Salter-Harris type?
|
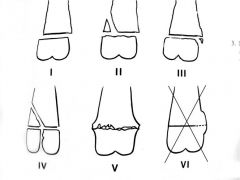
Type 2
|
|

Salter-Harris type?
|
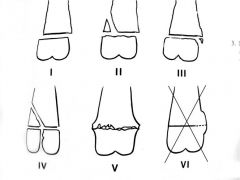
Type 4
|
|

Salter-Harris type?
|

Type 5
|
|

Salter-Harris type?
|
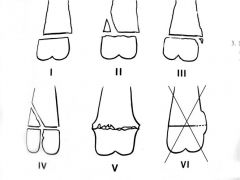
Type II - crosses the physis and part of metaphysis
|
|

Salter-Harris type?
|

Type V - see a step at the back of tibia and don't see the thin line of cartilage due to crushing fracture
|
|
fracture type?
|
avulsion fracture
|
|

classify this fracture
|
pathologic fracture
- recognize lucent, thin cortices - not much blastic activity going on - no history of trauma |
|
|
causes of pathologic fractures
|
- tumors
- infections - metabolic diseases (hyperparathyroidism) |
|

fracture type?
|
folding fracture
|
|

fracture type?
|
pathologic fracture secondary to osteosarcoma
|
|
|
primary bone healing
|
- osteonal remodeling
- nearly perfect apposition and alignment required - must be aseptic - early return to function - takes >6 months to return to original strength - cannot see radiographically |
|
|
Secondary bone healing
|
- less than perfect reduction, stability or infection
- cartilage bridge formed first - bony callus formed by endochondral ossification - takes longer to reach functional strength than primary - reaches full strength earlier than primary (6-8 weeks) |
|
|
approach to evaluating fracture healing
|
ABCD's
A - alignment B - bone C - cartilage D - DEVICE S - soft tissue |
|
|
expected radiographic findings for a healing fracture EARLY in healing process
|
widening of fracture line
callus formation |
|
|
expected radiographic findings for a healing fracture LATE in healing process
|
opaque, mature callus
increased mineral opacity within the fracture line |
|
|
fracture complications
|
- abnormal healing (malunion, delayed or non-union, angular limb deformity)
- sequestrum formation - implant failure |
|
|
Lesions associated with hypertrophic osteophaty (HO)
|
1. Manifestation of primary disease:
- thoracic lesion (lung tumor, non-neoplastic lung disease) - abdominal lesion (bladder neoplasia) 1. Radiographic findings: - rough periosteal new boen formation - diaphyseal region of the long bones - typically starts distally |
|
aggressive or non-aggressive?
|
aggressive
|
|

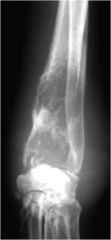
aggressive or non-aggressive?
|
aggressive
|
|

aggressive or non-aggressive?
|
non-aggressive
|
|

classify the lysis and comment on aggressiveness of lesion
|
geographic lysis, least aggressive
|
|

classify the lysis and comment on aggressiveness of lesion
|
moth-eaten lysis, aggressive lesion
|
|

classify the lysis and comment on aggressiveness of lesion
|
permeative lysis, aggressive
|
|

classify the lysis and comment on aggressiveness of lesion
|
cortical destruction, more aggressive than the other forms that don't destroy the cortex
|
|
|
radiographic signs of joint disease:
|
1. increased capsular thickness or effusion
2. perichondral (marginal) osteophytes 3. Enthesophytes 4. Subchondral erosions 5. Mineralized joint bodies 6. Subchondral bone opacity 7. Subchondral bone cysts 8. Joint space narrowing |
|
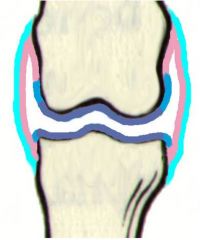
where would you find perichondral osteophytes?
|
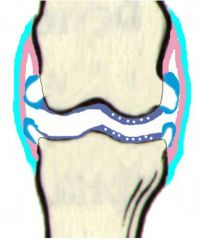
at the light blue bit - looks like a bald man's head
|
|
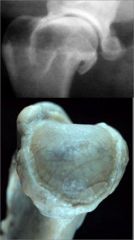
what's wrong with these bones?
|
perichondral osteophytes (bald man's head)
|
|

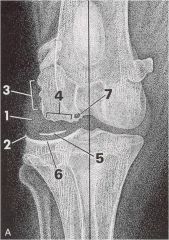
what sign of joint disease can you see in this radiograph?
|
enthesophyte at attachment of cranial cruciate
|
|

what's the sign of joint disease in this stifle?
|
decreased subchondral bone opacity
|
|

what's the sign of joint disease here?
|
mineralized joint body
|
|
|
what kinds of things can cause mineral opacity in a joint space?
|
- joint mice
- avulsed fragments of articular or periarticular bone - osetochondral component - synovial osteochondroma |
|
|
what can cause increased subchondral bone opacity in joint disease?
|
- osteosclerosis or eburnation
- stress remodeling |
|

what's the sign of joint disease in this joint?
|
increased subchondral bone opacity (osteosclerosis/eburnation or stress remodeling)
|
|

what's the sign of joint disease in this joint?
|
subchondral bone cyst (proliferation of synovium invades subchondral bone)
|
|

what's the sign of joint disease in this joint?
|
altered thickness of the joint
|
|
|
disk spaces that are normally narrow
|
C2-C3
C7-T1 T10-T11 |
|
|
ligaments of the cervical spine
|
- dorsal alanto-axial ligament
- transverse ligament of the dens - maintain stability and protect spinal cord |
|
|
ligaments of the spine
|
1. dorsal longitudinal ligament
- ventral floor of the spinal canal - CVM-I Syndrome 2. Intercapital ligaments - between heads of ribs - help prevent disc herniation in the thoracic spine |
|
|
standard protocol for spinal radiographs
|
collimate to include area of interest
center x-ray beam - cervical spine (C3-C4 and C7-T11) - thoracic spine (T6-T7 and T13-L1) - lumbar spine (L3-L4) |
|
|
correct positioning of lateral spinal view
|
- transverse processes superimposed
- intervertebral foramen uniform size - rib heads superimposed |
|
|
correct positioning of the ventrodorsal spinal view
|
- dorsal spinous process centered over vertebral body
|
|
|
important regions of the skull to evaluate:
|
teeth
mandible nasal cavity sinuses tympanic bullae calvarium |

