![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
1. To list the distinguishing features of Types I, II, III & IV hypersensitivity. |
Type 1 -mast cell activation to soluble antigen |
|
|
What are the steps of type I hypersensitivity?
|
1) soluble antigen present in serum
2) APC binds antigen 3) APC presents antigen to TH2 cell 4) TH2 secretes IL-4 5) TH2 cell activates B cell 6) B Cell secretes IL 4 7) B cell secretes IgE 8) IgE binds Fcε receptor 9) mast cell degranulates |
|
|
What is the name of the IgE receptor?
|
FcεRI
|
|
|
How does IgE work at the FcεRI receptor?
|
via crosslinking of the repetitive epitopes on the FcεRI receptor
|
|
|
What are the main hypersensitivity mediators of the Type 1 response?
|
1) Tryptase, chymase, cathepsin G, carboxypeptidase
2) Histamine, Heparin 3) TNF-α 4) IL3&IL4 5) CCL 6) Leukotrienes, prostaglandins 7) platelet activating factor |
|
|
What is the difference between the IgE activation in mast cells in connective tissue vs mast cells in the mucosa?
|
mucosal mast cells: tryptase |
|
|
What does the tryptase and chymotryptase enzymes do?
|
remodel connective tissue matrix
|
|
|
What does histamine and heparin do? (3)
|
increase vascular permeability
cause smooth muscle contraction mucus production parasite toxicity |
|
|
What does Il-4 and IL-13 do in the Type 1 hypersensitivity response?
|
promote inflammation
stimulate cytokines production of many cell types activates endothelium |
|
|
What does IL-3 and IL-5 do?
|
stimulate and amplify TH2 resposne
|
|
|
What does the chemokine CCL3 do?
|
chemotaxis for monocyte, macrophages and neutrophils
|
|
|
What do leukotrienes do?
|
increase vascular permeability |
|
|
What does patlet activating facotr do?
|
activates cell mediators
chemotactic for leukocytes |
|
|
What enzyme produces histamine from what molecule?
|
histidine decarboxylase from histidine |
|
|
What are the functions of the prostaglandins and luekotrienes? (2)
|
blood vasodilation |
|
|
what stimulates eosinophils?
|
IL-5
|
|
|
What attracts eosinophils?
|
CCL11
|
|
|
What does MC and TH2 activation cause to happen to eosinophils?
|
accumulation of eosinophils at site
activation of FcεRI receptor on eosinophil |
|
|
What are the eosinophil mediators do?
|
trigger release of histamine from mast cells |
|
|
What is the importance of basophils in the type I allergic response?
|
initiate TH2/IgE by producing IL-4 and IL-13
|
|
|
What are the important characteristics of allergens? (7)
|
1) protein |
|
|
What cell provides the first burst of IL-4 that primes the B cells to make IgE?
|
basophils
|
|
|
What happens during the late phase vs immediate phase reaction?
|
Immediate: allergen-IgE induced MC degranulation |
|
|
What influences the severity of allargic symptoms?
|
site of mast cell activation
|
|
|
What happens when mast cells are degranualted in gastrointestinal tract?
|
diarrhea, vomiting
|
|
|
What happens when mast cells are degranulated in airway?
|
increased mucus |
|
|
What happens when mast cells are degranulated in blood vessels?
|
edema
inflammation |
|
|
What causes anaphylaxis?
|
antigen in blood stream enters tissue and activates mast cells throughout the body |
|
|
What occurs during allergic rhinitis?
|
allergen crosses mucus membrane
|
|
|
What happens in allergic asthma?
|
submucosa has MC that degranulate upon seeing antigen
|
|
|
What are ways to block Type I allergy? (5)
|
1) block histamine or leukotrienes
2) epinephrine 3) block IgE binding to MC via Xolair 4) allergen shots 5) desensitization |
|
|
What is the mechanism of type II hypersensitivity?
|
1) IgG or IgM is produced in response to exogenous or endogenous tissue that is modified
2) this leads to membrane attack complexes or ingestion by phagocytes |
|
|
What are the conditions associated with type II hypersensitivity? (5)
|
1) Good pastures (anti kidney and lung)
2)autoimmune hemolytic anemia 3) pemphigus vulgaris 4) myasthenia gravis 5) graves |
|
|
What happens in pemphigus vulgaris?
|
disrupt epidermis
|
|
|
What happens in Graves disease?
|
antibodies stimulate TSH receptor
|
|
|
What happens in myasthenia gravis?
|
antibodies block AcH signaling
|
|
|
What is type III hypersensitivity caused by?
|
immune complexes of IgG and soluble antigens circulating and can not be removed
|
|
|
What is the arthus reaction? (6)
|
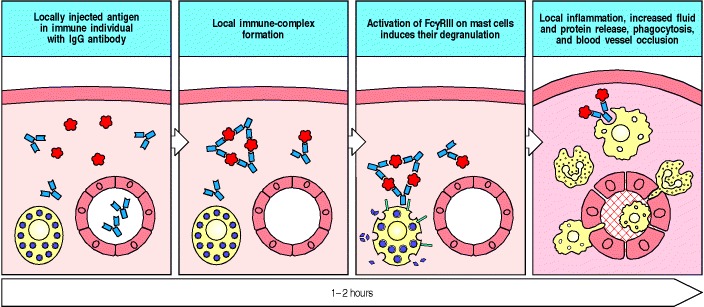
1) antigen gets complexed with IgG antibody
2) immune complex activates complement 3) c5a binds mast cell 4) immune complex binds to mast cell FcγRI 5) degranulation 6) inflammation and occlusion of blood vessel </img> |
|
|
What determines the pathology of Type III immune response?
|
where immune complex is deposited
|
|
|
What is the pathway for the type III immune response?
|
1) IgG/IgM bind soluble antigen
2) immune complex deposited on tissue 3) complement and neutrophils activated 4) pathology |
|
|
What are the conditions associated with type III immune response? (6)
|
1) SLE
2) GN 3) dermatitis 4) Arthritis 5) Retinitis 6) Vasculitis |
|
|
What is the mediator of type IV hypersensitivity?
|
antigen specific T effector cell
|
|
|
What are the 3 main types of Type IV hypersensitivity?
|
1) delayed type hypersensitivity
2) contact hypersensitivity 3) gluten sensitive enteropathy |
|
|
What is the antigen for delayed type insensitivity?
|
proteins such as insect venous, mycobacterial proteins
|
|
|
What is the consequence of delayed type hypersensitivity?
|
dermatitis
|
|
|
What is the mechanism for type IV hypersensitivity?
|
1) antigen processed by tissue macrophages
2) TH1 cells are stimulated 3a) chemokines are secreted to recruit macrophages 3b) INF-γ is secreted to activate macrophage and so they release their inflammatory mediators 3c) TNF-α and LT - local tissue destruction, increase blood adhesion 3d) IL-3/GM-CSF- monocyte production by bone stem cells |
|
|
What is type course of Type IV hypersensitivity?
|
24-72 hours
|
|
|
What is poison ivy an example of?
|
contact hypersensitivity
|
|
|
What causes celiac disease?
|
HLA-DQ2 or HLA-DQ8 MHC Class II
|
|
|
What are some common drugs that cause severe hypersensitivity?
|
1)carbamzepine
2) allopurinol 3) abacavir |
|
|
Why do some common drugs cause severe hypersensitivity?
|
class I association indicates CTL reactivity towards drugs with modified proteins
|

