![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
What are 3 ways in which microbes cause disease?
|
1. Contact or enter host cells and directly kill them (e.g. viruses inhibiting cellular nucleic acid synthesis &/or causing cell lysis)
2. Release factors that indirectly kill cells (e.g. exotoxins & endotoxins) 3. Induce a host response that harms the host as well as the microorganism (e.g. suppuration, scarring, allergic reaction) |
|
|
What are the 2 main types of acute inflammatory responses to infection?
|
Suppurative
(pus formation, with oedema, fibrin, neutrophils…) E.g. Acute lobar pneumonia: 1. Congestion & Consolidation 2. Red hepatisation 3. Grey hepatisation 4. Resolution or organisation Necrotizing (rapid/severe tissue destruction; little time for inflammation) E.g. Clostridium perfringens (strong toxins) |
|
|
What are the 3 main types of chronic inflammatory responses to infection?
Note: One type has 2 sub-types. |
Cytopathic & Cytoproliferative
(viral damage in the absence of host inflammatory response) E.g. • Inclusion bodies (CMV); • Cell fusion (RSV); • Blisters (HSV); • Cell proliferation (warts) Mononuclear & Granulomatous 1. Mononuclear • Lymphocytes (e.g. viral) • Plasma cells (e.g. syphilis) 2. Granulomatous • Slow-dividing organisms (e.g. TB) • Large size (e.g. helminths) Chronic Inflammation & Scarring |
|
|
What are 3 ways in which microbes cause disease?
|
1. Contact or enter host cells and directly kill them (e.g. viruses inhibiting cellular nucleic acid synthesis &/or causing cell lysis)
2. Release factors that indirectly kill cells (e.g. exotoxins & endotoxins) 3. Induce a host response that harms the host as well as the microorganism (e.g. suppuration, scarring, allergic reaction) |
|
|
What are the 2 main types of acute inflammatory responses to infection?
|
Suppurative
(pus formation, with oedema, fibrin, neutrophils…) E.g. Acute lobar pneumonia: 1. Congestion & Consolidation 2. Red hepatisation 3. Grey hepatisation 4. Resolution or organisation Necrotizing (rapid/severe tissue destruction; little time for inflammation) E.g. Clostridium perfringens (strong toxins) |
|
|
What are the 3 main types of chronic inflammatory responses to infection?
Note: One type has 2 sub-types. |
Cytopathic & Cytoproliferative
(viral damage in the absence of host inflammatory response) E.g. • Inclusion bodies (CMV); • Cell fusion (RSV); • Blisters (HSV); • Cell proliferation (warts) Mononuclear & Granulomatous 1. Mononuclear • Lymphocytes (e.g. viral) • Plasma cells (e.g. syphilis) 2. Granulomatous • Slow-dividing organisms (e.g. TB) • Large size (e.g. helminths) Chronic Inflammation & Scarring |
|
|
Upper Respiratory Tract diseases
Acute otitus media: Name infecting organisms, with corresponding comments Note: Acute Sinusitis has similar aetiology and pathogenesis. |
Viruses
(esp. Respiratory syncytial virus) [Cause at least 50% of URTs] Streptococcus pneumoniae Haemophilus influenzae Moraxella catarrhalis Streptococcus pyogenes Staphylococcus aureus [Generally secondary infection; most commonly nasopharyngeal residents; fluid often stays in middle ear for weeks to months (glue ears)] |
|
|
Upper Respiratory Tract diseases
Otitus externa: Name infecting organisms, with corresponding comments |
Staphylococcus aureus
Candidiasis albicans Gram -ve pathogens [External ear canal contains normal flora, warm moist environment] |
|
|
Upper Respiratory Tract diseases
Acute epiglottis: Name infecting organisms, with corresponding comments |
Haemophilus influenzae (type b)
[Organism spreads from nasopharynx to epiglottis] |
|
|
Upper Respiratory Tract diseases
Pharyngitis: Name infecting organisms, with corresponding comments |
Viruses
[Cause ~70% of sore throats] Streptococcus pyogenes [10-20% acute cases, sudden onset] Neisseria gonorrahoeae [Often asymptomatic, usu. via orogenital contact] Corynebacterium diphtheriae [Mild but toxic illness, can be severe] Haemophilus influenzae [Epiglottis] |
|
|
Name 4 normal flora of the mouth
|
Streptococcus mitis & other Streptococci (including Viridans)
Candida albicans Bacteroides spp. Lactobacillus spp. |
|
|
Name 7 normal flora of the nasal cavity and throat
|
Staphylococcus epidermidis
Staphylococcus aureus (carriers) Streptococci (including Viridans) Corynebacterium spp. Moraxella spp. Haemophilus spp. Neisseria spp. |
|
|
Name 3 pathogens of the mouth
|
Fusobacterium spp.
Actinomyces Candida albicans (opportunistic infection) |
|
|
Name 7+ pathogens of the nasal cavity and throat
|
Staphylococcus aureus
Streptococcus pyogenes Corynebacterium diphtheriae Haemophilus influenzae Streptococcus pneumoniae Moraxella catarrhalis Viruses: e.g. adenoviruses, rhinoviruses, influenza, RSV… |
|
|
Streptococcus pyogenes (Group A Strep)
Describe bacteria, disease, and complications |
• Gram +ve cocci, β – haemolytic, bacitracin sensitive
• Major cause of pharyngitis (‘strep throat’) • Complications include otitis media, sinusitis, acute glomerulonephritis, scarlet fever & rheumatic fever |
|
|
Streptococcus pyogenes (Group A Strep)
Describe virulence factors |
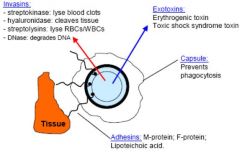
|
|
|
Streptococcus pneumoniae:
Describe virulence factors |
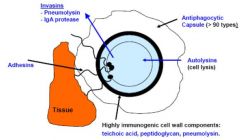
|
|
|
Streptococcus pneumoniae
Describe bacteria, disease, and complications |
• Gram +ve cocci, α – haemolytic, optochin sensitive
• Acute otitis media, sinusitis, LRTI’s (pneumonia), meningitis • 23-valent & 7-valent vaccines available (23-valent doesn’t work in children < 2 yrs old) |
|
|
Haemophilus influenzae:
Describe bacteria, disease, complications, and virulence factors |
• Gram –ve rods, can be capsulated or non-capsulated
• Acute otitis media, sinusitis, epiglottitis, LRTI’s (pneumonia), meningitis… • Virulence factors: capsule, outer membrane proteins, endotoxin, fimbrial & non-fimbrial adhesins, IgA protease, autolysins • Hib vaccine available (against type b capsule); however, non-typable strains have ~40-80% nasopharyngeal carriage, and are a significant cause of otitis media |
|
|
Moraxella catarrhalis:
Describe bacteria, disease, complications, and virulence factors |
• Gram –ve coccobacilli
• Acute otitis media & sinusitis in children (especially high colonization/carriage rates in indigenous children) • Virulence factors: Capsule, outer membrane proteins, adhesins, endotoxin |
|
|
Corynebacterium diphtheriae:
Describe bacteria, disease, complications, and virulence factors |
• Gram +ve rods (distinctive black colonies on tellurite agar)
• Diphtheria – rare in developed world • Virulence factors: diphtheria toxin (inhibits protein synthesis); toxoid = basis for vaccination |
|
|
What is over 50% of the "common cold" cases caused by?
|
Rhinoviruses and coronaviruses
|
|
|
What can Viral Upper Resp Tract Infection (URTI) can progress to?
|
Viral pneumonia
|
|
|
Viral respiratory infections:
"Restricted to surface" types - Give examples - Name consequences |
Common cold viruses
Influenza Streptococci in throat Candida albicans (thrush) Local spread Local (mucosal) defenses important Adaptive (immune) response sometimes too late to be important in recovery Short incubation period (days) |
|
|
Viral respiratory infections:
"Spread through body" types - Give examples - Name consequences |
Measles, munmps, rubella
Q fever Little or no lesion at entry site Microbe spreads through body, returns to surface for finall multiplication and shedding, e.g. salivary glands (mumps, CMV, EBV), resp tract (measles) Adaptive immune responce important in recovery Longer incubation period (weeks) |
|
|
Which levels of the respiratory tract can resp viruses infect?
|
Any level, although preferred sites exist
- e.g. URT for Rhinoviruses. |
|
|
List 6 antimicrobial defences in resp system, and the factors that impair each one.
|
1. Cough reflex (stroke, brain tumours, laryngeal cancer, etc.)
2. Filtering by nasal cavity 3. Mucociliary action (impaired by viral infection, cigarette smoke, etc.) 4. Phagocytosis by alveolar macrophages (smoke, alcohol, oedema, etc.) 5. General host immunity (immunosuppressed states) 6. Normal flora - URT only |
|
|
UP TO CASE 10 P19 - PATHOPLYSIOLOGY OF MIDDLE...
|
HKJKH
|

