![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
108 Cards in this Set
- Front
- Back
|
What amount is a typical range of cells is typical for a human body?
|
50 to 100 trillion cells
|
|
|
What are the 3 main regions of a cell?
|
1- Plasma membrane
2- Cytoplasm 3- Nucleus |
|
|
What is a plasma membrane (plasmalemma)?
|
It's the outer thin and flexible membrane of the cell which separates the intracellular from the extracellular environment.
|
|
|
What molecules are typically part of the plasma membrane?
|
Phosopholipids, cholesterol, and glycolipids, within which proteins are embedded.
|
|
|
What are phospholipids and what are the 2 main parts of them?
|
Phospholipids are the most abundant lipids in the plasma membrane.
Consist: The Heads which are hydrophilic, and lie on the inner and outer face of the membrane. The tails are hydrophobic and line up in the center |
|
|
Define:
Integral Proteins Peripheral Proteins |
Integral proteins:
-most abundant -usually extend through the entire membrane or protrude through one end of the membrane -Often act as receptors Peripheral proteins -Mainly on the cytoplasmic side -Support cytoplasm through network of filaments Glycocalyx -a carbohydrate that is projected out from the external surface of glcyoproteins and glycolipids -Functions in cell-to-cell binding and recognition |
|
|
What are 3 functions of the plasma membrane?
|
1. Serves as an external cell barrier against substances and forces outside the cell.
2. Externally facing proteins act as receptors (for hormones, neurotransmitters, etc) 3. Acts in transport of substances into or out of the cell (semi-permeable membrane). |
|
|
Define:
diffusion Active transport Vesicular or bulk transport |
Diffusion: movement of small, uncharged, molecules across the membrane. Examples: Oxygen, CO2, and fat soluble molecules.
Active transport: most larger water-soluble or charged molecules. Examples: Glucose, amino acids, and ions. Uses facilitated diffusion or pumps. Involves integral proteins. Vesicular or bulk transport: Macromolecules pass through the membrane this way. 2 types: exocytosis and endocystosis. |
|
|
define:
exocytosis endocytosis |
Endocytosis is an energy-using process by which cells absorb molecules (such as proteins) by engulfing them. It is used by all cells of the body because most substances important to them are large polar molecules that cannot pass through the hydrophobic plasma or cell membrane.
e.g.: mucus and protein secretions from the glands in the body. Exocytosis: is the durable, energy-consuming process by which a cell directs the contents of secretory vesicles out of the cell membrane and into the extracellular space. |
|
|
define the 3 types of endocytosis
phagocytosis pinocytosis Receptor-mediated Endocytosis |
Phagocytosis: This is when white blood cells engulf bacteria and it creates a space called a phagosome which fuses with a lysozome where the bacteria are broken up by enzymes.
Pinocytosis: When the cell takes in fluid by small folding surrounds a small quantity of fluid outside the cell. Common in intestines to absorb nutrients Receptor-mediated Endocytosis: After the binding of a ligand to plasma membrane-spanning receptors, a signal is sent through the membrane, leading to membrane coating, and formation of a membrane invagination. The receptor and its ligand are then opsonized in clathrin-coated vesicles. Once opsonized, the clathrin-coated vesicle uncoats (a pre-requisite for the vesicle to fuse with other membranes) and individual vesicles fuse to form the early endosome. Since the receptor is internalized with the ligand, the system is saturable and uptake will decline until receptors are recycled to the surface. |
|
|
Define:
Familial hypercholesterolemia |
Is an inherited disease in which the cells lack the receptors that bind to cholesterol binding LDLs.
As a result, cholesterol cannot enter the cells and builds up in the blood, causing hypercholesterolemia and atherosclerosis which lead to stroke or myocardial infarction. |
|
|
Define:
Cytoplasm |
Cytoplasm: is the cellular region between the nucleus and plasma membrane.
Consists of the cytosol or cytoplasmic matrix: the aqueous component of the cytoplasm of a cell, within which various organelles and particles are suspended. |
|
|
Define:
Ribosomes |
Ribosome: a minute particle consisting of RNA and associated proteins, found in large numbers in the cytoplasm of living cells. They bind messenger RNA and transfer RNA to synthesize polypeptides and proteins.
|
|
|
Rough endoplasmic reticulum (rER):
|
The outer (cytosolic) face of the rough endoplasmic reticulum is studded with ribosomes that are the sites of protein synthesis. Rough endoplasmic reticulum is especially prominent in cells such as hepatocytes where active protein synthesis occurs.
|
|
|
What is the nucleus of a cell and what the 3 main parts of it?
|
-Nucleus is the main control center of the cell and contains the genetic material (DNA). DNA directs the cells activities by providing the instructions for protein synthesis.
Parts: 1. Nuclear envelope 2. Chromatin and chromosomes 3. Nucleoli |
|
|
What is the nucleolus?
|
The nucleolus is a structure found in the nucleus of cells. It forms around specific chromosomal regions in the nucleus of eukaryotic cells, and is made up of proteins and ribonucleic acids. Its function is to transcribe ribosomal RNA (rRNA) and combine it with proteins to form incomplete ribosomes.
|
|
|
What is chromatin?
|
Chromatin is how DNA exists in eukaryotic cells. They condense and shrink into chromosomes during Prophase of mitosis and meiosis.
|
|
|
What happens in G1 phase?
|
cells are active and grow vigorously and
centrioles start to replicate. |
|
|
What happens in G2 phase?
|
Enzymes needed for cell division are
synthesized, centrioles finish replication and cell gets ready to divide. |
|
|
What happens in S phase?
|
DNA replicates itself for the future two
daughter cells having identical genetic material |
|
|
What happens in prophase of mitosis?
|
-Histones condense chromatin into chromosomes
-Centrioles move to polar ends of the cell -Spindle fibers form -The Nuclear envelope disintegrates -Nucleoli disappears |
|
|
What happens in metaphase of mitosis?
|
-Chromosomes cluster at the middle of the cell, to form a metaphase plate
-Seperase cleaves cohesin to start seperating the chromatids |
|
|
What happens in anaphase of mitosis?
|
-The chromatids are pulled apart at their kinetochores by the spindle fibers.
|
|
|
What happens in telophase of mitosis?
|
-The chromosomes are pulled to opposite ends of the cell.
-A cleavage furrow develops and the cell elongates in preparation for cytokinesis. -The chromsomes uncoil into chromatin -The nuclear envelope reforms -nucleoli appear |
|
|
What is cytokinesis:
|
When the cell is divided
|
|
|
What is down syndrome?
|
Trisomy 21
Is a genetic disorder caused by the presence of all or part of a third copy of chromosome 21. It is typically associated with physical growth delays, a particular set of facial characteristics and a severe degree of intellectual disability. The average full-scale IQ of young adults with Down syndrome is around 50 (70 and below is defined as the cut-off for intellectual disability), whereas young adult controls have an average IQ of 100. |
|
|
What is Klinefelter's syndrome?
|
Results from an additional X chromosome in males. (XXY)
Principal effects include hypogonadism and sterility. A variety of other physical and behavioural differences and problems are common, though severity varies and many XXY boys have few detectable symptoms. The only reliable method of diagnosis is karyotype testing. The degree to which XXY males are affected, both physically and developmentally, differs widely from person to person. |
|
|
Turner syndrome
|
(XO)...
absence of the other X chromosome (Monosomy X) Encompasses several conditions in human females, of which monosomy X (absence of an entire sex chromosome, the Barr body) is most common. It is a chromosomal abnormality in which all or part of one of the sex chromosomes is absent or has other abnormalities (unaffected humans have 46 chromosomes, of which two are sex chromosomes). In some cases, the chromosome is missing in some cells but not others, a condition referred to as mosaicism. There are characteristic physical abnormalities which affect many but not all people with Turner syndrome, such as short stature, swelling, broad chest, low hairline, low-set ears, and webbed necks. Girls with Turner syndrome typically experience gonadal dysfunction (non-working ovaries), which results in amenorrhea (absence of menstrual cycle) and sterility. Concurrent health concerns may also be present, including congenital heart disease, hypothyroidism (reduced hormone secretion by the thyroid), diabetes, vision problems, hearing concerns, and many autoimmune diseases. Finally, a specific pattern of cognitive deficits is often observed, with particular difficulties in visuospatial, mathematical, and memory areas. |
|
|
Define:
Aging Mitochondrial theory of aging Genetic theories of aging |
Aging: is complex and may involve cell damage due to free radicals as a result of normal cell metabolism or cell injury due to radiation and chemical pollutants.
Mitochondrial theory of aging: involves a decrease of energy production by radical-damaged mitochondria which weakens and ages the cell. Vitamins C and E act as antioxidants and prevent excessive production of free radicals. The same is true with caloric intake restriction due to lowering the metabolic rate which slows aging. Genetic Theories of Aging: proposes that aging is programmed into our genes (senescence). |
|
|
What is a
Neoplasm Benign Neoplasm malignant neoplasm or cancer |
A cell mass which divides and multiplies abnormally; it is also called a neoplasm.
Neoplasms are classified as Benign or Malignant. Benign neoplasm or tumor is a local mass, remains compacted, often encapsulated, grows slowly and seldom kills the host. Malignant neoplasm or cancer is a mass which is not-capsulated and grows rapidly. Cells here are immature and they invade their surrounding. These give metastasis (invading other tissues) by means of lymphatics and/or blood |
|
|
What are
Oncogenes? |
Oncogenes are the result of mutations of certain regulatory genes, called protooncogenes, which normally stimulate or inhibit cell proliferation and development.
Genetic accidents or viruses may lead to the formation of oncogenes. Oncogenes dominate the normal alleles (proto-oncogenes), causing deregulation of cell division, which leads to a cancerous state. Bladder cancer and acute myelogenous leukemia are caused by occogenes. |
|
|
What are the 4 types of tissue?
|
Muscle, Nervous, Epithelial, and connective tissues
|
|
|
What are the 3 types of muscle tissue and what are their main functions?
|
Skeletal muscle:
a type of striated muscle, usually attached to the skeleton. Skeletal muscles are used to create movement, by applying force to bones and joints; via contraction Smooth muscle: Smooth muscle is found within the walls of organs and structures such as the esophagus, stomach, intestines, bronchi, uterus, urethra, bladder, and blood vessels, and unlike skeletal muscle, smooth muscle is not under conscious control. Cardiac muscle: is also an "involuntary muscle" but is a specialized kind of muscle found only within the heart. |
|
|
What is nervous tissue specialized to?
|
Nervous tissue is specialized to:
react to stimuli and to conduct impulses to various organs in the body which bring about response to the stimulus. |
|
|
What type of cells is nerve tissue composed of mainly?
|
Neurons, which are found in the spinal cord, peripheral nerves, that branch throughout the body.
|
|
|
Are neurons easily stimulated and do they transmit impulses very rapidly?
|
Yes
|
|
|
Define:
Epineurium Perineurium Endoneurium |
Epineurium : A sheath of dense connective tissue, that surrounds the nerve.
Perineurium: the sheath of connective tissue surrounding a bundle (fascicle) of nerve fibers within a nerve. Endoneurium: which consists of a thin layer of loose connective tissue, surrounds the individual nerve fibers. |
|
|
What the 8 main functions of the Epithelial tissue?
|
1. Protection: Epithelial cells from the skin protect underlying tissue from mechanical injury, harmful chemicals, invading bacteria and from excessive loss of water.
2. Sensation Sensory stimuli: penetrate specialized epithelial cells. Specialized epithelial tissue containing sensory nerve endings is found in the skin, eyes, ears, nose and on the tongue. 3. Secretion In glands:, epithelial tissue is specialized to secrete specific chemical substances such as enzymes, hormones. 4. Absorption: Certain epithelial cells lining the small intestine absorb nutrients from the digestion of food. 5.Excretion: Epithelial tissues in the kidney excrete waste products from the body and reabsorb needed materials from the urine. Sweat is also excreted from the body by epithelial cells in the sweat glands. 6. Diffusion: Simple epithelium promotes the diffusion of gases, liquids and nutrients. Because they form such a thin lining, they are ideal for the diffusion of gases (eg. walls of capillaries and lungs). 7. Cleaning: Ciliated epithelium assists in removing dust particles and foreign bodies which have entered the air passages. 8. Reduces Friction: The smooth, tightly-interlocking, epithelial cells that line the entire circulatory system reduce friction between the blood and the walls of the blood vessels. |
|
|
What are epithelial tissue and glands?
|
Epithelial are sheets of cells that cover body surfaces and cavities.
Their function is to protect the body (such as the skin) or sensory reception such as the olfactory epithelial cells, absorption, such as the internal covering cells of the intestine, ion transport and filtration, like the cells covering various tubules in the kidney. Glands are also covered internally by epithelial cells which function in secretion of their products. |
|
|
What are the 3 shapes (classifications) of epithelial cells?
|
1- Squamous (flat)
2- Cuboidal (cube like) 3- Columnar (tall and rod-like) |
|
|
Define:
Simple Stratified |
Simple: one layer
Stratified: more than one layer |
|
|
What is a squamous cell?
|
an epithelial cell that is flat like a plate and form a single layer of epithelial tissue
The surface squamous cells are irregularly shaped and very flat; so flat that the cell nucleus sometimes creates a bump in the surface of the cell. Gases and other substances can easily diffuse across squamous cells to the underlying basement membrane, and because of their smooth surface, liquids can quickly flow over them. As such, simple squamous epithelia are seen lining body cavities and capillaries to reduce friction, as well as lining the alveoli to facilitate gas exchange. |
|
|
What two ways are glands classified?
|
Glands of the body are classified as either exocrine or endocrine types.
|
|
|
Define:
Endocrine Glands Exocrine Glands |
*An Exocrine gland is distinguished by the fact that it excretes its essential product by way of a duct to some environment external to itself, be it either inside the body or on a surface of the body.
Examples of exocrine glands include the sweat glands, salivary glands, mammary glands, and liver. *Endocrine gland is its counterpart. It secretes its essential product (hormones) without the use of a duct directly into the bloodstream or else by diffusion into its surrounding tissue (paracrine signaling) where it often affects only target cells near the release site. Examples of endocrine glands include the adrenal glands, located atop the kidneys and responsible for the secretion of certain hormones such as adrenaline, cortisol and others. The testes, in males and ovaries in females are not only gonads, organs which generate male and female germ cells respectively, but are also endocrine glands in that they produce various androgens and estrogens together known as steroidal sex hormones. |
|
|
Exocrine Glands release their products into ducts in three different ways...Define them:
1- merocrine 2-apocrine 3-holocrine |

1. Merocrine: The most common method. A cell is classified as merocrine if the secretions of that cell are excreted via exocytosis (contents released from cell) from secretory cells into an epithelial-walled duct or ducts and thence onto a bodily surface or into the lumen.
2. Apocrine: the apical portions of cells are pinched off and lost during the secretory process. This results in a secretory product that contains a variety of molecular components including those of the membrane. Mammary glands release their products in this manner. 3. holocrine: The third type of secretory release, holocrine, involves death of the cell. The secretory cell is released and as it breaks apart, the contents of the cell become the secretory product. This mode of secretion results in the most complex secretory product. Some sweat glands located in the axillae, pubic areas, and around the areoli of the breasts release their products in this manner. Sebaceous glands also are of this type. |
|
|
There are 3 factors that hold epithelial cells together:
|
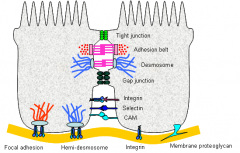
1. Adhesion
2. Contours of adjacent cell membranes 3. Special cell junctions Which include: -Tight junctions -Adhering junctions -desmosomes -gap junctions |
|
|
What are Tight junctions (zona occludens)?
|
Go back to Tissues slide 26ish
|
|
|
What is Ehlers-Danlos Syndrome?
|
Ehlers–Danlos syndrome (EDS) is an inherited connective tissue disorder with different presentations that have been classified into several primary types. EDS is caused by a defect in the structure, production, or processing of collagen or proteins that interact with collagen. (1 and 3)
The collagen in connective tissue helps tissues resist deformation. Collagen is an important contributor to the physical strength of skin, joints, muscles, ligaments, blood vessels and visceral organs; abnormal collagen renders these structures more elastic. Depending on the individual, the severity of the mutation can vary from mild to life-threatening. There is no cure, and treatment is supportive, including close monitoring of the digestive, excretory and particularly the cardiovascular systems. |
|
|
What are integrins?
|
Integrins are transmembrane receptors that mediate the attachment between a cell and its surroundings, such as other cells or the extracellular matrix (ECM). In signal transduction, integrins pass information about the chemical composition and mechanical status of the ECM into the cell. Therefore, in addition to transmitting mechanical forces across otherwise vulnerable membranes, they are involved in cell signaling and the regulation of cell cycle, shape, and motility.
Typically, receptors inform a cell of the molecules in its environment and the cell responds. Not only do integrins perform this outside-in signaling, but they also operate an inside-out mode. Thus, they transduce information from the ECM to the cell as well as reveal the status of the cell to the outside, allowing rapid and flexible responses to changes in the environment, for example to allow blood coagulation by platelets. There are many types of integrin, and many cells have multiple types on their surface. Integrins are of vital importance to all animals and have been found in all animals investigated, from sponges to mammals. Integrins have been extensively studied in humans. Integrins work alongside other proteins such as cadherins, immunoglobulin superfamily cell adhesion molecules, selectins and syndecans to mediate cell–cell and cell–matrix interaction and communication. Integrins bind cell surface and ECM components such as fibronectin, vitronectin, collagen, and laminin. |
|
|
What is the extra cellular matrix (ECM)?
|
In biology, the extracellular matrix (ECM) is the extracellular part of multicellular structure (e.g., organisms, tissues, biofilms) that typically provides structural and biochemical support to the surrounding cells.
Because multicellularity evolved independently in different multicellular lineages, the composition of ECM varies between multicellular structures; however, cell adhesion, cell-to-cell communication and differentiation are common functions of the ECM. The animal extracellular matrix includes the interstitial matrix and the basement membrane. |
|
|
What are 2 categories of Carrier-mediated transport?
|
a. facilitated diffusion
b. active transport |
|
|
What types of molecules are capable of diffusing through the phospholipid bilayer passively?
|
Small molecules, such ions, (iodine)...lipid-soluble molecules (fat soluble that dissolve in the lipid portion of the bilayer...remember like-dissolves like...so hydrophobic molecules dissolve hydrophobic molecules). and water (osmosis).
Lipid soluble substances can enter a cell by dissolving in the lipid portion of the membrane and diffusing through it. The greater the lipid solubility, the more readily a molecule will pass through the membrane, i.e., the greater will be the flux for a given concentration difference Water soluble, lipid-insoluble substances by definition cannot pass through membranes by dissolving in the lipids. How do they get through? There must be water-filled channels or pores spanning the membrane through which these substances may diffuse. LIPIDS Each lipid molecule has a polar head and two non-polar tails. The polarity in the head results from the molecular interaction between the oppositely charged phosphate and nitrogen groups. The resulting dipole makes this part of of the molecule polar and, therefore, water soluble. It is called the hydrophilic, or water-loving, portion of the lipid molecule. In contrast, the two tails of each lipid molecule are non-polar and water insoluble. They are composed of long-chain fatty acids which are hydrophobic, or water-hating, in nature. The tails are joined to a backbone molecule which, in turn, is attached to the polar head. Because they each contain a hydrophilic and hydrophobic end, lipid molecules naturally form a bilayered membrane. The polar, water-soluble heads point toward the water on the inside and outside of the cell, while the non-polar, fatty-acid tails point away from water and toward the membrane interior. The resulting bilayer of lipid molecules contains an oily inner core, It functions as a selective barrier permeable to lipid-soluble substances and impermeable to polar, water-soluble substances. |
|
|
What is passive transport and in which direction is the concentration gradient?
|
It is the net movement of molecules and ions across a membrane from higher to lower concentration, it does not require metabolic energy. Passive transport includes simple diffusion, osmosis, and facilitated diffusion
|
|
|
What is active transport?
|
Active transport is net movement across a membrane that occurs against a concentration gradient (to the region of higher concentration). Active transport requires metabolic energy (ATP) and involves specific carrier proteins.
|
|
|
What factors increase permeability in simple diffusion?
|
a. smaller molecules increases rate of diffusion
b. smaller membrane thickness c. high oil/water partition coefficient of the solute increases solubility in the lipid of the membrane. |
|
|
What molecules have the highest permeabilities in lipid membranes?
|
Small hydrophobic solutes have the highest permeabilities in lipid membranes.
|
|
|
How do hydrophilic substances cross the cell membrane?
|
Hydrophilic solutes must cross cell membranes through water-filled channels, or pores. If the solute is an ion, then its flux will depend on both the concentration difference and the potential difference across the membrane.
This is because the lipid bilayer is composed of fatty acid tails which are not water soluble (think oil and vinegar) |
|
|
How is stereospecificity important in Carrier-mediated transport?
|
For example, D-glucose (the natural isomer) is transported by facilitated diffusion, but the L-glucose isomer is not. Simple diffusion, however, would not distinguish between the two isomers because it does not involve a carrier.
When it comes to protein molecules, structure and function go hand in hand. So, proteins are very highly picky about what molecules they will transport. |
|
|
How is saturation important in Carrier-mediated transport?
|
The transport rate increases as the concentration of the solute increases, until the carriers are saturated. (Collision theory?)
The transport maximum (™) is analogous to the maximum velocity (V max) in enzyme kinetics. |
|
|
What are some characteristics of facilitated diffusion? [TRANSMEMBRANE PROTEIN CHANNELS]
|
Not to be confused with diffusion. Facilitated diffusion is not a type of diffusion (thermal motion) but a type of transport process.
Facilitated diffusion (also known as facilitated transport or passive-mediated transport) is the process of spontaneous passive transport (as opposed to active transport) of molecules or ions across a biological membrane via specific transmembrane integral proteins. Being passive, facilitated transport does not involve the use of chemical energy; rather, molecules and ions move down their concentration gradient. Facilitated diffusion is not a form of diffusion, however it is a transport process in which molecules or ions which would otherwise cross the membrane with great difficulty exploit transmembrane protein channels to help them cross this membrane. Polar molecules and charged ions dissolved in water cannot diffuse freely across the plasma membrane due to the hydrophobic nature of the fatty acid tails of phospholipids that make up the lipid bilayers. Only small non-polar molecules, such as oxygen can diffuse easily across the membrane. Hence, all polar molecules are transported across membranes by proteins that form transmembrane channels. These channels are gated, enabling them to open and close and thus regulating the flow of ions or small polar molecules. Larger molecules are transported by transmembrane carrier proteins, such as permeases that change their conformation as the molecules are carried through, for example glucose or amino acids. Non-Polar molecules, such as retinol or lipids are poorly soluble in water. They are transported through aqueous compartments of cells or through extracellular space by water-soluble carriers as retinol binding protein Glucose, sodium ions and chloride ions are just a few examples of molecules and ions that must efficiently cross the plasma membrane but to which the lipid bilayer of the membrane is virtually impermeable. Their transport must therefore be "facilitated" by proteins that span the membrane and provide an alternative route or bypass. 1. Characteristics of facilitated diffusion -occurs down an electrochemical gradient (downhill), similar to simple diffusion. -does not require metabolic energy and therefore is passive. –is more rapid than simple diffusion. -is carrier-mediated and therefore exhibits stereospecificity, saturation, and competition. |
|
|
What is an example of facilitated diffusion? (Diabetes)
|
Example of facilitated diffusion
-glucose transport in muscle and adipose cells in downhill is carrier-mediated, and is inhibited by sugars such as galactose, therefore, it is categorized as facilitated diffusion. In diabetes mellitus, glucose uptake by muscle and adipose cells is impaired because the carriers for facilitated diffusion of glucose require insulin. |
|
|
What are some characteristics of PRIMARY ACTIVE transport?
|
1. characteristics of primary active transport
-occurs against an electrochemical gradient (uphill). -requires direct input of metabolic energy in the form of adenosine triphosphate (ATP) and therefore is active. -is carrier-mediated and therefore exhibits stereospecificity, saturation, and competition. |
|
|
What is an example of Primary Active transport? (Na+ K+ pumps)
|
in cell membranes transports Na+ from intracellular to extracellular fluid and K+ from extracellular to IC fluid, it maintains low intracellular Na+ and high intracellular K+.
-Both Na+ and K+ are transported against their electrochemical gradients. -Energy (ATP) is provided. -The stoichiometry is 3 Na+/2 K+. -Specific inhibitors of Na+, K+-atpase are the cardiac glycoside drugs ouabain and digitals. |
|
|
What type of proteins function in cell-cell signaling, reception, and can form channels for ions?
|
Integral
|
|
|
What is the normal blood glucose level?
|
70-120 mg/ dL
|
|
|
What is the function of glycocalyx?
|
Cell-cell recognition
|
|
|
Which of the following correctly describes the plasmalemma?
|
Phospholipid bilayer
|
|
|
What types of molecules can easily pass through the plasma membrane?
|
Small, hydrophobic
|
|
|
Acetylcholine is packed in a vesicle that is transmitted to the synapse for interaction to the next cell or muscle end plate. What type of transport is this?
|
Exocytosis
|
|
|
What can result in atherosclerosis and subsequent myocardial infarction?
|
Familial hypercholesterolemia
|
|
|
Where does protein synthesis occur?
|
Rough ER and cytoplasm
|
|
|
Which of the following is the precursor for progesterone?
|
Cholesterol
|
|
|
Where is ATP produced in mammalian cells?
|
Mitochondria
|
|
|
A child has an abnormal enlargement of the spleen, liver, and bone marrow. Tests indicate a buildup of glucocerebroside, an intermediate in glycolipid metabolism. What is the diagnosis?
|
Gaucher’s Disease
|
|
|
Free radicals are highly reactive and damage various parts of the cell. What enzyme helps neutralize free radicals, and where is it located?
|
Catalase, peroxisome
|
|
|
Which of the following is the largest polymer in the cytoskeleton?
|
Microtubule
|
|
|
Aneuploidy can result from meiotic or mitotic nondisjunction or omission. An adult has stunted growth, mental retardation, and has a history of cardiovascular problems. Genetic tests indicate a female genotype. Which syndrome is the adult most likely suffering from?
|
Turner’s
|
|
|
Which vitamins will slow aging by helping prevent damage to mitochondria?
|
Vitamins C & E
|
|
|
What are oncogenes?
|
-Genes that affect cell growth and proliferation
-Intact genes that cause cancer when activated |
|
|
Hypocalcemia can result from an ionic imbalance. What is the primary symptom of hypocalcemia?
|
Muscle fatigue
|
|
|
Which types of muscle is innervated by the autonomic nervous system?
|
Cardiac, smooth
|
|
|
A Florida runner is sweating profusely after a long distance race. Which type of gland is most active during this process?
|
Exocrine
|
|
|
A patient’s blood test reveals glucose levels at 130mg/dL. The patient is given synthetic hormones. What type of hormone is most likely administered?
|
Insulin
|
|
|
A doctor treats an exceptionally tall, thin man, with long limbs and fingers. He is concerned that the man might be susceptible to a cardiovascular disorder, and tests him for a genetic condition. What chromosome is most likely mutated?
|
15 (Marfan Syndrome)
|
|
|
Which type(s) of collagen are defective in Ehlers-Danlos Syndrome?
|
I and III
|
|
|
The extracellular matrix is important for...?
|
Cell adhesion (the binding of a cell to a surface)
|
|
|
Which of the following are methods to improve simple diffusion?
|
a. Increasing lipid content of solute
b. Decreasing size of solute c. Decreasing membrane thickness |
|
|
Insulin mostly uses a ______ receptor to allow glucose transport into a cell.
|
GLUT4
|
|
|
The sodium potassium pump operates to establish the proper ion gradient around a cell to allow for proper physiologic reactions. Where does it send these ions, and in what concentrations?
|
3 Na+ outside, 2K+ inside
|
|
|
During hyperpolarization of the action potential, the cell attempts to restore its resting membrane potential. Which of the following drugs would prevent this from occurring?
|
Ouabain
|
|
|
Gastritis occurs from excess HCl in the stomach, which results in irritation. What ion forms an antiport with H+ that allows the acidity of the stomach to increase?
|
K+
|
|
|
A patient exhibits dehydration and has frequent bouts of diarrhea. A doctor notes his blood pressure is slightly high, at 130/90. An MRI reveals local inflammation in the pancreas and GI tract. There is also a buildup of mucus lining the epithelia. What is the diagnosis?
|
Cystic fibrosis
|
|
|
Which cranial nerve triggers a release in ADH from the posterior pituitary?
|
CN 10
|
|
|
Edema can be caused from…
|
a. Albumin deficiency
b. Destruction of blood vessels c. Lymphatic defect |
|
|
Which phase of the action potential occurs with voltage-gated Sodium channels opening, and an influx of Sodium into the neuron?
|
Depolarization
|
|
|
TTX blocks what ion’s channel?
|
Na+
|
|
|
True/False: A 2nd stimulus can occur during the absolute refractory period.
|
FALSE
|
|
|
True/False: Hyperkalemia results in a sharper drop during the repolarization phase, because more K+ is leaving the cell.
|
FALSE
|
|
|
What is a symptom of Myasthenia Gravis?
|
Shortness of breath; (think respiratory muscle weaknesses)
|
|
|
Pheochromocytoma is a tumor to the adrenal medulla. Patients with this condition undergo a 24-hr urine test for elevated levels of…
|
VMA
|
|
|
Parkinson’s can result from…
|
Deficiency in dopamine
|
|
|
What synthetic neurohormone is given to decrease prolactin levels?
|
Dopamine
|
|
|
Which of the following are almost always inhibitory neurotransmitters?
|
GABA and Glycine
|
|
|
True/False: The more H+ the stronger the acid.
|
TRUE
|
|
|
alactosemia is characterized as what type of disorder?
|
Carbohydrate metabolism
|
|
|
Marasmus results from malabsorption and maldigestion of what source of energy?
|
Proteins
|
|
|
True/False: The brain can use ketone bodies for energy.
|
TRUE, but prefers glucose
|
|
|
What is pseudostratified epithelium and why is it considered a false 'stratification'
|
Because the way the nucleus are arranged, it looks like it has multiple layers but it is only simple epithelial tissue
|

