![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
120 Cards in this Set
- Front
- Back
|
With regard to exanthems -- what is the "1st Disease"? Caused by what type of virus/bacteria?
|
Measles/Rubeola
- Paramyxovirus |
|
|
With regard to exanthems -- what is the "2nd Disease"? Caused by what type of virus/bacteria?
|
Scarlet Fever
GABHS |
|
|
With regard to exanthems -- what is the "3rd Disease"? Caused by what type of virus/bacteria?
|
German measles, Rubella
Togavirus |
|
|
With regard to exanthems -- what is the "4th Disease"? Caused by what type of virus/bacteria?
|
Dukes Disease
Not a distinct entity |
|
|
With regard to exanthems -- what is the "5th Disease"?
|
Erythema infectiosum
Parvovirus B19 |
|
|
With regard to exanthems -- what is the "6th Disease"?
|
Exanthem subitum, roseola infantum
HHV6, HHV7 |
|
|
Name the DNA viruses? Which one is the ssDNA virus?
|
DNA:
Herpes Hepadnavirus Adenovirus Papovavirus Parvovirus -- ssDNA Poxvirus |
|
|
Name the Herpesvirus group?
|
HSV
VZV CMV EBV |
|
|
Name the Hepadnavirus group
|
Hepatitis B
|
|
|
Examples of the Poxvirus?
|
Molluscum contagiosum
Smallpox ORF Milker's nodules |
|
|
Name the RNA viruses
|
Paramyxovirus (measles, mumps)
Togavirus (Rubella) Rhabdovirus (Rabies) Retrovirus (HIV, HTLV) Picornovirus (Enteroviruses, Coxsackie virus, Hand-Foot-and-Mouth Dz) |
|
|
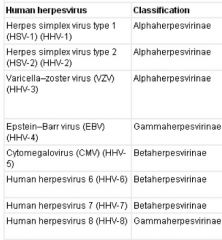
Of the Herpesvirus family, which ones are Alpha, Beta, and Gamma?
|
|
|
|
How is VZV transmitted? and, infectious period is?
|
Via respiratory droplets
INFECTIOUS PERIOD: Until at least 5 d after onset of rash Or until all lesions are dry, crusted |
|
|
Name the cause of this type of exanthem?
24-48 hours after prodrome “dewdrop on a rose petal” Centrifugal spread, starting on scalp, trunk, or face, and spreading to extremities Pathognomonic finding: lesions in various stages at the same time Most lesions have crusted over by day 6 Heal with hypopigmentation & scarring |
Varicella
|
|
|
What is Reye syndrome?
|
Associated with Varicella infection.
Reye syndrome is acute encephalopathy & fatty degeneration of viscera; almost always occurs w/ viral illness, unclear etiology Symptoms: decreased LOC, vomiting, abnormal LFT’s |
|
|
What is the most common complication of Varicella in kids?
|
#1 - Secondary bacterial superinfection
M/C S. aureus or GABHS more common in kids <5 #2: Neurologic involvement; Reye syndrome |
|
|
What is Varicella gangrenosa?
|
Varicella gangrenosa: rapidly progressing erythema, induration, and pain
|
|
|
What is the M/C serious complication in adults with Varicella?
|
Varicella pneumonia
- Can also get thrombocytopenia, arthritis, uveitis, nephritis, myocarditis, pancreatitis, hepatitis - Purpura fulminans, DIC |
|
|
Varicella vaccine is live or dead? When is it given?
|
- Live attenuated vaccine
- Routine vaccination at 12-18 months of age - Post-exposure prophylaxis - Immunocompromised children - Adults susceptible to varicella Effective in decreasing overall incidence: -- Milder disease w/ fewer lesions in vacinees w/ breakthrough -- High vaccine efficacy over 10 yrs for both groups receiving either 1 or 2 doses |
|
|
What type of virus is VZV?
|
Alphaherpesvirus (HHV-3)
|
|
|
What type of virus causes Rubeola?
|
Rubeola aka Measles
Caused by Paramyxovirus (ssRNA) |
|
|
What viral family is Mumps?
What viral family is rubella? |
Mumps - Paramyxovirus
Rubella - Togavirus |
|
|
Name the three C's of Rubeola?
|
Cough, Coryza, Conjunctivitis
|
|
|
What are Koplik spots?
|
Enanthem of Rubeola:
Koplik’s spots Punctate gray-white to erythematous papules on buccal mucosa Occur during prodromal period Grains of sand on a red background |
|
|
Describe the exanthem of Rubeola
|
- 2-4 dd after prodrome
- Begins on face (esp forehead), hairline, behind ears, spreads downward onto trunk & extremities - Erythematous to purple-red macules, papules; may become confluent - Fades in same order of appearance |
|
|
What is the delayed neurodegenerative disease associated with measles?
|
Subacute sclerosing panencephalitis:
- Characterized by seizures, personality changes, coma, death - Occurs in 1 in 100K pts w/ measles |
|
|
How is Rubeola transmitted?
|
Nasopharyngeal epithelium, to conjunctiva, to LN, to RES, to viremic state, to skin/liver/GI
|
|
|
How long should a person with rubeola stay in respiratory isolation?
|
from 4 days from the rash onset
|
|
|
What are some of the complications of Rubeola?
|
Pneumonia - Gastroenteritis
Bronchitis - Myocarditis Otitis - Encephalitis |
|
|
How do you treat Rubeola?
|
ribavirin (synthetic nucleoside analog) and Vitamin A supplementation
|
|
|
What type of virus is rubella?
|
Togavirus
|
|
|
How long is incubation of rubella?
|
14-23 days
|
|
|
How long is the prodrome for rubella
|
2-5 days prior the Exanthem
50% of pts are asymptomatic mild, self-limited disease is common |
|
|
Describe the exanthem of rubella?
|
Erythematous to “rose-pink” macules & papules, tend to become
confluent Most commonly involves the face and trunk Spreads in a cephalocaudad manner Involutes after 1-3 days in the same order it appeared Generalized lymphadenopathy often occurs -- Suboccipital, postauricular, and cervical regions -- Highly characteristic of Rubella but not pathognomonic. Arthralgias, arthritis, esp in females (52%) --- Fingers, wrists, knees |
|
|
What is the enanthem associated with Rubella?
|
Forscheimer's spots
|
|
|
What are the complications of rubella?
|
Encephalitis
Mycocarditis Hepatitis Pancytopenia, Hemolytic-uremic syndrome |
|
|
How long should a child be in isolation from rubella?
|
Contact isolation for 7 days following rash onset
|
|
|
What is the etiology of Scarlett Fever?
|
Bacterial exanthem caused by GABHS
Streptococcal pyogenic exotoxin shift from SPE-A to SPE-B, SPE-C --- ↓ morbidity, mortality |
|
|
Describe the tongue finding in scarlet fever?
|
Tonsillopharyngeal erythema, exudate, petechial macules of palate
White strawberry tongue in 1st few dd: white coating w/ red, edematous papillae projecting through Red strawberry tongue by 4th-5th day: red, glistening tongue w/ prominent papillae |
|
|
Do you have rhinorrhea with scarlet fever?
|
Usually absent rhinorrhea and cough; tender anterior cervical LAD
|
|
|
Describe the exanthem of scarlet fever
|
Fine, erythematous, macular and papular eruption: “sandpaper” or “gooseflesh”
Trunk, extremities Accentuation in flexural areas w/ petechial component: Pastia’s lines Circumoral pallor Generally resolves over 4-5 days May heal with desquamation (hands, feet, toes, fingers) |
|
|
Which disease has Pastia's lines?
|
Scarlet Fever
|
|
|
Which disease has Forscheimer spots?
|
Rubella
|
|
|
Name some complications of scarlet fever
|
Pneumonia, pericaridits, meningitis, hepatitis, glomeulonephritis, rheumatic fever
|
|
|
How do you prevent acute rheumatic fever?
|
Primary mode of prevention is to start abx (TOC Pen V or macrolides) within 9 days of symptoms
|
|
|
What is the etiology of Erythema Infectiosum?
|
Parvovirus B19
|
|
|
How long is the prodrome of Erythema Infectiosum?
|
Lasts 5-7 days, characterized by f/c, h/a; rash and arthralgias usually appear in the 3rd week of illness -- usu occuring time with IgG Ab appear.
|
|
|
Name five other diseases/clinical associations w/ parvovirus B19
|
Papular-purpuric gloves and socks syndrome
Petechial exanthems Transient aplastic crisis Fetal hydrops Arthritis |
|
|
Describe Stage 1 of Erythema Infectiosum
|
Stage I:
2-3 dd following prodrome Fiery-red facial erythema: “Slapped Cheeks”, spares nasal bridge & perioral areas |
|
|
Describe Stage II of Erythema Infectiosum
|
Lacy, reticulated eruption on extremities, trunk
1-4d after facial rash, fades over 2-3 wks May be pruritic, evanescent Spares palms/soles |
|
|
Describe Stage III of Erythema Infectiousum
|
Intermittent waxing/waning of lacy, reticular eruption in response to environmental stimuli: physical activity, warm temperatures, sunlight
Variable length, usually 1-3 weeks |
|
|
What percent of patients with ill joint symptoms following Erythema Infectiousum?
|
8-10% of kids, 60% of adults (esp females)
MCP, PIP, knees, wrists, ankles |
|
|
What is the risk of getting B19 infection if you have an underlying RBC production disorder?
|
Transient aplastic crises in pts w/ d/o of ↓ RBC production or ↑ RBC destruction
B19 has high affinity for erythroid precursors, binding to? P antigen (globoside) receptor |
|
|
What receptor does B19 target on erythroid precursors?
|
Transient aplastic crises in pts w/ d/o of ↓ RBC production or ↑ RBC destruction
B19 has high affinity for erythroid precursors, binding to? P antigen (globoside) receptor |
|
|
Can B19 cross the placenta
|
Yes
|
|
|
What can B19 do to a fetus?
|
- Anemia
- High output CHF - Hydrops fetalis Generalized edema w/ ascites, pleural effusions, polyhydramnios - Intrauterine fetal demise |
|
|
What is the greatest risk to the fetus from a B19 infection?
|
1st 20 wks of pregnancy
|
|
|
B19 can cause an erythematous, petechial patch and plaques on the palms and soles, normal mucosal exam, no LAD -- aka?
|
Papular purpuric gloves and socks syndrome
|
|
|
Identify:
Acute onset of rapidly progressive, symmetric swelling & erythema of the hands, feet Often w/ petechial or purpuric component Sharp dermarcation at the wrists, ankles Usually very pruritic |
Papular purpuric gloves and socks syndrome
|
|
|
When pts have the exanthem in gloves and socks syndrome, are they infectious?
|
Yes (C2 EI)
|
|
|
What is the enanthem in gloves and socks syndrome?
|
Hyperemia, petechiae, erosions on the soft and hard palate, pharynx, tongue, inner lips
|
|
|
What is 6th disease also known as?
|
Roseola infantum, aka Exanthem subitum
|
|
|
What causes roseola infantum?
|
HHV 6 and HHV7:
-- Preferentially infect activated T cells -- Majority of childhood infections: HHV-6A -- More frequent in immunocompromised hosts: HHV-6B |
|
|
How is roseola infantum transmitted?
|
Via Saliva
Horizontal transmission |
|
|
What is classic presentation of Roseola Infantum?
|
High fever (101-106) for 3-5 dd
Exanthem when temp normalizes Mild illness in children < 3 yo |
|
|
What is the Berliner's sign?
|
Periorbital edema that causes child to look sleepy, seen in roseola infantum.
|
|
|
Describe the exanthem in roseola infantum.
|
Nondescript, erythematous blanchable macules & papules
Peripheral halo of vasoconstriction Appears initially on the trunk, spreads to extremities, neck, face Resolves over 1-3 dd Periorbital edema is common clue to dx in febrile but o/w well appearing child prior to the exanthem Sleepy look caused by palpebral & periorbital edema? Berliner’s sign |
|
|
What is the enanthem in roseola infantum?
|
Nagayama's spots;
Erythematous papules involving mucosa of the soft palate and uvula (2/3) |
|
|
In solid organ and BMT recipients, reactivation of roseola infantum may mimic what disease?
|
may mimic acute GvHD
|
|
|
Name some common causes of exanthems in children
|
Nonpolio enteroviruses (summer months)
Respiratory viruses (winter months) Adenovirus Rhinovirus Parainfluenza virus Respiratory synccytial virus Influenza virus EBV HHV-6,7 Parvovirus B19 |
|
|
What is another name for Papular Acrodermatitis of Childhood
|
Gianotti-Crosti syndrome
|
|
|
What causes Gianottic-Crosti?
|
- distinct viral exanthem that may occur after infection with any of several viral agents
EBV (MCC in US) HBV (Italy, Japan) |
|
|
Describe the exanthem in Gianottic-Crosti
|
Edematous, erythematous, monomorphous papules & occasionally papulovesicles
Distributed symmetrically over the face and extensor surfaces of UE/LE Usually spares the trunk -- Buttocks may be involved Hemorhagic changes or localized purpura may be present Usually asymptomatic, may be pruritic May take 8-12 wks to resolve |
|
|
Unilateral Laterothoracic Exanthem is aka?
|
Asymmetric periflexural exanthem of childhood
|
|
|
Describe the exanthem of Unilateral Laterothoracic exanthem
|
EXANTHEM:
- Onset is unilateral on the trunk - Extends toward axilla & less often around inguinal region or an extremity - Centrifugal spread - Often becomes bilateral --- Maintains predominance on initial side of presentation Various morphologies: Macules, papules, eczematous, mobilliform, scarlatiniform, annular, reticulate Pruritus in 50% |
|
|
What is a unique finding on unilateral laterothoracic exanthem biopsy?
|
lymphocytic infiltrate around dermal eccrine ducts
|
|
|
Enterovirus are part of what virus family?
|
Picornavirus (ssRNA);
Includes: Echovirus Poliovirus Enterovirus Coxsackie virus A&B |
|
|
What are some associated disease with enteroviruses?
|
HFMD - Gianotti-Crosti
Herpangina - Non-Specific Aseptic meningitis - HSP Still’s like disease - AGEP |
|
|
What is the leading cause of viral meningitis?
|
Nonpolio enteroviruses are leading cause of viral meningitis
|
|
|
Name the disease:
EXANTHEM: Gray-white vesicular lesions on palms, soles, less often involving dorsal or lateral srfaces of hands/feet Associated w/ fever, malaise, occ cervical & submandibular LAD |
Hand Foot Mouth Disease
|
|
|
Name the disease:
ENANTHEM: Painful vesicles, erosions of buccal surfaces, palate, tongue, uvula, gingivae, anterior tonsillar pillars Can lead to anorexia, dehydration |
Hand Foot Mouth Disease
|
|
|
Which serotype has been implicated in more severe disease and even death in HFMD epidemics in Taiwan?
|
Enterovirus 71
More severe disease in children < 5 Majority of deaths from pulmonary edema or pulmonary hemorrhage |
|
|
Herpangina is caused by what virus?
|
Coxsackie A & B
|
|
|
Name the disease:
- Children ages 3-10 - F, sore throat, malaise - Gray-white vesicles, erythematous erosions involving palate, uvula, tonsillar pillars |
Herpangina
|
|
|
Which Echovirus can mimic zoster?
|
Echovirus 6 can mimic zoster with a vesicular eruption that is dermatomal
|
|
|
Which Echovirus can mimic meningococcemia?
|
Echovirus 9: aseptic meningitic, petechial rash similar to meningitis
|
|
|
Which echovirus mimics roseola?
|
Echovirus 16
|
|
|
What is eruptive pseudoangiomatosis?
|
Acute onset of hemangioma-like lesions
-- Angiomatous papules surrounded by rim of blanching Spontaneous resolution 2-6 dd F, malaise, HA, diarrhea, respiratory complaints |
|
|
What causes Mono?
|
Epstein Barr Virus
|
|
|
What type of virus is EBV?
|
Epstein Barr Virus is a DNA herpesvirus family; Tropism for lymphocytes (B-cells) and epithelial cells
|
|
|
What % of patients with infectious mononucleosis will develop a rash following the administration of ampicillin or amoxicillin?
|
90-95% of pts develop an erythematous macular & papular eruption
May be related to ampicillin-antibody immune complexes resulting from B cell activation Occurs 5-9 dd after starting antibiotic Does not represent a true allergy |
|
|
How do you dx Mono in the lab?
|
Heterophil Ab: most useful confirmatory test (high specificity)
Virus-specific serologies for: kids <4 (often heterophile antibody negative), atypical presentations, severe or prolonged disease |
|
|
What are the four genus groups of Rickettsial Disease?
|
Bartonella
Coxiella Ehrlichia Rickettsia |
|
|
What organism causes bacillary angiomatosis?
|
Bartonella henselae
Bartonella quintana |
|
|
What organism causes trench fever? transmitted by?
|
B. quintana
transmitted by Human body louse |
|
|
What organism causes Qfever? transmitted by?
|
Coxiella Burnetii -- by ticks
|
|
|
What organism causes Human monocytic ehrlichiosis? human granulocytic ehrlichiosis? vector?
|
Ehrlichia chaffeensis -- HME -- lone start tick
Anaplasma phagocytophilum -- human granulocytic ehrlichiosis -- deer tick, dog tick |
|
|
What organism causes rickettsialpox?
|
Rickettsia akari; transmitted by house mouse mite
|
|
|
What does rickettsia conorii cause? transmitted by?
|
Mediterranean spotted fever -- Dog ticks
|
|
|
What organism causes epidemic typhus? Endemic typhus?
|
Epidemic = Rickettsia prowazekii
-- transmitted by the human body louse Endemic = Rickettsia typhi -- transmitted by the rat flea |
|
|
What organism causes Rocky Mountain spotted fever?
|
Rickettsia rickettsii -- wood tick and dog tick
|
|
|
What is another name for murine typhus?
|
Endemic Typhus
|
|
|
Who transmits endemic typhus?
|
Rat Flea, Xenopsylla cheopsis -- organism is Rickettsia typhi
|
|
|
What is the treatment(s) of choice for endemic typhus?
|
Tetracycline or Chloramphenicol
|
|
|
Who transmits rickettsia akari? and, what disease does it cause?
|
House mouse mite, Liponyssoides sanguineus
- Caused by Rickettsialpox |
|
|
What is the triad of Rickettsialpox?
|
Classic triad:
Fever Eschar Rash (numerous monomorphous red papules with small central vesicular component) -- usu black eschar at site. |
|
|
How do you treat rickettsialpox?
|
Doxy or chloramphenicol
|
|
|
What is the most common ricketsial disease in the U.S.?
|
M/C is rickettsia rickettsii -- RMSF
|
|
|
What is the epidemiology of RMSF?
|
Most common rickettsial illness in the US
Highest incidence in kids ages 5-9 North Carolina and Virginia – highly endemic Among children living in southeastern & southern US, 12% had positive R. rickettsii antibody titers Throughout US – except Maine and Vermont |
|
|
Name the vector for RMSF
|
Western US, Canada:
Dermacentor andersoni (wood tick) Eastern US: Dermacentor variabilis (dog tick) |
|
|
What % of RMSF pts do NOT recall a tick bite?
|
40%
|
|
|
Describe the exanthem of RMSF?
|
Appears on day 3-5 of illness
Discrete, erythematous, blanching macules, papules - Spread centripetally (start on extremities, spread centrally) - Initially on ankles, wrists, palms, soles Evolve into petechial macules, papules - May become hemorrhagic, +/- focal necrosis |
|
|
How do you diagnosis RMSF?
|
Indirect fluorescent antibody (IFA) test is most widely used diagnostic examination
- Detects anti-R.rickettsi IgM and IgG - usually present 10 to 14 days following acute infection |
|
|
TOC for RMSF?
|
Doxy!!
Risk of dental staining in kids < 8 yo, is far outweighed by risk of RMSF; unlikely to occur with short courses. Chloramphenicol (use in pregnant pts) |
|
|
Cause of Qfever
|
Coxiella burnetti
|
|
|
How is Qfever transmitted
|
Contact w/ infected domestic animals (cattle, sheep, goats)
Inhalation of contaminated aerosols |
|
|
Tx for Q-Fever
|
Doxy, FQs, or Co-trimoxazole
|
|
|
Cause and vector of Human monocytic ehrlichiosis?
|
Caused by: Ehrlichia chaffeensis
Vector: Lone star tick (amblyomma americanum) |
|
|
Cause and vector of Human granulocytic ehrlichiosis?
|
Caused by: Anaplasma phagocytophilum
Vector: Ixodes scapularis (NE & upper midwestern U.S.), Ixodes pacificus (west coast) |
|
|
TOC for ehrlichiosis?
|
Doxy
|

