![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
|
Which form of hypertension is a risk factor, rather than a disease?
|
Primary hypertension, or Essential Hypertension (EH).
|
|
|
What is a high BP?
|
Important to take account for normal BP - e.g. white coat hypertension.
140/90 is high blood pressure generally |
|
|
How do you diagnose high BP?
|
On basis of 'usual' BP taken on several occasions.
|
|
|
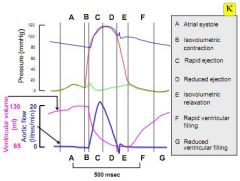
What are the 7 phases of the cardiac cycle?
|
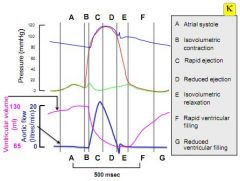
A - Atrial systole
B - Isovolumetric contraction (beginning of Ventricular systole) C - Rapid ejection D - Reduced ejection E - Isovolumetric relaxation (beginning of ventricular diastole) F - Rapid ventricular filling G - Reduced ventricular filling |
|
|
Which valves are open and which are closed in phase A of the cardiac cycle?
|
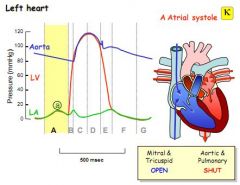
A - Atrial systole. The Aortic and pulmonary valves are closed, and the mitral and tricuspid valves are open.
|
|
|
Which valves are open and which are closed in phase B of the cardiac cycle?
|
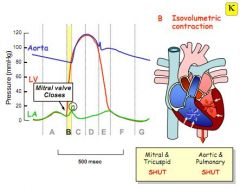
None are open. Isovolumetric contraction means that the initial ventricular pressure of contraction is less than that beyond the aortic and pulmonary valves, hence the ventricles are full and in systole, but none of the valves are open.
|
|
|
Which valves are open and which are closed in phase C of the cardiac cycle?
|
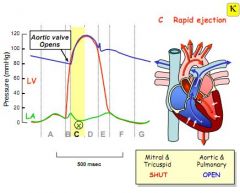
Rapid ejection phase. The aortic and pulmonary valves open as the pressure inside the ventricles exceeds that outside the valves, blood spurts out rapidly.
|
|
|
How much of ventricular filling is usually due to atrial contraction, what else contributes, and when might this change?
|
20% normally due to atrial contraction, the remainder is venous pressure. When heart rate rises diastole is shorter, so the ventricles fill less, making the atrial contribution higher/more important.
|
|
|
What causes the t-wave?
|
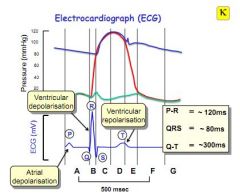
Repolarisation of ventricular muscle during the second half of systole (reduced contraction phase)
|
|
|
What causes the p-wave?
|
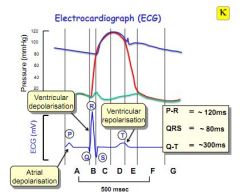
Atrial depolarisation.
|
|
|
What is end diastolic volume and pressure and how might they differ right to left?
|
End diastolic volume is the amount of blood in the ventricles after diastole (filling), in essence the capacity of the heart. End diastolic pressure is the amount of pressure generated by that volume of blood at the end of diastole (filling).Higher in left over right as it is bigger.
|
|
|
What is a typical EDV and EPD?
|
EDV - 120-140ml, EDP - <10mmHg
|
|
|
What is the dicrotic notch?
|
Backflow of blood into the left ventricle as the aortic valve shuts.
|
|
|
What is the ejection fraction and what is a typical stroke volume?
|
EDV is typically 120-140ml. A typical stroke volume is 70ml.
The ejection fraction is the proportion of blood which filled the ventricle ejected in systole, or typically 70/120. |
|
|
What is the proportion of diastole to systole and how might this change as heart rate increases?
|
Diastole is usually double systole. This ratio gets smaller as heart rate increases, as the heart cannot fill as much as it is beating faster.
|
|
|
In a pressure volume loop, what does the bottom line demonstrate?
|
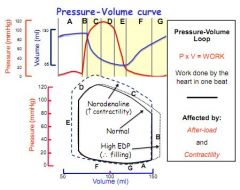
Ventricular filling during the relaxation phase. Filling is facilitated by compliance of the muscle, so if this line is steep, it may indicate fibrosis.
|
|
|
Where might you notice signs of heart failure on a patient lying down in bed?
|
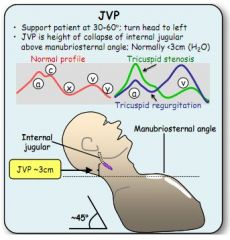
The jugular venous pulse, in the neck around 3cms above the manubriosternal angle.
|
|
|
What are the four heart sounds?
|
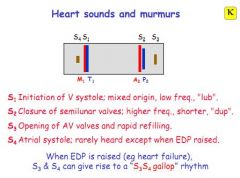
S1 - initiation of ventricular systole (LUB)
S2 - closure of the semi-lunar valves (aorta and pulmonary) (DUP) S3 - opening of AV valves S4 - Atrial systole (rarely heard) |
|
|
What might you hear in heart failure
|
An S3-S4 gallop.
|
|
|
What might you suspect from a split S1 sound?
|
Delayed conductance through the bundle of His.
|
|
|
What might you suspect if the gap between S1 and S2 is wide?
|
Pulmonary hypertension or stenosis.
|
|
|
What causes murmurs, and what might cause a diastolic or systolic murmur?
|
Turbulence, so not always pathological - either stenosis or leakage. A diastolic murmur would be mitral stenosis, a systolic murmur would be aortic stenosis. A soft S2 might indicate aortic incompetence.
|
|
|
What two cell types make up blood vessels?
|
Endothelial cells - regulate smooth muscle, control movement of substances across the barrier
Smooth muscle controls diameter. |
|
|
What are the three layers in a typical muscular artery and what does each contain?
|
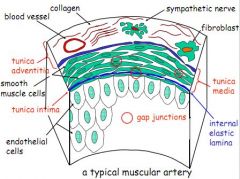
Tunica intima (lumen facing) - mono-layer of endothelial cells
Tunica media - smooth muscle Tunica adventitia - connective tissue, blood vessels, collagen and nerves |
|
|
What is the diameter of a typical capillary and a vein?
|
Capillary - 8uM, vein e.g. 5mm.
|
|
|
Do capillaries contain nerves and smooth muscle?
|
No.
|
|
|
What forms the scaffold of smooth muscle cells?
|
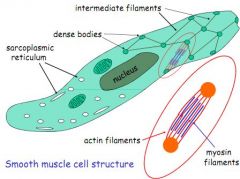
Dense bodies connected by actin and myosin filaments.
|
|
|
Name some key vasoconstrictors and dilators.
|
Vasoconstrictors - Histamine, NA, Adrenalin, Angiotensin 2, ADH
Vasodilators - NO, bradykinin, prostaglandins, substance P |
|
|
What 2 things do smooth and striated muscle have in common?
|
Triggered by Ca2+ contraction, contain actin and myosin filaments
|
|
|
List 5 ways that smooth muscle is different to striated muscle?
|
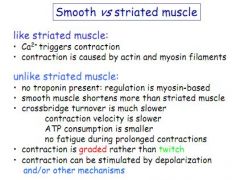
|
|
|
Describe excitation-contraction coupling in smooth muscle cells.
|
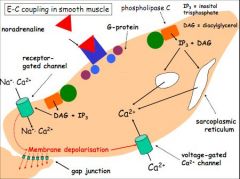
Vasoconstricting agonist activates the process - most commonly NA on Alpha-adrenergic receptor.
G-protein receptor > Phospholipase C > IP3 and Diacylglycerol (DAG). IP3 > SR channels release lots of Ca2+ DAG > cation channels, influx of Na+ and Ca2+. Membrane depolarisation - L-type Ca2+ channels open, depolarisation can spread to other neighbouring cells |
|
|
Which enzyme phosphorylates myosin?
|
Myosin Light Chain Kinase.
|
|
|
What substance is released by the endothelium to relax smooth muscle?
|
Nitric Oxide (formerly Endothelium Derived Relaxing Factor)
|
|
|
What might trigger endothelial cells to release NO?
|
Vasodilating substances, such as bradykinin, or shear forces cause by high pressure (in veins only)
|
|
|
How does NO released by endothelial cells trigger relaxation of smooth muscle?
|
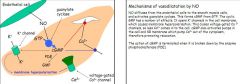
Activates Guanylate Cyclase, this make cGMP from GTP. cGMP opens K+ channels, hyperpolarising smooth muscle cell membranes closing Ca2+ channels, it also activates pumps to remove Ca2+.
|
|
|
What enzyme breaks down cGMP?
|
Phosphodiesterase.
|
|
|
What is the general effect of oxidative stress?
|
Impaired endothelial function - Superoxide reacts with NO to form Peroxynitrite - prevents NO mediated vasodilation, so stops blood vessels dilating properly.
|
|
|
Describe the pathway for smooth muscle relaxation by factors other than NO (known as Endothelium Derived Hyperpolarisation)
|
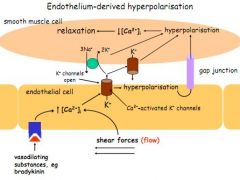
Endothlium Derived Hyperpolarisation respond to the same stimuli as NO (vasodilating substances, shear forces).
These raise Ca2+ in the endothelium, which opens K+ channels. K+ out hyperpolrises the endothelial cells, and this has a know on effect on smooth muscle - hyperpolarising and relaxing smooth muscle by lower intercellular Ca2+ |
|
|
List 4 functions of the endothelium of blood vessels?
|
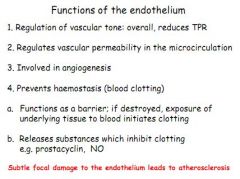
Regulate vascular tone
Regulate permeability Involved in angiogenesis Prevents haemostasis/clotting |
|
|
Other than NO, how else might blood vessels be relaxed?
|
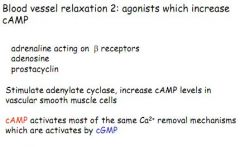
Agonists which increase cAMP - adrenalin on B-receptors, adenosine and prostacyclins
Stimulate Adenylate cyclase, which increases cAMP, which works like cGMP |
|
|
What is metabolic hyperaemia?
|
Increased metabolism in exercise causes release of local vasodilators which act on arterioles - K+, H+, CO2, lactic acid
This helps keep flow to active muscle over inactive sites. |
|
|
What is reactive hyperaemia?
|
When blood flow is cut off, e.g. in a stroke or MI, metabolites accumulate to enhance blood flow by vasodilation. When blood flow resumes, these factors enhance perfusion until they are washed away.
|
|
|
List 2 systemic mechanisms for regulating the vasculature, and 2 local ones.
|
Systemic - Autonomic Nervous System, Renin-Angiotensin-Aldosterone
Local - Myogenic response, metabolic and reactive hyperaemia |
|
|
What is the myogenic response, or Bayliss effect?
|
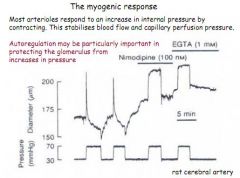
Response to stretch in vascular cells, which detect raised pressure and respond by contracting.
|
|
|
Describe the effects of sympathetic and parasympathetic stimulation a) heart and b) vasculature (and give receptors!).
|
A) Heart - SNS increases rate and contractility - Beta-1
Heart - PNS decreases heart rate via muscarinic receptors B) Vasculature - SNS causes constriction, e.g. splanchnic, renal, cutaneous and muscle systems Vasculature - PNS - Causes vasodilation e.g. salivary glands, penis, GI, pancreas |
|
|
The ANS is said to be the effector arm of the baroreceptor reflex, explain this.
|
It works at rest to maintain a constant blood pressure in response to changes detected in the vasculature.
|
|
|
As well as maintaining constant BP, list three other useful functions of ANS control of the vasculature.
|
Maintain pressure when standing up/bleeding
Increasing CO in exercise Thermoregulation |
|
|
Which is more important during the sympathetic response, NA or Adr?
|
NA is more important than adrenalin during a sympathetic response.
|
|
|
List the receptors which NA and Adrenalin work on and give their effects.
|
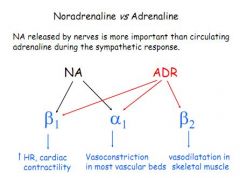
Beta-1 - Raises heart rate and contractility (NA and Adr)
Alpha-1 - Vasoconstriction of most vascular beds (NA and Adr) Beta 2 - Vasodilation of skeletal/coronary muscle (Adrenaline only) |
|
|
When is adrenalin important?
|
Fight or flight, exercise, hypotension and hypoglycaemia.
|
|
|
How does angiotensin 2 work on the vasculature and via what receptor?
|
Via Angiotensin 2 - receptor type 1 (AT1), cause vasoconstriction
|
|
|
Briefly describe the RAAS.
|
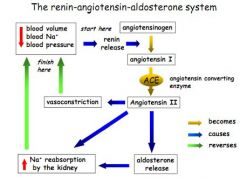
Renin cleaves Angiotensinogen (from liver) to Angiotensin 1
Angiotensin 1 is converted to Angiotensin 2 by ACE (lungs) Angiotensin 2 is a vasoconstrictor, which stimulates the adrenal glands to produce Aldosterone Aldosterone stimulates Na+ reabsorption in the kidney -increasing BP, blood volume and Na+ levels |
|
|
Describe the two main effects of ADH and their receptors.
|
Act on V2 receptors in the DCT/collecting duct, stimulating cAMP, expression of Aquaporins and H2O reuptake
Act on V1 receptors in the vasculature to cause vasoconstriction |
|
|
What are prostanoids, and which ones do what?
|
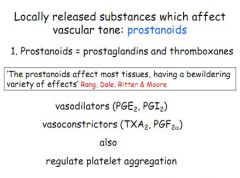
Locally released substances which affect vascular tone.
PGE2 and PGI2 - vasodilate in inflammation, TXA2 and PGF2 vasoconstrict in thrombosis |
|
|
What are the common precursors to all PGs?
|
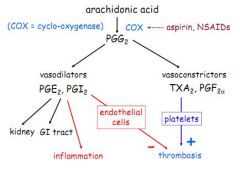
Arachidonic acid, cleaved to PGG2 by COX
|
|
|
How does histamine affect vascular tone?
|
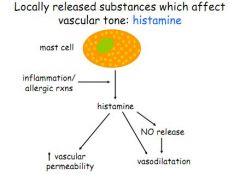
Released by mast cells in type 1 hypersensitive reaction, increases permeability and vasodilation via NO.
|
|
|
How is the brain vasculature structurally adapted?
|
Circle of willis provides all blood flow to brain
Highly perfused organ with dense capillaries BBB stops lots of substances which might interrupt flow |
|
|
How is the brain vasculature functionally adapted?
|
Strong metabolic hyperaemia (ensures blood flow parallels cortical activity)
Weak regulation by ANS Standing displaces CSF, lowering intracranial pressure and preventing venous collapse. |
|
|
Describe structural and functional adaptations in the coronary vasculature.
|
Structural:
Ischemia promotes formation of coronary collaterals Heart has high capillary density Functional: Strong metabolic hyperaemia Adrenalin reinforces this by acting on B2 receptors Lots of O2 extraction, more than normal tissue. |
|
|
When does blood flow to the left ventricle occur and why is this a problem when the heart rate increases?
|
Only occurs in diastole. Diastole shortens as heart rate increases, which can cause ischemia.
|
|
|
How does the SNS regulate skin perfusion?
|
SNS controls areteriovenous anastamoses in the skin, when hot, these open, causing increased perfusion and loss of heat.
|
|
|
How much blood flow can the skin lose without any effect?
|
90%, hence in haemorrhage, the skin goes cold, pale and clammy as blood is diverted elsewhere.
|
|
|
What is pulse pressure?
|
Systole - distole = Pulse pressure
|
|
|
What is mean arterial pressure (MAP)?
|
Diastole + (systolic-diastolic)/3 = MAP
|
|
|
Mean arterial pressure is used in equations related to what?
|
MAP = CO x TPR, or, CO = MAP/TPR
|
|
|
What does systolic pressure reflect?
|
Cardiac function and artery compliance.
|
|
|
What does diastolic pressure reflect?
|
Total peripheral resistance.
|
|
|
What is the effect of gravity on arterial blood pressure?
|
Weight of column of blood means that mean arterial pressure is double in the legs what it is at the heart, and 2/3rds in the head what it is in the heart.
|
|
|
Is the diastolic pressure taken with a sphygmomanometer accurate?
|
No, the real diastolic is about 8mmHg more.
|
|
|
Which part of the brain stem controls BP?
|
Nucleus tractus solitarius
|
|
|
Which nerves feedback info on BP from the carotid sinus, and aortic arch?
|
Glossopharyngeal - carotid sinuses
Vagus, aortic arch |
|
|
What mechanism helps control acute BP changes?
|
Baroreceptor reflex.
|
|
|
What are the type of receptors involved in the baroreceptor reflex, what do they detect and how do they influence blood pressure?
|
Mechanoreceptors in the carotid sinuses and aortic arch detecting stretch. Reduced stretch = reduced firing, increased strecth = increased firing. Most sensitive to small changes in normal BP.
|
|
|
Do baroreceptors adapt?
|
Yes, after a few hours the set point in the brain stem will be adjusted to the new level, hence exercise is effective.
|
|
|
What effect does posture have on BP, CO and CVP?
|
Blood pools in legs, causing reduced CVP, reduced CO and therefore reduced BP.
|
|
|
What 4 factors are thought to control blood volume as part of long term BP control?
|

Na+ and H2O
Cardiopulmonary stretch receptors (blood volume) Baroreceptors in carotid sinus (arterial blood pressure) Pressure naturesis (raised renal artery pressure increases Na+ and H2O loss) |
|
|
Define the role of osmoreceptors.
|
Osmoreceptors in the hypothalamus respond to changes in plasma osmolality by either increasing thirst, releasing ADH, increasing Na+ reuptake.
|
|
|
What senses changes in blood volume?
|
Cardiopulmonary receptors in the atria and ventricles measure blood volume.
|
|
|
What is the main similarity and the key difference between the Guyton and RAAS models for the long term control of BP?
|
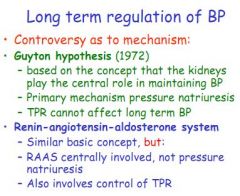
Both have the kidneys playing the main role.
In the Guyton model, pressure natriuresis plays the key role, whilst the RAAS plays the key role in the other hypothesis |
|
|
Contrast the effects of the baroreceptors and cardiopulmonary receptors by reference to effects of denervating each set of receptors.
|
Denervating baroreceptors only slightly alters MAP, but variations are possible, indicating they are involved in immediate tweaking.
Denervating cardiopulmonary receptors causes sustained hypertension + increased variability. |
|
|
What are the two types of hypertenion and what what are possible causes?
|
Primary/essential (90% of cases), genetic/environmental - salt, stress etc
Secondary (10%), due to renal stenosis, or endocrine (birth control etc) |
|
|
What are the two main strategies for treating hypertension?
|
Lifestyle (cut NaCl, exercise etc), and drugs to reduce sympathetic stimulation, stop angiotensin 2/aldosterone, increase cpacity for kidneys to exceret urine, reduce vascular tone and lower blood volume.
|
|
|
What is a common duiretic used to treat hypertension, what are its effects and side effects, indications/contraindications?
|
Thiazide-type diuretics, increase kidney NaCl and H2O excretion, lowers blood volume and CO. TPR falls by an unknown mechanism. Side effect - hypokalaemia. Good in elderly, bad in gout.
|
|
|
List 4 B-blockers and the receptors they work on?
|
Propanolol - non-selective B-blocker
Atenolol - B1 selective-blocker Pindolol - Partial agonist, blocks B1, stimulates B2 Carvedilol - B1 and A1 blocker |
|
|
What are the main effects of beta-blockers, side effects, indications and contraindications?
|
Block sympathetic stimulation to heart, lowering CO. Also reduce renin, angiotensin 2. Can cause fatigue and bronchospasm, also cardiac depression. Good in angina and post-MI, bad in asthma (as they block B2).
|
|
|
What are the sites of action of the main types of anti-hypertensives?
|
1) ACE-inhibitors and Angiotensin 2 receptor blockers all prevent angiotensin 2 binding the smooth muscle cell
2) Thiazide diuretics reduce blood volume/venous return/CO 3) Ca2+ channel blocker - reduce the plateau phase, lowering force of contraction 4) B-blocker, act on B1 to reduce SNS stimulation, lowering rate and contractility Also: K+ channel agonists working on the vasculature to help to prevent depolarisation induced contraction Alpha-1 selective antagonist, which act on vascular smooth muscle to prevent SNS induced constriction (but do not block Alpha-2 mediation of circulating NA) Finally: Methyldopa, an NA analogue which activates alpha-2, reducing NA release (used in pregnancy as doesn't affect foetus) Also Clonidine by the same action, used as a sedative |
|
|
What is a common ACE-I used to treat hypertension, what are its effects and side effects, indications/contraindications?
|
Enalapril. Block conversion of Angiotensin 1 to angiotensin 2, inhibit bradykinin breakdown.
Cause a dry cough. Indicated in post MI, heart failure and diabetes. Contraindicated in pregnancy, renal failure. |
|
|
What is losartan?
|
ARB - as an ACE, but better... no cough.
|
|
|
Give a type of calcium channel blocker which is vascular selective, and one which is not, give effect/side effects, indications and contra-indications.
|
Vascular selective - Amlodipine
Non-vascular selective (so also heart) - Verapamil Inhibit arteriole constriction by blocking opening of voltage gated Ca2+ channels. Selective - Tachycardia/headache Non-selective - Bradycardia. Indicated in angina, contraindicated in heart failure/pregnancy |
|
|
What effects/side effects might you expect from an alpha-1 receptor blocker?
|
Block SNS constriction of arterioles. Also postural hypertension, ankle oedema, drowsiness.
|
|
|
What are the 4 adrenergic receptors and what do they mediate?
|
Alpha-1 - Smooth muscle contraction, vasculature
Alpha-2 - Smooth muscle contraction, cardiac relaxation, inhibition of NA when levels are high Beta-1 - Cardiac contractility Beta-2 - Smooth muscle relaxation |
|
|
Why are selective alpha-1 blockers preferred to non-selective?
|

Alpha 2 receptors feedback to reduce circulating levels of NA when levels are high.
Non-selective alpha-blockers inhibit this feedback, leading to raised circulating NA, which works on B1 to cause tachycardia and increased CO Selective Alpha-1 blockers achieve the vasodilatory effects, without affecting the Alpha-2 receptors, so circulating NA levels remain normal. |
|
|
How do methyldopa and clonidine work and why is this useful for pregnant hypertensives?
|
Stimulate alpha-2, reducing SNS stimulation and lowering CO. Doesn't cross placenta and no effect on foetus.
|
|
|
Why aren't K+ channel agonists used more?
|
Very powerful anti-hypertensive, used as treatment of last resort.
|
|
|
What are the current prescribing guidelines for hypertension?
|
Patient under 55 - ACE-I, Ca2+ blocker or diuretic, all three, then add b-blocker
Patient over 55 - Diuretic/Ca2+ blocker, then ACE-I, then all 3, then b-blocker. |
|
|
What would be the effect on vascular smooth muscle tone of a drug which inhibits cGMP phosphodiesterase or reduces amounts of ROS?
|
Dilators. cGMP phosphodiesterase reduces levels of cGMP, so inhibiting this would raise cGMP. cGMP reduces levels of intracellular Ca2+. ROS bind NO rendering it inactive. So both these drugs would relax, one by raising NO and the other by lower free Ca2+.
|
|
|
How would a Ca2+ channel blocker affect autoregulation?
|
Blunt it. Autoregulation relies on Ca2+ channels
|
|
|
What causes increased flow to muscles in exercise?
|
Metabolites like NO.
|
|
|
How much do the atria contribute to ventricular filling at rest, and what are some of the important cardiac functions performed by them?
|
At rest the atria contribute 15-20% to ventricular filling - we could survive without this.
Important functions: SA node is located in the right atrium Veno-atrial receptors are important for signalling changes in blood volume to the brainstem. Stretch of the atria causes release of atrial natriuretic peptide (ANP) |
|
|
When might the atria become more important to overall cardiac function?
|
In exercise and when heart rate is high and there is less time for ventricular filling, the atria make a larger and more important contribution to ventricular filling.
Contraction of the atria may also assist ventricular filling if the latter is compromised (e.g. stiff ventricular wall). |
|
|
Which valves are open and which are closed in phase D of the cardiac cycle?
|
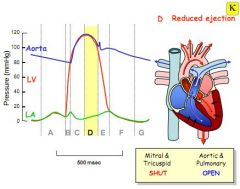
Reduced ejection. The force in the ventricles begins to drop as they empty, flow keeps valve open even when force is less than that in the artery. Aortic and pulmonary remain open, mitral and tricuspid are closed.
|
|
|
Which valves are open and which are closed in phase E of the cardiac cycle?
|
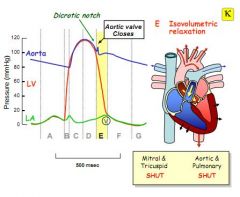
Isovolumetric relaxation. The pressure in the arteries finally forces the aortic and pulmonary valves shut - the aortic closure causing the dicrotic notch seen in phase E. The mitral and tricuspid are also closed.
|
|
|
Which valves are open and which are closed in phase F of the cardiac cycle?
|
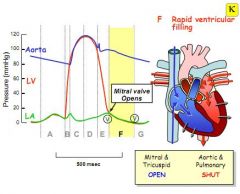
Rapid ventricular filling. The relaxation of phase E drops the pressure in the ventricles, and the mitral and tricuspid valves open to fill the ventricles. The aortic and pulmonary remain closed.
|
|
|
Which valves are open and which are closed in phase G of the cardiac cycle?
|
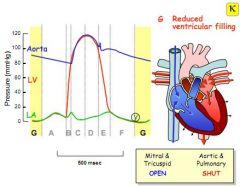
Reduced ventricular filling. As the ventricles fill the pressure between the atria and ventricles equalises and the rate of filling slows. Mitral and tricuspid open. Aorta and pulmonary closed.
|
|
|
What is the myogenic response in arterioles?
|
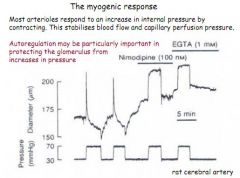
Arterioles respond to raised internal pressure by contracting (to stabilise blood flow and capillary perfusion pressure)
|
|
|
What is the probable cause of hypertension?
|
Deficiency in renal salt excretion, probably worsened by a high salt diet.
|

