![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
57 Cards in this Set
- Front
- Back
|
Subnormal Hormone Production
|
defects in embyrogenesis (aplasia) defect in enzyme required for hormone synthesis normal gland destroyed by 2o process granulomatous disease, infarction autoimmune disease chemical exposure eg cancer treatment physical damage e.g. surgery tumour |
|
|
Route of Administration
|
Steroid and thyroid hormones can be given orally Gastrointestinal absorption First pass kinetics Peptide hormones require injection (insulin) Depot IM injections (testosterone) Transdermal (gonadal steroids) Intranasal spray / solution / oral (DDAVP) Pumps (insulin) |
|
|
Congenital (anterior) hypopituitarism
|
Neonate presents with hypoglycaemic seizures
- Examination: no excess pigmentation (excludes primary adrenal disease), baby may be quite floppy, drowsy, poor feeding |
|
|
Congenital (anterior) hypopituitarism Tx
|
1.
Start lifelong hydrocortisone replacement • Initially IV • then orally, once feeding established 2. Start lifelong thyroxine (orally) 3. Growth hormone SC (from PBAC) till 13-14yrs 4. At 11-12 years start gonadal hormones • increase over 2yrs to mimic normal puberty • Gonadal replacement lifelong |
|
|
Types of deficiency?
|
Primary: at the endocrine organ Secondary: at the anterior pituitary Tertiary: at the hypothalamus |
|
|
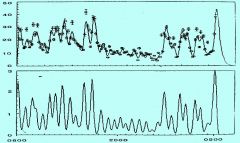
Biorhythms / chronobiology of hormones
|
time-related minutes-hours (LH, testosterone) day (corticosteroids) weeks (menstrual cycle: oestradiol, prog) seasons (thyroxine in hibernation) sleep-associated (early puberty) effects of hormone relate to its half-life insulin vs. IGF1 biological half-life vs. plasma half-life (hard to measure) |
|
|
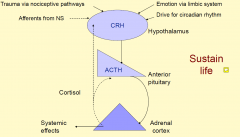
Feedback control of the secretion of cortisol and other glucocorticoids
|
|
|
|
Steroid replacement therapy
|
Glucocorticoids (Cortisol replacement 14 mg/m2/day) - Hydrocortisone (2-4 times a day); 20mg - Cortisone acetate (2 times a day); 25mg - Prednisolone (2 times a day); 5mg - Dexamethasone (once a day); 0.75mg Often lower maintenance doses for pituitary disease: (Cortisol replacement 7-10 mg/m2/day) All need higher dose for severe stress: Hydrocortisone: 100 mg/m2 IMI or IV (Medialert bracelet) |
|
|
Adrenal replacement: adrenal disease
|
Glucocorticoids and mineralocorticoid required Monitor with ACTH (for primary adrenal disease), check for Xs pigmentation, tiredness, easy vomiting Over-replacement causes weight gain, Cushingoid appearance, delay in bone age and short stature |
|
|
Plasma levels and secretion of ACTH
|
|
|
|
Mineralocorticoid replacement (under renin-angiotensin feedback)
|
Mineralocorticoid deficiency: urinary salt loss, low Na, high K (may see peaked T waves on ECG), high PRA Mineralocorticoid replacement (fludrocortisone) - Necessary in primary adrenal disease - Not necessary in pituitary disease - Monitor with plasma renin activity and electrolytes • Blood pressure (if high then too much replacement) |
|
|
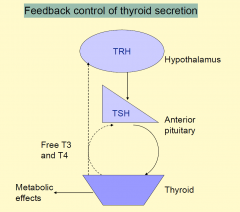
Feedback control of thyroid secretion
|
|
|
|
Thyroid hormone replacement
|
Thyroxine (T4) Long half-life (7-10 days) Oral once per day Liothyronine (T3) rarely used in 2013 Short half-life (hours) 2-3 X per day IV in some circumstances (ICU with monitoring) If longstanding hypothyroidism, start slowly, may aggravate underlying heart disease, untreated cortisol deficiency Usually just omit if vomiting |
|
|
Monitoring Thyroid Hormone Replacement
|
Monitoring
-Well being -Growth -Menses -Constipation / diarrhoea -Neurological development -TSH levels (if 1˚ disease) -Free T4 and free T3 (especially if 2˚ disease) -Bone age (for cong hypothyroidism) |
|
|
Thyroid hormone compliance
|
In congenital hypothyroidism usually excellent (brain development in first 3 yrs) Often poor in adolescents (use TSH as a marker for compliance as it takes longer to come down) Sometimes overdosing / abuse in adults -For weight loss -For increase in energy Side effects of overdosing: -Osteoporosis -Hyperthyroidism (anxiety) |
|
|
Growth hormone deficiency
|
$18,000 pa for Growth hormone Under Federal Government TGA Strict guidelines: -Initiation: height <1st PC, GV <25th PC -Satisfactory response: growth velocity >50th PC Ceased if bone age advanced (epiphyses nearly fused) -13.5yrs for girls -15.5yrs for boys |
|
|
Diabetes Insipidus Presentation
|
10yr old water seeking for 1 year, leaving class to drink and pass urine, nocturia, on awakening drinks from the tap Poor growth, food intake decreased Water deprivation: unable to concentrate urine, hypernatraemic Diagnosis: diabetes insipidus due to ADH deficiency (posterior pituitary) MRI showed a tumour involving hypothalamus (DDx: head injury) |
|
|
ADH replacement
|
DDAVP 100mcg mane, 100mcg mid, 200mcg nocte During vomiting illness unable to tolerate oral Needs intravenous fluids, 6-10L/day low solute Consider IV DDAVP Monitoring the requirement requires -Fluid balance -check osmolality of urine, specific gravity -Check serum electrolytes -weighing |
|
|
Vasopressin deficiency (diabetes insipidus) 1-deamino 8 D arginine vasopressin
|
DDAVP (Minirin) nasally 1-2 times/day; or metered spray or recently orally 3 times/day DDAVP intravenously in ICU: very short acting Monitor with serum sodium, urine output, osmolality (or urinary specific gravity) When unable to tolerate medication patient needs free access to fluid (oral or high IV input of low sodium fluids) |
|
|
Hypoparathyroidism
|
Diagnosis: low calcium and high phosphate Can be due to thyroid surgery Parenteral PTH available under Special Access Scheme, (treatment of osteoporosis, ? Safety) Vitamin D and calcium orally (2-3 times/day) Problems when unable to tolerate oral preparations or irregular absorption |
|
|
Hypoparathyroidism Case
|
4mth old baby presenting with seizures and tetany Hypocalcaemia: Calcium 1.2mmol/l, Phosphate 3.6mmol/l, PTH unrecordable Urgent treatment: intravenous calcium (very toxic to soft tissues) Oral vitamin D, oral calcium (high calcium diet) |
|
|
Hypoparathyroidism: treatment
|
Under-replacement causes hypocalcaemia - Fitting and tetany Over-replacement causes hypercalcaemia - Vomiting and thirst - Nephrocalcinosis Monitor blood levels (Ca, PO4) frequently, also urinary calcium: creatinine ratio Renal ultrasound |
|
|
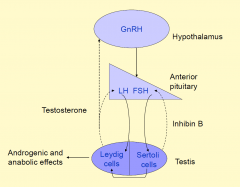
Feedback control of testicular function
|
|
|
|
Aims of pubertal induction therapy
|
mimic natural puberty increase in hormones over 2-3 years normal virilisation / feminisation not to compromise final height achievement of peak bone mass with continuing maintenance of a mineralised bone matrix |
|
|
Timing of pubertal induction
|
12-13 years in girls 13-14 years in boys individualise to maximise final height but prevent body disproportion (from late therapy) minimise the time the adolescent is different from their peers |
|
|
Feedback regulation of ovarian function
|
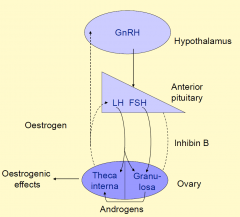
|
|
|
Pubertal induction in girls
|
half a tablet (0.5mg progynova) every second day for 6 mths half a tablet every day for 6 mths one lowest strength tablet daily for 6 mths 1 1/2 lowest strength daily for 6 mths -plus progestagen days 1-10 each months 1 next strength tablet (2mg progynova) daily for 6 mths -plus progestagen for 10-14 days/mth |
|
|
Gonadal replacement in females
|
Combination of oestrogen and progesterone Progesterone given to prevent endometrial hyperplasia cancer risks, hypertension Trisequens (combination, low E2) Oral contraceptive (combination E/P, higher E2) and cheaper Monitor clinically and measure LH (if primary hypogonadism) |
|
|
Pubertal induction in boys 1
|
Andriol (testosterone undecanoate) 40mg
one every second day for 3-6 mths One every day for 6mths one bd for 6mths two mane, one evening for 6 mths two twice daily |
|
|
Pubertal Induction in Boys 2
|
Sustanon (testosterone propionate 20%, phenylpropionate 40%, isocaproate 40%)
50mg a month for 6 mths 100mg a month for 6 mths 150mg a month for 6 mths 200mg a month for 6 mths 250mg a month for 6 mths 250mg every 2-3 weeks |
|
|
Hypogonadism in males
|
Testosterone esters every 2-3 weeks Long acting testosterone undecanoate every 12-14 week, every 6 weeks initially authority required monitoring of trough and peak values of T Over-replacement causes - Aggression - Painful prolonged erections Under-replacement - Low bone mineral density - Reduced strength - Decreased libido Clinical assessment and LH levels (if primary hypogonadism) |
|
|
Replacement hormones
|
no prolactin releasing hormone just DA the inhibitory (thus the only hormone to be tonically inhiited)
|
|
|
Principles of Endocrinology
|
1. Negative Feedback
- basal state - related hormones often exist - hormonal secretion patterns vary 2. Dynamic Testing Possible hormone excess - SUPPRESSION TEST Possible hormone lack - STIMULATION TEST |
|
|
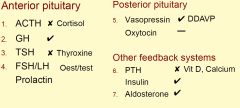
Endocrine Investigation 1
|
|
|
|
Endocrine Ix 2
|
|
|
|
Things to consider
|
› Time
- Day - Cycle › Fed/Fasting › Half Life › Pregnancy |
|
|
Circadian Rhythms
|
› Cortisol (& ACTH) - higher at night
› (Vasopressin) - higher at night › TSH › Testosterone › LH, FSH in adolescent › (GH) after exercise and in stage 3-4 sleep |
|
|
Growth Hormone Axis
|
› GH
- Pituitary - Short half life - Variable serum levels - Not worth measuring in deficiency states! › IGF-I - Many tissues - Longer half life (hrs) - Stable levels - Binding proteins - Second messenger - GH - Nutrition |
|
|
Stimulation tests
|
› Pituitary
- “Multiple Pituitary Stimulation” - GnRH - TRH - Hypoglycaemia - (CRH) - Metabolic - Hypoglycaemia - Amino acids (arginine stimulation for GH) › Exercise › Drugs - Clonidine - Metoclopramide - Propranolol › Sleep › Stress |
|
|
Pituitary Inhibitory Tests
|
- Hormonal
- Somatostatin - Nutritional & metabolic - Oral glucose tolerance test (OGTT) - Drugs - Bromocriptine |
|
|
Other Endocrine Testing
|
STIMULATION
› Adrenal - SynACTHen - ITT › Gonads - GnRHs INHIBITION › Adrenal - Dexamethasone Suppression › Gonads - Hormone Replacement |
|
|
Local Investigations
|
› Pituitary
- Visual fields - Xray - CT/MRI › Adrenal - CT/MRI › Thyroid - Ultrasound - Tc Scan & Uptake - FNAB (biopsy) › Gonads - Ultrasound - CT or MRI Scans |
|
|
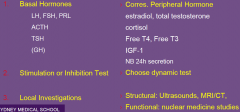
Growth Investigations (EG SHORT CHILD)
|
› Basal Hormones
› Stimulation test - MPS (hypoglycaemia) - Arginine - Propranolol - Clonidine - Exercise › Local Investigations - Scan › “Disease” produced - Bone Age › Associated disease - Asthma - Renal › General - Haematology - Nutrition |
|
|
Short Stature
|
› Constitutional
› Intercurrent Disease - Malabsorption - Inflam Bowel disease - Renal - Respiratory › Nutritional › Emotional Deprivation › “Small for dates” › Skeletal Dysplasia › Chromosomal abnormalities - Turners › Dysmorphic Dwarfism › Endocrine causes - Hypothyroidism - CAH - Growth hormone deficiency |
|
|
Congenital Adrenal Hyperplasia (CAH)
|
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive diseases resulting from mutations of genes for enzymes mediating the biochemical steps of production of cortisol from cholesterol by the adrenal glands (steroidogenesis).
|
|
|
Elevated Blood Prolactin
|
› Tumour
- Prolactinoma: - Secondary to pressure › Stalk section › Drugs - Antipsychotics - Opiates - Reserpine - metoclopramide › Diseases - Renal - Primary Hypothyroid (TRH can increase prolactin) › Pregnancy › Exercise ++ › Local Stimulation |
|
|
DDx Prolactin producing tumours
|
DDx between these 2
- prolactinomas prolaction; 3-10x normal - secondary, non-secretory tumours; only 1-5-2 folds |
|
|
Cushing’s Syndrome Dx
|
› Determine (i) if it is present, then (ii) the primary organ
(i) Syndrome confirmed › Basal Hormone (?when) - cortisol › 24 h Urinary free cortisol › Dexamethasone Suppression Test - Screening 1 mg test (ii) primary organ implicated in causing the syndrome › ACTH level (detectable or not?) › Dexamethasone Suppression Test - Low dose - High dose › Local imaging - CT/MRI head or adrenals - (visual fields) - (Inferior petrosal sinus sampling) |
|
|
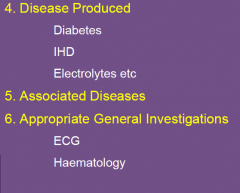
Cushing Complications
|
› Diseases produced
- Diabetes - Osteoporosis › Associated diseases - ECG - Cardiac › General |
|
|
Thyroid Axis
|

T3 10x active and also in its negative feedback strength
|
|
|
Thyroid Investigations
|
› Hormones
- TSH - Free T4, Free T3 › Antibodies - TRAb - Anti-TPO - Anti-Thyroglobulin › Thyroglobulin levels › Imaging - Ultrasound - Scan & Uptake - Technetium uptake - Perchlorate discharge - (MRI/CT) › Fine needle biopsy |
|
|
Thyroid Adenomas and Toxic Multi-nodular goitres
|

- cancer as cold spots on thyroid scans (non-functional)
|
|
|
Meningoccoccal, DIT and Adrenals
|
bleed into the adrenal
waterhouse .... syndrome - need extra cortisone in this state |
|
|
Commenest cause of hypoadrenalism world-wide
|
TB
|
|
|
Adrenal Cortex Hormone Synthesis
|

|
|
|
Adrenal Masses
|
› May be hypersecreting
- Phaeochomocytoma (adrenal medulla) - Conn’s syndrome (primary hyperaldosteronism) - Cushing’s syndrome - Androgen over-secreting (eg DHEA; testosterone) › May be non-functioning - If generalised may cause Addison’s disease |
|
|
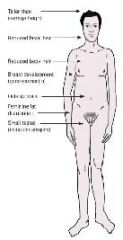
Primary hypogonadism
Genetic sex hormone deficiency -Male |
|

