![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
136 Cards in this Set
- Front
- Back
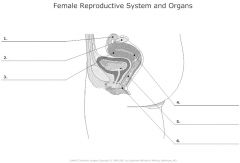
Female reproductive system labeling |
|
|
|
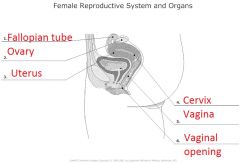
Female reproductive system labelled facing forward |

|
|
|
More detailed labeling of female reproductive system |

|
|
|
More detailed labeling of female reproductive system labelled facing forward |

|
|
|
Spontaneous ovulation |
Rats and humans show spontaneous ovulatory cycles in which ovulation, the release of the egg (ova) from the follicle of the ovary, occurs spontaneously or, more or less independently of external stimulation.
|
|
|
Induced ovulation |
Induced ovulation which occurs in cats, rabbits, mink, etc., is when the female comes into heat or estrous automatically, but does not ovulate without external stimulation. The female shows sexual arousal but mating stimulation is necessary to complete the cycle and induce ovulation. |
|
|
Granulosa cells and secondary oocytes |

|
|
|
What happens to a follicular cell when it is released? |
Only one follicle will grow, and it secrets more and more estrogen. This feedbacks positively and increases the LH surge likelihood. Surge of LH triggers oocyte expulsion into interstitial space. Corpus luteum in left over, and it starts to secrete progesterone. Progestation - hormone. progesterone maintains mucous and vasculerization of the endometrium for potential implantation. If no fertilization, the corpus luteum will die into the corpus albicans. |
|
|
Describe the follicles during the ovarian cycle |
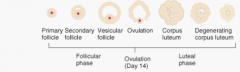
|
|
|
Describe the work of hormones during the uterine cycle |
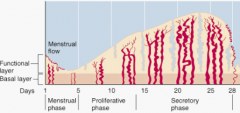
Most consider menstrual phase as part of follicular phase, were estrogen is increasing. Luteal phase is where progesterone levels peek. |
|
|
What occurs in the endometrium? |
Blood vessel development, and where the uterine lining disintegrates during a period. |
|
|
What is the endometrium composed of? What cell layers does it have? |
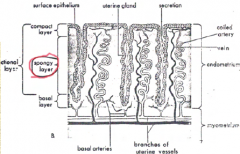
Surface epithelium is part of the spongy layer, and the uterine gland is within. |
|
|
What happens to FSH and LH during ovulation? |
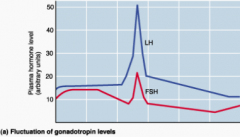
FSH peaks when the follicle cells/granulocytes went through. LH peaked when the egg is released. |
|
|
What happens to estrogen and progesterone during ovulation? |

Estrogen rises while follicular cells are maturing, and progesterone rises and stays up after egg is released, to help sustain a pregnancy if the egg gets fertilized. Progesterone is secreted by the corpus luteum. |
|
|
The female hypothalamic-pituitary-gonadal feedback cycle |
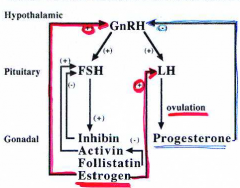
Only one GNRH, but estrogen is not increased by corpus luteum by inhibin feedbacking to slow down FSH production. Many cells won't secrete testosterone until primed by estrogen. Progesterone feedbacks to shut off its activation quickly. Activan activates FSH and increasing follistatin which shuts down reproduction of activin. |
|
|
Amenorrhea |
Failure to menstruate |
|
|
Dysmenorrhea |
Painful or difficult menstruation |
|
|
Menorrhagia |
Excessive menstrual bleeding |
|
|
Oligo menorrhea |
Infrequent or irregular menstrual bleeding |
|
|
Factors that disrupt menstrual cycle |
1. Pregnancy 2. Lactation 3. Stress 4. Starvation/anorexia 5. Exercise |
|
|
Contraceptive methods used in the US |
Sterilization - 38% - Once a woman has her fallopian tubes "tied", it is difficult to reverse the procedure. Oral contraceptives - 32% - The pill is 95% to 97% effective, but questions about its safety persist. Barrier methods - 24% - Condoms, diaphragms and cervical caps have failure rates of 12% or more. Intrauterine devices - 3% - Most manufacturers have stopped making IUDs for fear of costly lawsuits. This method fails in 6% of women. Spermicides - 3% - Foams, creams, and jellies are sold over the counter, but failure rates are about 26%. |
|
|
Contraceptive methods abroad |
Noristerat - This two-month injectable contraceptive has a 2% failure rate and is approved for use in more than 40 countries. Norplant - Placed under the skin on the inside of the upper arm, this progestin-releasing implant can provide 99% protection for up to 5 years. RU-486 - This pill can induce menstruation in a woman whose period is up to six weeks late. Filshie clip - This titanium-and-silicone clip can block the Fallopian tubes without cutting or cauterizing, making it easier for a woman to change her mind. |
|
|
Birth control (oral) works by |
Containing estrogen, progesterone, and sometime progestin. They put the hormones in your body that mimics pregnancy, so the release of the oocyte does not happen. |
|
|
Physical side effects of oral contraceptives |
1. Lower progesterone and testosterone levels. 2. Breast enlargement. 3. Decreased menstrual bleeding. 4. Weight gain and water retention. 5. Headaches, nausea, cramps. 6. Increase in blood clots and heart attacks. 7. Increase in breast, uterine and cervical cancer. |
|
|
Psychological side effects of oral contraceptives |
1. May increase depression (high progestin pills) 2. May increase nervousness (high estrogen pills)
Birth control pills also decrease the variability of physical and behavioural changes over the menstrual cycle. |
|
|
Estrus cycle |
– recurring physiologic changes induced by reproductive reproductive hormones in most female mammals |
|
|
Attractivity |
– How ‘attractive’ the female makes herself to a potential mate |
|
|
Proceptivity |
– Active solicitation on the part of the female |
|
|
Receptivity |
– Active acceptance of mounting and copulating. Example of receptivity is lordosis. |
|
|
Lordosis |

Lordosis is a form of receptivity, especially in rats. The term lordosis refers to the normal inward curvature of the lumbar and cervical regions of the spine. Excessive or hyperlordosis can happen and lumbar hyperlordosis is commonly referred to as sway back, hollow back or saddle back, a term that originates from the similar condition that arises in some horses. A major factor of lordosis is forward pelvic tilt, when the pelvis tips forward when resting on top of the thighs. Curvature in the opposite direction is termed kyphosis. Sometimes the word lordosis is used to mean "hyperlordosis" but this is incorrect use of the word. |
|
|
Estrus cycle in rats |

A surge of LH causes expulsion of ova (multiple), as a result corpus luteum secretes progesterone. The progesterone increased before release in proetsrus. This blip is many luteal cells only secrete progesterone when primed by estrogen. |
|
|
Behavioural changes during the ovulatory cycle (rats) |

During estrus, sexual behaviour goes up, aggression goes slightly down, activity (wheel-running) goes up, feeding goes down because you need to mate and don't have time to think about food, scent-mark goes up in order to spread pheromones to attract a mate, olfactory activity goes up, pain perception goes down, and emotionality goes down. |
|
|
Changes in vaginal cells over the estrus cycle of the rat |
Cells seem cornified during estrus, compared to other stages. Metestrus is partially cornified. |
|
|
Species differences in female sexual receptivity |
Rats and squirrel monkeys are only sexual during estrus, whereas rhesus monkeys and humans are sexual at all other times. |
|
|
Changes in body temperature over the menstrual cycle in females |
Temperature peaks just before ovulation, then drops off. Progesterone only is produced largly after ovulation. |
|
|
Changes in physiological responses over the menstrual cycle |
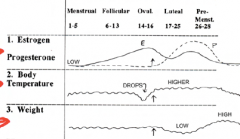
Temperature increases before and after ovulation, weight is lowest right after ovulation, then increase right before menstruation. |
|
|
Changes in behavioural responses over the menstrual cycle |
During ovulation, positive feelings increase, negative feelings decrease, sexual activity increases, sensitivity to visual, auditory, and tactile stimuli increases, and sensitivity to pain and cold decreases, but increases afterwards at luteal and premenstrual stages. |
|
|
Changes in olfactory sensitivity over the menstrual cycle in 5 women |
Increased sensitivity during follicular stage, and decreased sensitivity during luteal stage. |
|
|
Possible neuroendocrine mechanisms for the change in food intake over the menstrual cycle |
- As progesterone increases, fat and food intake increases - As estrogen increases, fat and food intake decreases
|
|
|
PMS |
-Also called PMDD (premenstrual dysphoric disorder) -Time right before menstrual syndrome -Common symptoms include tiredness, irritability, depression, red eye, hay fever, acne, hoarseness, tender breasts, appetite cravings, bloated abdomen (from water retention), backache, painful joints, and swollen ankles. |
|
|
Effect of oral contraceptives on PMS symptoms |
Less irritability, mood swings, depression, and tension. |
|
|
Psychopathology and the menstrual cycle |
Premenstrual = late luteal. Menstrual and PMS have increased depressive behaviors. |
|
|
Four different patterns of PMS symptoms |
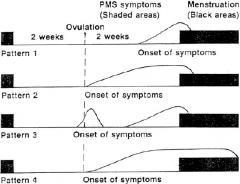
|
|
|
Premenstrual syndrome: causes and cures |
1. Low progesterone level; estrogen/progesterone imbalance
Cures: progesterone therapy (natural or synthetic), works to relieve symptoms of some patients.
2. Increased aldosterone, renin and angiotensin II, increase in sodium and water retention
Cures: aldosterone antagonists (spirono lactone), lithium (diuretic), work to reduce fluid retention and bloating only
3. Low dopamine levels, therefore, high prolactin secretion and high alpha MSH secretion
Cures: L-dopa/bromocriptine (dopamine agonist), relieve sore breasts may reduce water retention
4. Low norepinephrine (high MOA levels)
Cures: MAO inhibitors (parnate), relieves depression
5. Elevated luteal opiate levels drop, therefore, opiate withdrawal
Cures: Naloxone to reduce luteal rise in opiates. Effectiveness? Unknown.
6. Elevated prostaglandin levels
Cures: Prostaglandin inhibitors (aspirin, mefenamic acid), reduce dysmenorrheal (back and headache, tension, dizziness)
7. Vitamin B6 (pyridoxine) deficiency
Cures: B6 treatment, questionable
8. Psychosomatic disorder or social stress or mood disorder
Cures: Psychotherapy, social support, tranquilizers, reduce stress, conflict, but not somatic symptoms |
|
|
Why has no one found a "cure" for PMS? |
-No animal model for research -Despite enormous efforts to isolate a single or multiple endocrinological cause of PMS, the causal status remains obscure. -Given the complex array of hormonal symptoms and feedback, which underlies the menstrual cycle, the impact of these symptoms on the CNS function and the large number of symptoms, which occur during PMS, it is unlikely that the cause is a single hormonal abnormality. |
|
|
Definition of stress |
–The force exerted on the body which tend to create an imbalance in the system or a need for the animal to perform a physiological or behavioral response to in order to cope with the stimulus. |
|
|
Physical or psychological stressors |
–Physical-bodily damage –Psychological-affect the body w/out physical damage |
|
|
Central nervous system in response to stress |
Regulates our response to stress. Perspective on things elevates stress response. |
|

|
Eustress means levels of positive stress and distress means levels of negative stress. Eustress = positive experience Distress = unpleasant experience When it is close to "normal" baseline from the right side, one feels "boredom". Between baseline and unpleasant experience is feeling just not great and having a bad day. |
|
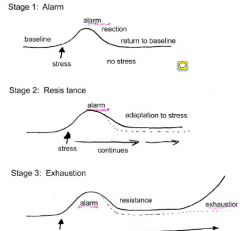
Selye's general adaptation syndrome |
First stage stress is temporary, second the level does not stay at normal levels: the SNS is still active, your system is still catabolic, and hormones are still being pumped through your system. Adaptation illness exhaustion: another sress when you never went back to base line. you will then have a physical and or mental breakdown. |
|
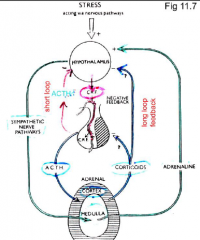
Stress acting via a nervous pathway |
A goes back to hypothalamus as positive feedback loop. Hypothalamus impulses piuitary via CRF, to secreate ACTH which effects adrenal cortax to serete cortisol. Cortisol inhibits immunesystem (why you're sick after stress), and goes to liver and decreases catabolic activeity (less energuy transeferd to body). These are also negatively feedbacking to hypothalamus and ptuitary. |
|
|
Somatic motor system |
SMS is voluntary motion via somatic neurons to skeletal muscles. |
|
|
Autonomic nervous system |

In the preganglionic fiber, acetylcholine is the neurotransmitter. In the postganglionic fiber: SNS: noradrenaline, ATP, acetylcholine (sweat glands and blood vessels) and NPY PSN: acetylcholine, peptides |
|
|
SNS and PNS divisions in the autonomic nervous system |
SNS is not only activated in stressful responses, but there are times when your SNS is activated all the time: if you have low blood pressure, water retention in large intestine. If you need to increase heart rate during run or what not, will raise it as well. ANS for bladder function, sexual funtion (erection), but SNS dos ejaculation. Along spine, especially in lumbar section with motor SNS ganglia. prevertal ganglia are closer to the organ, extending in away from the spine. The SNS is largely responsible for catabolic metabolism. PNS is largely responsible for anabolic metabolism: building. Mostly in sacral area. |
|
|
ACh in sympathetic and parasympathetic nervous system |
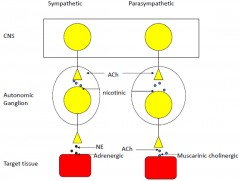
Post ganglion accepts Ach to muscarinic cholonergenic, but they both release Ach from CNS. |
|
|
Metabolic stress |
•Catabolic-Sympathetic nervous system –Fight or flight •Anabolic-Parasympathetic nervous system –Hormone rebound Growth is inhibited during periods of chronic stress-‘psychosocial dwarfism' |
|
|
How worry affects hormone levels |
-Adrenaline and cortisol levels skyrocket during stress |
|
|
Advantages to pups handled in infancy |
Rats handled in infancy show a reduced stress response (lower corticosteroid release and faster return to baseline) than non-handled rats. Also, learning is increased by handling because high corticosteroid levels in non-handled rats may cause deterioration of hippocampal cells which are important for spatial learning. |
|
|
The effects of stress on hippocampal cells |
•Very easily damaged •Hypercortisolemia may affect hippocampal cells -May cause diabetes -is cell degeneration of hippocampal cells (memory) handling found faster cortisol levels are elevated in non- handled mice to the extent the hippocampal cells are damaged and memory is diminished.
|
|
|
Behavioural symptoms of stress |
1. Tiredness, irritability, apathy 2. Accident proneness 3. Sudden loss or gain in weight (anorexia or binge eating) 4. Increased drinking, smoking, or drug use 5. Insomnia; nightmares; bedwetting (children) 6. Impotence; sexual problems 7. Aggression: baby battering; wife beating 8. Anxiety, depression, suicide attempt 9. Phobias; obsessive-compulsive behaviour 10. Poor job performance 11. Lack of concern and creativity 12. Withdrawal, day dreaming, nostalgia 13. Absenteeism 14. Excessive concern for minor problems` |
|
|
Stress effects on the immune system |
•Increases ACTH release •Inhibits thymus activity –reduced immunological efficiency |
|
|
Hormonal changes in stress |
i) Increase in catabolic hormones Epinephrine, growth hormone, glucagon, and cortisol promote carbohydrate, fat, and protein breakdown. Vasopressin and aldosterone promote Na+ and H20 conservation - maintain high blood pressure - conserve H20 and Na+ lost in sweat. ii) Decrease in anabolic hormones Insulin promotes synthesis of glycogen fat and protein. Testosterone and estrogen promote protein synthesis and sex drive. Calcitonin promotes bone formation. LH and FSH promotes gonadal stimulation and sex drive. |
|
|
Long term effects of high corticosteroid levels |
-suppression of anabolic processes -muscle atrophy -decreased sensitivity to insulin: steroid - induced diabetes -hypertension -arterial disease -amenorrhea (decreased LH and decreased FSH) -impotence -immunosuppression (decreased thymus) -damage to hippocampus (reduced type II receptors) in old age -reduced cognitive abilities in old age
These occur when negative feedback of glucocorticoids fails. |
|
|
Monogamy |
1male-1 female pair bond – Biparental |
|
|
Polygamous |
Not monogamous |
|
|
Polygyny |
Many women, one man. |
|
|
Parental Behaviours in Rodents |
-Nest building -Crouch over pups in a nursing posture -Lick pups -Retrieve pups |
|
|
Lactation and Maternal Behaviour in the rat |
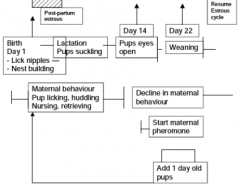
|
|
|
The relationship between maternal behaviour and pup development |
As time progresses, eyes start to open, pups leave nest etc, pup retrieval decreases. |
|

|
Transfusion of blood from maternal females induces rapid onset maternal behaviour in virgin female rats. Injection of estrogen, progesterone, and prolactin activates maternal behaviour in ovariectomized nulliparous females within 48 hours of pup exposure. |
|
|
Location of estrogen receptors |
-Basically everywhere
|
|
|
Prolactin in female rats |
Prolactin is necessary to facilitate Estrogen/Progesterone priming of maternal behaviour in hypophysectomized ovariectomized nulliparous female rats. There is greater progesterone in hypophysectomized over intact. |
|
|
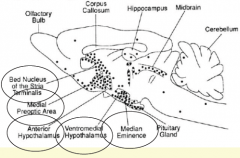
Oxytocin in female rats |
Oxytocin injections into the cerebral ventricles induces immediate maternal behaviour in estrogen-primed ovariectomized nulliparous female rats. Infusion of oxytocin into the olfactory bulbs of estrogen-primed virgin female rats stimulates immediate maternal behaviour. |
|
|
Morphine in female rats |
Morphine inhibits the onset of maternal behaviour in day 17 pregnancy-terminated rats, and this effect is reversed by naloxone. |
|
|
The dual olfactory pathways in rats |
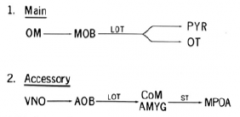
Both the main and accessory olfactory pathways may be important in mediating maternal behaviour. |
|
|
Direct parental care |
Huddle and sleep with pups Groom and clean pups Retrieve and carry pups Provide food for pups Active defense of pups Care of pups in the absence of a female Play and socialization of pups |
|
|
Indirect parental care |
Secure resources Build nests and shelters Antipredator sentinel Provide care to the mother Territorial defense |
|
|
Survivor rates when father is present |
Warm ambient temperatures -Higher survival rate if father is absent Cold ambient temperatures -Higher survival if rather is present Foraging for food -Higher survival rate if father is present |
|
|
Treatment of infertility |
PMSG - acts as FSH Clomiphene - anti-estrogen - enlarges ovaries *Blocks Estrogen receptors in hypothalamus and pituitary, therefore, reduces negative feedback, allowing more FSH to be released. HCG - acts like LH to stimulate ovulation |
|
|
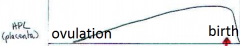
HCG on pregnancies |
HCG levels increase about 3 weeks after the embryo becomes implanted in the uterine wall. |
|
|
Aschheim-Zondek |
(AZ or mouse test) – several mice injected with urine – look for hemorrhagic follicles – results available after 96hrs
|
|
|
Freidman |
(Or rabbit test) – rabbits are induced ovulators – inject with urine specimen – if HGC present in urine- rabbits will produce corpus luteum (takes 48 hrs) |
|
|
Galli-Mainini |
(or Frog test) – pregnancy urine can induce spermiation in frogs and toads – results in 2-4 hours – high false negative rate due to seasonal variations |
|
|
Immunological tests |
1-2 hours -involves production of HCG antibodies and displacement of labeled HCG by unlabeled - like a radioimmunoassay. |
|
|
Agglutination tests |
5 min to 2 hours -The HCG antibody is placed on latex. HCG in urine combines with antibody and latex agglutinates. |
|
|
Agglutination inhibition tests |
5 min to 2 hours HCG in urine combines with antibody and inhibits agglutination of latex particles. |
|
|
Two different monoclonal antibodies combined in an HCG test system |
One antibody specifically reacts with intact HCG and does not react with HLH. The second antibody reacts with the B-subunit of HCG and less strongly with the B-subunit of HLH. |
|
|
HCG levels rise as... |
...estrogen and progesterone levels are decreased. HCG levels are low when estrogen and progesterone levels are high. |
|
|
Hormone levels of prolactin in pregnancy |
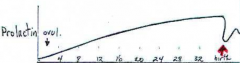
Increased during ovulation and pregnancy, decreased during birth. |
|
|
Hormone levels of HPL (placenta) during pregnancy |
Increases all throughout ovulation and pregnancy, and goes down during after-birth, when the placenta comes out. It is at its peak during birth. |
|
|
Relaxin and oxytocin |

|
|
|
Hormone changes in the adenohypophysis during pregnancy |
ACTH: 0 - (no change) Prolactin: ++ TSH: 0 GH: 0 FSH: .. (very low) LH: .. (very low) |
|
|
Hormone changes in the neurohypophysis |
Vasopressin ? Oxytocin + (near parturition_ |
|
|
Hormone changes in the ovary |
Estrogen + Progesterone + |
|
|
Hormone changes in the adrenal cortex |
Cortisol + |
|
|
Pancreas |
Insulin - (inhibited by HPL) |
|
|
Placenta |
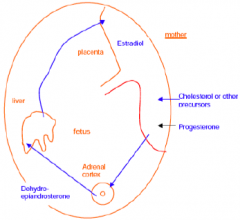
An "incomplete" endocrine gland (Feto-placento-maternal unit). Progesterone -> appetite, diverts glucose into fat synthesis Estrogens -> growth and development of breast, uterine muscles -> changes in carbohydrate metabolism, protein synthesis, thyroid and adrenal function |
|
|
Pregnenelone |
Increases the receptivity of the uterus to relaxin before birth. |
|
|
Human Placental Lactogen (HPL) |
Insulin inhibitor, released from the placenta. |
|
|
Pregnancy maintenance, with progesterone and estrogen |
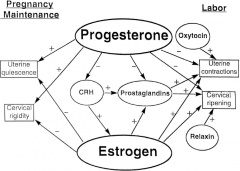
|
|
|
Parts of the breast |

|
|
|
Diagram of a cluster in the mammary gland of a goat |

|
|
|
Prepubertal development in mammary glands |
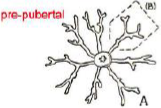
-Uses growth hormone and thyroxine
|
|
|
Differentiation of mammary glands during puberty |
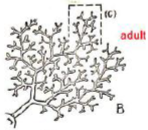
-Uses growth hormone, estrogen and progesterone, and corticosteroids
|
|
|
Differentiation of mammary glands during pregnancy |
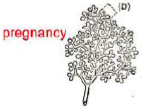
-Uses corticosteroids, estrogen and progesterone, prolactin, and growth hormone (HPL) |
|
|
Lactation in mammary glands |
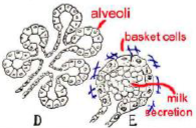
-Uses corticosteroids, prolactin, and oxytocin |
|
|
Stimulation of oxytocin release |
Can be caused by pup suckling, neural inputs from the mammary gland and reproductive tract. |
|
|
Milk Secretion and Ejection |

|
|
|
Oxytocin and prolactin release during Nursing |
Oxytocin, but not prolactin, shows a conditioned release to the baby's cries |
|
|
Neuropsychology and neuropsychological tests |
Neuropsychology: The study of the relationship between brain and behaviour/ cognition Neuropsychological Tests: A special class of psychological tests that samples sensory, perceptual, cognitive or motor skills for which the integrity of a particular region of the brain is known to be essential. |
|
|
Growth hormone |
• Required for proper growth and development • Somatotropin • Growth factors • GH has its effects pre/perinatally • Mediates brain development • Works through IGFs • Lack of GH during development leads to short stature |
|
|
Cognitive functioning differences between patients with idiopathic growth hormone deficiency vs. those with short stature |
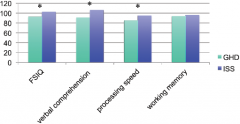
|
|
|
Sex differences in cognition |
Men>Women • strength • visuospatial • mental rotation • quantitative
Women> Men • verbal skills • perceptual speed and accuracy • fine motor skills |
|
|
Methods to test mental rotation |
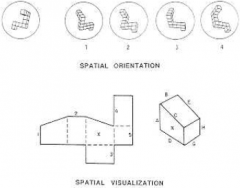
Boys ended up testing better but it was cultural thing and how they were raised, and the differences were not significant. |
|
|
Sex differences in cognition: Hypothetical Cognitive Task where men>women |

The only place where they're actually different is weight and strength. |
|
|
Sex differences in cognition: Organizational or Activational? |
• Unknown- cannot manipulate hormonal millieu in a developing (human) fetus • sex difference appear at puberty • Experiments of nature – CAH – androgen insensitivity – women exposed to DES (in utero) |
|
|
Pathways to sexual differentiation |
XY chromosomes -> SRY expressed XX chromosomes -> No SRY expressed
|
|
|
Precursor to sex hormones |
Pregnenelone is precursor to testosterone. Testosterone has two different pathways. 5-alpha-reductase turns testosterone into 5-alpha-DHT. Testosterone via aromatase leads to estrogen. Pregnenelone also leads to cortisol when not taking the testosterone route. If your body is making too much cortisol, it is not making enough testosterone, and if your body is making too much testosterone, it is probably not making enough cortisol. |
|
|
Androgens and Cognition: Congenital Adrenal Hyperplasia (also called salt wasting disease, because if you don't have enough cortisol, you experience osmodisregulation, like your ions are unbalanced, which is also called adrenogenital syndrome) |
• Genetic defect; specific enzyme missing, so cortisol is not secreted (see figure) • too much converted into adrenal testosterone during development • male brain development pattern • increased spatial abilities,poorer perceptual speed, and higher frequency of specific learning disabilities. |
|
|
CAH girls with salt wasting showed best performance on spatial tasks |
Improved spatial function in girls with CAH not reliably found This study broke down the subject groups into SW and SV subtypes Only the SW subtype showed the ‘male type’ pattern on spatial tasks. |
|
|
Androgens and Cognition: Androgen insensitivity |
• Testicular feminization syndrome • x-linked recessive trait (46XY) • failure to code (or mutated) testosterone receptors • normal androgen secretion; yet, cells insensitive to it • phenotypically female-- femininized brain • Lower PIQ than VIQ- no strong findings |
|
|
AIS males demonstrate cognitive test scores that are more similar to normal females |
Studies in AIS are rare. Study showing that males who have AIS mutation look more like females on a difference score of verbal comprehension minus perceptual organization No differences were found on FSIQ or VIQ. PIQ was highest in normal male siblings. |
|
|
Androgens and Cognition: Diethyl stilbestrol (DES) |
• Females exposed in utero to DES (antiemetic/miscarriage prevention) • masculinizes or de-feminizes females • masculine type brain • Few differences noted |
|
|
Women who were exposed to DES prenatally do not differ from their unaffected (same sex) siblings on spatial cognitive functioning |
No differences noted between affected and unaffected sibs on spatial tasks However, women who had been exposed later in gestation may be more affected than those who were exposed earlier |
|
|
Cognition and the menstrual cycle: Plasma concentration of hormones across the menstrual cycle |
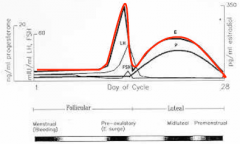
|
|
|
Cognition across the menstrual cycle: The Female Fertilization Cycle |
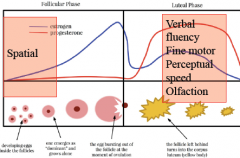
|
|
|
Conclusions from menstrual studies |
In Premenopausal women: • Estrogen has negative effects on spatial skills • Estrogen facilitates simple verbal tasks • Differences in cognitive function not likely to be confounded with alterations in mood • Effect sizes small |
|
|
Methodological issues in menstrual studies |
• Small sample sizes • Failure to verify actual menstrual phase • Use of cognitive tests that are inappropriate for detecting changes in performance • Interpretation of non-significant findings as if they were statistically significant • Use of idiosyncratic terminology for identifying phases of cycle • Selection of inappropriate phases for testing |
|
|
Menopause on cognition |
• Average age 50.8 • Menopause-- occurs over time (up to 2 years for estrogen levels to decrease) • Anecdotal evidence from menopausal women • Aging process may influence cognitive decline independently |
|
|
Surgical menopause: the effects of estrogen or placebo on verbal memory |
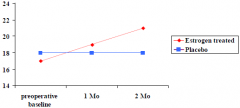
|
|
|
Women’s Health Initiative Memory Study (WHIMS) |
• Subset of women from the Women’s Health Initiative Study (n=161,808 post menopausal women) • Halted prematurely when a increased risk of cardiovascular events and certain forms of cancer • All women were over 65 at the time of study entry • 4552 CEE+medoxyprogesterone or placebo • 2947 CEE vs. placebo • No effect on cognition or on the prevalence of dementia • Negative study |
|
|
What WHIMS failed to answer |
• All women started HRT LONG after menopause; what happens if HRT is initiated perimenopausally? • CEE does it cross the BBB? What about 17β-estradiol? • More research needed |
|
|
Menopause in healthy women: effects of estrogen replacement |
• Recall and recognition of lists of words, word pairs or short paragraphs impaired after menopause. • Most robust finding is of enhanced verbal memory with estrogen • Non-verbally mediated cognitive tasks unaffected by estrogen • SERMs do not affect cognition |
|
|
Methodological issues in menopausal studies |
• Self-report measures of memory change • Few neuropsychological tests administered • Concomitant use of other medications • Dose differences and plasma levels not measured • Independence of mood change? • Estrone vs. 17-β estradiol vs. CEE and route of administration • Progestins? |
|
|
Hormones and Alzheimer’s Disease |
• Prevalence women>>men • Severe cognitive deficits in AD • HRT- improves cognitive function • 30-50% reduction in risk of AD in women treated with HRT • Later age of onset in AD women treated with HRT |
|
|
Estrogen treatment in Alzheimer’s Disease: Possible mechanisms of action |
• Neuronal survival and repair – amyloid precursor metabolism – nerve growth factor activity • Neuronal function – neurotransmitter systems – glucose utilization • Vasculature – improve blood flow – prevent cerebrovascular disease |

