![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
Hormones and types |
Endocrine system - using hormones as signalling molecules
Transport in blood
Two types of hormone
Protein and peptide hormones - not soluble in the phospholipid membrane so don’t enter the cell and use a secondary messenger
Steroid hormones - pass through the plasma membrane and enter the cell to have a direct effect on DNA - receptor molecule inside cell to form complex to cause the production of mRNA
Endocrine hormones are released directly into the blood - ductless
Exocrine hormones are stored or into a duct |
|
|
Detecting the signal |
Hormones are transported all around the body but only have an effect in one type of tissue only Receiving the signal are the target cells or grouped as target tissue Specific receptor shape on cell surface membrane for non-steroid hormones |
|
|
First and second messengers |
Non-steroid messengers are first messengers and can’t pass through the plasma membrane They bind to a specific receptor shape and trigger a secondary messenger inside the cell which stimulate a response inside the cell Many non-steroid hormones act via a G protein in the membrane which is activated when the hormone binds The G protein activates an effector molecule - usually an enzyme to convert an inactive molecule into the active secondary messenger In many cells the effector molecule is adenyl cyclase, for adrenaline hormone, to convert ATP into cAMP which is the secondary messenger to act directly on a protein or initiate a cascade of enzymes |
|
|
Adrenal glands |
Above the kidneys Divided into outer adrenal cortex and inner adrenal medulla Endocrine glands - straight into bloodstream Adrenal cortex produces life essential hormones - steroid hormones to make mRNA that bind to a specific point on DNA Adrenal medulla produces adrenaline and noradrenaline |
|
|
Adrenaline |
Adrenal medulla into the blood to transport Non-steroid hormone so needs secondary messenger and receptor Increase heart rate Raise blood pressure Increase mental awareness Stimulate conversion of glycogen to glucose |
|
|
The pancreas |
Has both exocrine and endocrine functions Small organ below the stomach Pancreatic juices containing enzymes into the small intestine Hormones secreted from the islets of Langerhans into the blood |
|
|
Exocrine function |
Into a duct Most cells in the pancreas synthesise and release digestive enzymes The exocrine cells are in small groups surrounding tiny tubules called acini Acini separated by connective tissue and enzymes made are secreted into the tubule at the centre of the group and the tubules join up to make the pancreatic duct The pancreatic duct secretes enzymes into the small intestine Fluid contains Pancreatic amylase - enzyme for amylose into maltose Trypsinogen - inactive protease to be activated to trypsin Lipase - digest lipid molecules Sodium hydrogencarbonate to make alkali to neutralise the acid as come from stomach |
|
|
Endocrine function |
Islets of Langerhans between the acini Contain alpha and beta cells to make up the endocrine into the blood Alpha cells make glucagon Beta cells make insulin |
|
|
Releasing insulin |
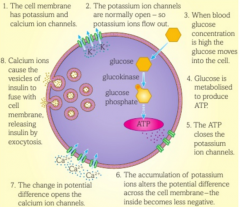
Secreted from beta cells in the islets of Langerhans To reduce blood sugar concentration The cell membrane of the beta cells contains both calcium ion channel and potassium ion channels The potassium ion channels are normally open and the calcium ion channels are normally closed - K+ ions diffuse out of the cell making the inside of the cell more negative at rest the potential difference is -70mV When glucose concentrations outside the cell are high, glucose molecules move into the cell The glucose is quickly used in metabolism to produce ATP which uses the enzyme glucokinase The extra ATP causes the potassium channels to close The potassium can no longer diffuse out and this alters the potential difference across the cell membrane - it becomes less negative The change in potential difference opens the calcium ion channels Calcium ions enter the cell and cause the secretion of insulin by moving vesicles to the cell surface membrane, fuse with it and release insulin by exocytosis |
|
|
Releasing insulin picture |
|
|
|
Blood glucose concentration |
Needs to be carefully regulated Too low then hypoglycaemia where inadequate delivery of glucose to tissues particularly the brain Too high then hyperglycaemia where significant organ damage High continuously then diabetes diagnosis Cells in the islets of Langerhans constantly monitor the concentration of glucose in the blood High glucose release insulin Low glucose release glucagon Act on liver cells |
|
|
Blood glucose rises too high |
High blood glucose is detected by the beta cells in the islets of Langerhans Beta cells secrete insulin into the blood Insulin travels around the body to target cells in the liver and muscles Insulin too large to pass through plasma membrane so attaches to receptor and activates the enzyme tyrosine kinase Tyrosine kinase causes phosphorylation of inactive enzymes in the cell This activates the enzymes to cause a cascade of enzyme-controlled reactions in the cell More transporter proteins for glucose are placed in the cell surface membrane by causing vesicles with the transporter proteins to fuse with the membrane More glucose enters the cell Glucose is converted to glycogen for storage - glycogenesis More glucose is converted to fats More glucose is used in respiration Reduces blood glucose concentrations |
|
|
Blood glucose falls too low |
Low blood glucose concentration is detected by the alpha cells islets of Langerhans Alpha cells secrete glucagon into the blood Glucagon in travels around the body to the target liver cells Glucagon attaches to receptors on the hepatocytes and stimulates a G protein inside the cell This activates the enzyme adenyl cyclase inside each cell Adenyl cyclase converts ATP to cAMP to activate a series of enzyme-controlled reactions inside the cell Glycogen is converted to glucose by glycogenolysis More fatty acids used in respiration Amino acids and fats are converted into additional glucose by gluconeogenesis Increases blood glucose concentrations |
|
|
Negative feedback |
Glucagon and insulin are antagonistic - opposite effects and inhibit the opposing Will fluctuate around a level - not constant |
|
|
Negative feedback glucose loop |

|
|
|
Diabetes mellitus |
A condition where the body is no longer able to produce sufficient insulin to control its blood glucose concentration Lead to prolonged high concentrations of glucose after a meal Concentrations getting too low after exercise or fasting |
|
|
Type 1 diabetes |
Usually starts in childhood Thought to be due to an autoimmune response where immune system attacks beta cells Can’t synthesise sufficient insulin and can’t store excess glucose as glycogen Excess blood glucose isn’t removed quickly When blood glucose concentration falls there is no store of glycogen so concentrations of glucose become too low |
|
|
Type 2 diabetes |
Can produce insulin but not enough As you age your responsiveness to insulin declines Receptors in liver and muscle cells become less responsive Blood glucose concentration is almost permanently raised so damage organs and circulation Factors bring it on such as obesity, lack of exercise, high sugar diet, family history |
|
|
Treating type 1 diabetes |
Insulin injections Monitor blood glucose concentration and then use the correct dose of insulin to keep stable Alternatives include a pump that constantly pumps insulin, islet cell transplant, pancreas transplant Can treat with stem cells to grow new beta cells |
|
|
Treating type 2 diabetes |
Changes in lifestyle Lose weight, exercise regularly, monitor carbohydrate intake Can be supplemented by medication that increase insulin released by the pancreas |
|
|
Source of insulin for treating diabetes |
Used to be extracted from an animal pancreas usually pigs Now genetically modified bacteria to produce human insulin Exact copy of human insulin Less chance of rejection due to an immune response Lower risk of infection Cheaper to manufacture Less moral objections |

