![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
15 Cards in this Set
- Front
- Back
|
describe structure of platelets and there other name |
also called thrombocytes; they are an irregular spindle shaped that will assume other shapes on contact. -about 2-4um |
|
|
Platelet formation |
formed by process called Thrombopoietin. originate from one cell but as the differnetiate more they get larger, as stimulated by hormones they then break off to form smaller parts called platelets. |
|
|
stages of blood coagulation.. |
Stage 1: a) constriction of blood vessels, immediate response to reduce blood flow. b)formation of platelet plug (trigger for later coagulation process).
stage 2 and 3: formation of plug which requires platelets. clotting cascade. |
|
|
stage 1 part a) of coagulation process: |
-exposure of underlying collagen layer, stimulates activation for platelets to adhere to one another. -this triggers release of mediators (ADP and Thromboaxne A2 ) from epithelium; this stimulates more aggregation of platelets and vasoconstriction of blood vessels. |
|
|
stage 1 part b) of coagulation process: |
-chemical reactions take place on surface of platelet to activate prothrombin; can follow Intrinsic pathway (everything in the blood) or the extrinsic pathway (cellular element- in the tissue). |
|
|
Intrinsic activation pathway of prothrombin |

activation due to contact with broken endothelium layer. factor xii --> factor x |
|
|
Extrinsic activation pathway of prothrombin |
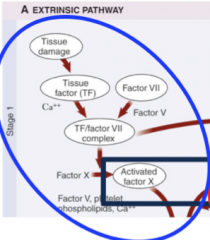
activation due to detection of tissue damage. tissue factor--> factor vii --> factor x |
|
|
once factor x is activated then... |
factor x will activate prothrombin activator, this will bind with calcium to active prothrombin. -prothrombin activates thrombin that activates fibrinogen, which will activate fibrin . |
|
|
components opposing clot formation: |
-endothelium is smooth and secrets prostacyclin which prevent platelet aggregation from occurring all the time. -Nitric acid is also secreted that causes vasodialtion -tissue factor pathway inhibitor released from endothelium stops extrinsic pathway. -antithrombins (Heparin) inhibit thrombin. -Coumadin impairs liver use of Vit K -Asprin also impairs platelet aggregation. |
|
|
What is Fibronolysis? |
process of breaking down blood clot, occurs at the same time as clot formation. -clot is made using Plasminogen. this is the pre-enzyme for plasmin which will breakdown the fibre of the blood clot so that blood will flow again. (plasminogen is activated by tissue plasminogen activator). |
|
|
Blood Groups: Group A; Group B; Group AB; Group O;
|
A; antigen A, Antibody B B; antigen B, Antibody B AB; antigen A and B, no antibody O; no antigen, antibody A and B |
|
|
blood group AB is a? |
universal receiver |
|
|
Blood group O is a ? |
universal donor |
|
|
Rhesus Positive means ...? |
you have an D antigen, about 85% of the population are positive. |
|
|
why does the Rhesus system cause problems with pregnancy? |
it involves igG antibodies that are able to cross the placenta. if the mother is -ve and baby +ve then the D antigen will move across the placenta and the mother will start to produce (at first) igM antibodies, so the baby will not be harmed. however for the second pregnancy if baby is once again +ve , antibodies are already present so igG will develop that is able to cross the placenta and cause the baby to develop anaemia. |

