![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
86 Cards in this Set
- Front
- Back
- 3rd side (hint)
|

|
|
|
|
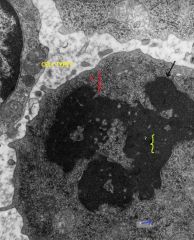
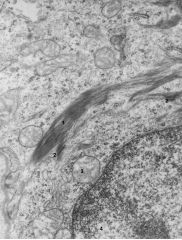
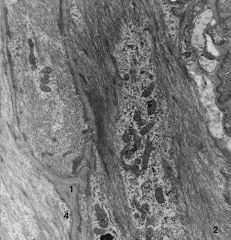
The nucleus is located at the lower right hand side of the micrograph. Dense chromatin ([MARGINAL] heterochromatin)(1) is distributed along the nuclear side of the nuclear envelope except in regions of the nuclear pores (2).
x 63,525 3 = Euchromatin 4 = Smooth Endoplasmic Reticulum 5 = Golgi Body 6 7 Desmosomes with attachment plate 8 keratin 9 mitochondria 9 |
|
|

|
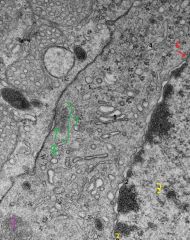
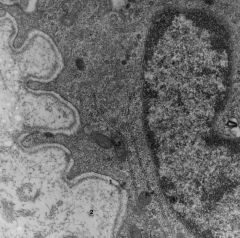
Pinocytosis in an endothelial cell. The vessel lumen is to the upper right and the underlying connective tissue is to the lower left. Note the thin gray (electron dense) line of the basal lamina immediately below the cell. There are several unlabeled vesicles forming at the luminal surface of the cell.
1 = Vesicles open to the outside of the cell facing the extracelluar matrix. 2 = Partially enclosed vesicle just inside the plasma 3 = Vesicle completely contained within the cytoplasm of the cell |
|
|
|
|
|
|
|

|
|
|
|

|

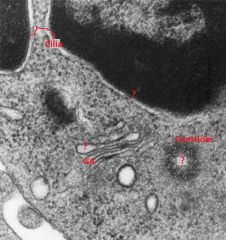
Part of a cell showing a centriole (C) cut transversely. Note the triplet arrangement of microtubules cut in cross-section.
x 115,920 GA = Golgi Apparatus (Body) PR = Polyribosomes (Polysomes) NS = Perinuclear Space (of the nuclear envelope) |
|
|

|
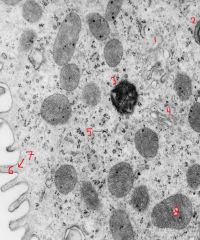
Rough endoplasmic reticulum arranged in stacks in a pituitary cell. Ribosmes (arrows) are associated with the membrane of the endoplasmic reticulum.
x 92,800 1 = Mitochondrion 2 = Secretory Granule |
|
|
|
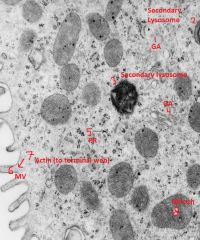
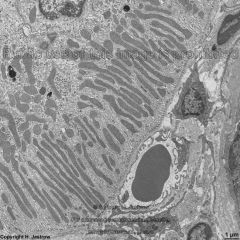
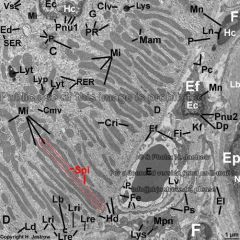
Cytoplasmic organelles of a renal collecting duct cell.
x 50,240 TL = Tubular Lumen MV = Microvilli on cell surface M = Mitochondrion PR = Polyribosomes (Polysomes) GA = Golgi Apparatus (body) IS = Intercellular Space; note the interdigitations of the cell membranes are between the two cells. (lower right) Although not labeled, note (at the lower right of the micrograph) that there is a thin gray line of the basal lamina just external to the cell membrane. |
|
|
|
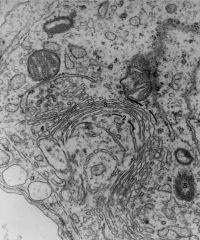
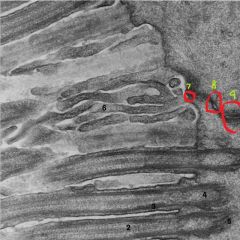
Detail of Golgi Apparatus (body)
x 55,000 1 = Cis, forming, convex face 2 = Trans, maturing, concave face 3 = Saccules 4 = Vesicles budding from saccules 5 = Centrioles |
|
|

|
Detail of Golgi Apparatus (body)
x 55,000 1 = Cis, forming, convex face 2 = Trans, maturing, concave face 3 = Saccules 4 = Vesicles budding from saccules 5 = Centrioles |
|
|
|
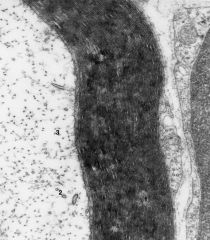
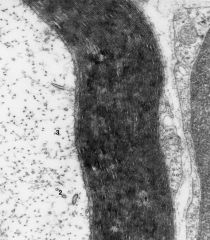
High magnification of myelin sheath (1) Surrounding a nerve fiber in a peripheral nerve. Within the fiber can be seen:
2 = Microtubules 3 = Neurofilaments. Such a nerve fiber might be either an AXON of a multipolar motor neuron or the DENDRITE of a sensory pseudounipolar neuron. x 102,400 |
|
|
|
High magnification of myelin sheath (1) Surrounding a nerve fiber in a peripheral nerve. Within the fiber can be seen:
2 = Microtubules 3 = Neurofilaments. Such a nerve fiber might be either an AXON of a multipolar motor neuron or the DENDRITE of a sensory pseudounipolar neuron. x 102,400 |
|
|
|
Epithelial cells showing a large bundle of tonofilaments (1) in one of them.
2 = Desmosomes along the opposing cell membrances of two cells 3 = Mitochondrion 4 = Nucleus of the lower cell x 57,050 |
|
|
|
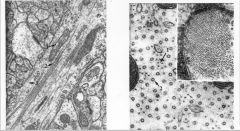
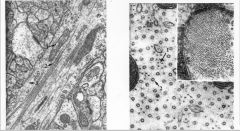
#4 Longitudional Segment of Initial Axon Segment
(x 75,000) Prominent features include: A. Scattered Ribosomes B. Fascicles of Microtubules C. Mitochondria D. Occasional Neurofilaments #5 - Microtubules, Neurofilaments and Neuroglial Filaments (x 211,000) The inset at the upper right shows bundles of cytoplasmic filaments in an astrocyte. The remainder of the figure is a transverse section through a dendrite of an anterior horn cell. The cytoplasm contains abundant microtubules and neurofilaments. |
|
|
|
#4 Longitudional Segment of Initial Axon Segment
(x 75,000) Prominent features include: A. Scattered Ribosomes B. Fascicles of Microtubules C. Mitochondria D. Occasional Neurofilaments #5 - Microtubules, Neurofilaments and Neuroglial Filaments (x 211,000) The inset at the upper right shows bundles of cytoplasmic filaments in an astrocyte. The remainder of the figure is a transverse section through a dendrite of an anterior horn cell. The cytoplasm contains abundant microtubules and neurofilaments. |
|
|
|
Apical Region of Epithelial cells, showing Cilia cut longitudinally.
x 71,400 1 = Cell Membrane 2 = Central Microtubules 3 = Peripheral Microtubules 4 = Basal Body 5 = Rootlets The Densities of some cell junctions can be seen in the upper right quadrant of the photo, along the cell membranes of the two opposing cells. 6 = Microvilli, for comparison of size with cilia 7 is a tight junction (claudins and occludins) 8 is an intermediate junction (with connections to terminal web) cadherins and catenins link to actin 9 is a desmosome (macula adherens) with Keratin and desmosomal attachment plaque desmoglein and desmocollin --all three make up a terminal bar |
|
|
|
Several longitudinally cut smooth muscle cells from an intra-renal artery. Each cell is surrounded by a gray basal lamina(l).
2 - Myofilaments (mainly actin), often attached to electron dense plaques. The "hairy" look is typical of smooth muscle. 3 - Mitochondria 4 - Pinocytotic vesicles along plasma membrane. These, too, are typical of smooth muscle. X 23,550 |
|
|
|
Basal Lamina (1) of Epithelial cell
2 = Reticular fibrils in ground substance. A condensation of this area just deep to the basal lamina contributes to the "basement membrane" often seen in light microscropy. 3 = Mitochondrion x 52,000 |
|
|
|
|
|
|
|
|
|
|
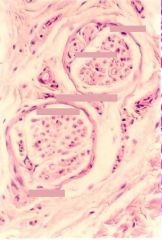
What is this? Where else found?
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|

|
|
|
|
|
|
|
|
|
|
|
|
|
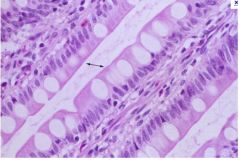
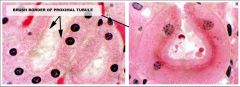
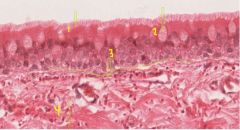
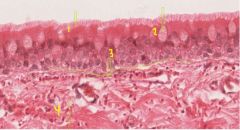
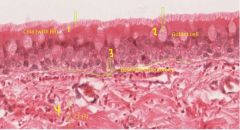
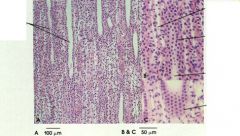
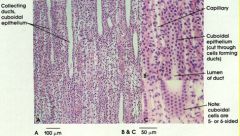
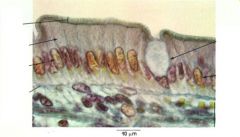
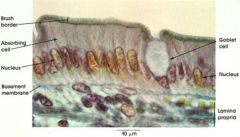
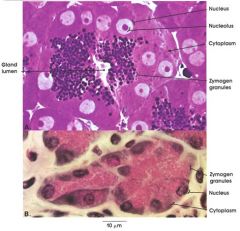
Absorbing cell: Single cell layer of tall columnar cells. Basal ovoid nucleus. Although the cells appear retangular in this section, they are actually five- or six-sided when they are cross-sectioned. When the underlying tissue folds or bends, these cells may have a pyramidal appearance.
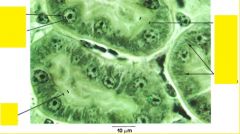
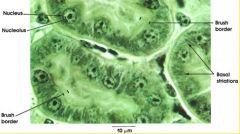
Nucleus: Ovoid. Situated in lower half of the columnar cell. The nuclei in tightly packed cells may appear elongated and staggered at different levels within the cell. This is readily seen in pseudostratified ciliated columnar (see Plate 19). Brush border: Also know as the straited border. Made up of fine, closely packed microvilli that vastly increase the surface area of the cell. Characteristic of absorptive surfaces. Adequate absorption of digestive products is dependent upon this cell surface specialization of absorbing columnar epithelial cells. Goblet cell: Unicellular mucous glands scattered among the tall columnar cells appear empty because mucin is extracted during tissue processing. See Plate 20 for goblet cell mucus. These unicellular gland cells are a specialization of simple epithelium and serve a protective function for the principal epithelial cell type. Basement membrane: Delicate in appearance but a firm support for the columnar cells. See also Plate 20. Lamina propria: Connective tissue stroma. Reticular framework containing a.variety of wandering cells as well as vascular and lymphatic channels. Cells commonly found in the lamina propria |
|

|

|
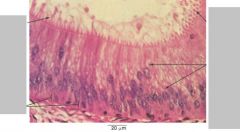
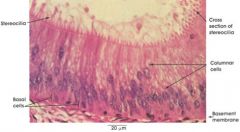
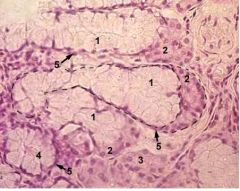
The epididymal duct is lined by a pseudostratified columnar epithelium containing two types of cells: tall columnar cells bearing so-called stereocilia and rounded basal cells. The cells forming a pseudostratified epithelium deceptively appear to be stratified in two or more layers. The cells actually vary in height, but all are in contact with the basement membrane.
Columnar cells: Tall cells bearing stereocilia. These are non-motile processes of the columnar cells projecting into the lumen. Although they are called cilia, electron micrographs show that they lack the structural characteristics of cilia, and they resemble greatly elongated microvilli. In this figure, they are seen in both cross and longitudinal section. Nuclei of columnar cells are elongated and lie at different levels. Basal cells: Rounded or triangular cells, lying against the basement membrane, form a discontinous layer around the duct. |
|

|

|
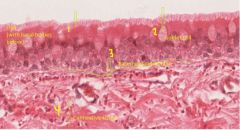
Epithelium: Pseudostratified ciliated columnar epithelium. The term pseudostratified refers to the appearance of the epithelium in section. Although the cells appear to be stratified because the nuclei are found in several layers, the basal portions of all cells are actually in contact with the basement membrane.
Cilia: These motile structures carry a carpet of mucus, provided by goblet cells, which collects inhaled debris and takes it to the pharynx where it is either coughed out or swallowed. Goblet cells: These non-ciliated mucus-secreting cells are seen in various stages of mucous synthesis and discharge. Basement membrane: This common structure is thickest in the trachea, but wandering cells of the immune system can be found traversing the membrane. Other cells of the immune system are also seen at various levels of the epithelium. Lamina propria: The lamina propria of the trachea is thin but contains small blood vessels and collagenous and elastic fibers. |
|
|
|
|
|

|

|
|
|
|
|
|
|
|
|
|
|
|
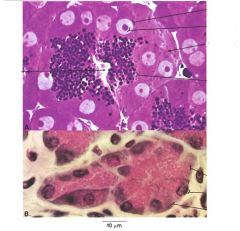
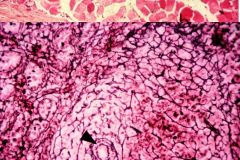
SUBLINGUAL SALIVARY GLAND
Stained with haematoxylin and eosin 1 - mucous part of mixed secretory unit 2 - serous part (serous demilune) of mixed secretory unit 3 - serous secretory unit 4 - mucous secretory unit 5 - myoepithelial cells |
|
|
|
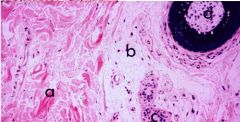
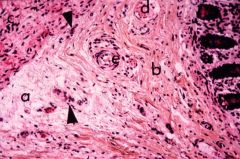
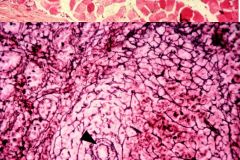
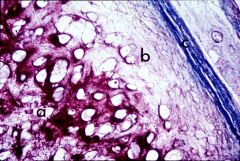
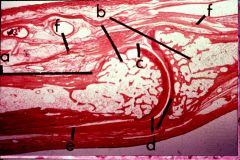
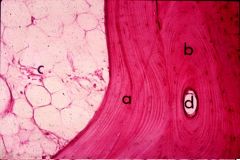
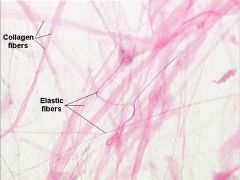
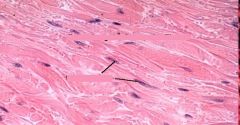
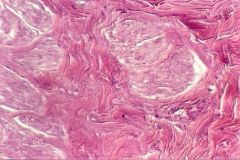
Collagen fibers represent the principal type of fiber in the connective tissues of the body. Microscopically, these fibers appear as individual strands or bundles which stain acidophilically. In the skin, collagen fibers are arranged irregularly and in thick bundles as in the dense irregular connective tissue of the pars reticularis (a) while in the loose irregular connective tissue, which is continuous with the pars papillaris (b) which surrounds the sweat glands (c) and hair follicles (d), the collagen fibers are smaller and less numerous. Thus, these two forms of irregular connective tissue are distinguished on the basis of the relative number of collagen fibers and the thickness of the fiber bundles. Human skin. Hematoxylin and eosin stain
|
|
|
|
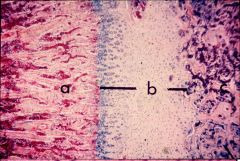
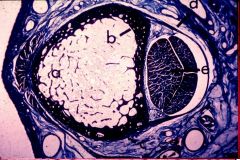
In the areolar or loose irregular connective tissue (a) the collagen fibers are fine and the loose arrangement of these fibers permits the visualization of the intercellular or ground substance (light spaces between the collagen fibers). In the dense irregular connective tissue (b) the collagen fibers are thick and more tightly packed, tending to obscure the ground substance. Sharp distinctions between these two forms of fibrous connective tissue are not always possible. Irregular connective tissues are associated with smooth muscle (c), small nerves (arrows), small veins (d) and arteries (e) shown in this photomicrograph. Human colon. Quad stain.
|
|
|
|
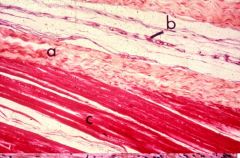
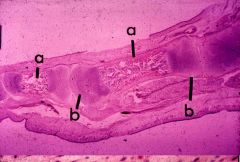
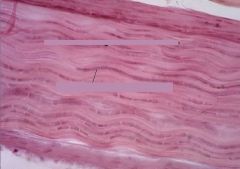
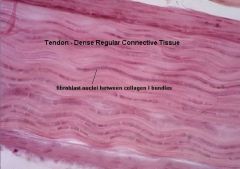
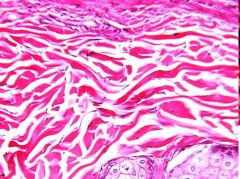
n dense regular fibrous connective tissue collagen fibers are arranged parallel to one another. In the tendon, collagen fibers form compact bundles (a) which are separated by small areas of loose fibers and small blood vessels (b). The junction between the tendon and skeletal muscle (c) can be distinguished. Human muscle-tendon junction. Quad stain.
|
|
|
Ephedrine
[Trade Name] |
Ephedrine
|
|
|
Sodium Nitroprusside
[Trade Name] |
Sodium Nitroprusside
|
|
|
|
Reticular fibers are found principally in the blood-forming organs (e.g., bone marrow, spleen and lymph nodes). In these tissues the reticular fibers form networks and tend to surround structures such as blood vessels (arrow). Reticular fibers can be demonstrated only by selective staining procedures. They appear as fine dark lines in this preparation. Human spleen. Silver stain.
|
|
|
|
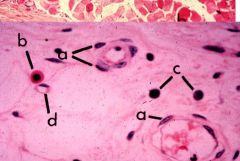
Also present in connective tissue are the adventitial or perivascular cells (a) located along the wall of small blood vessels. Mast cells (b) which are characterized by their granular, acidophilic cytoplasm also are frequently found along capillaries (d). Plasma cells (c) are similar in size and shape to mast cells but have a more eccentrically located nucleus and basophilic cytoplasm. Human connective tissue. Hematoxylin and eosin stain
|
|
|
|
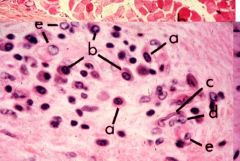
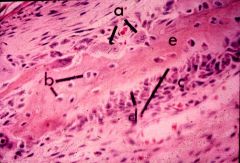
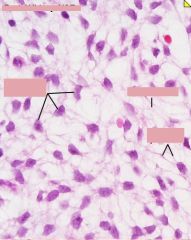
In areas of slight inflammation many different cells can be seen: mast cell (a), plasma cells (b), fibroblast (c), smooth muscle cells of the arteriole (d) and endothelial cells (e). Human connective tissue. Hematoxylin and eosin stain
|
|
|
|
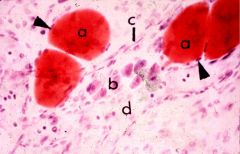
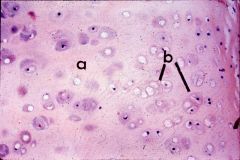
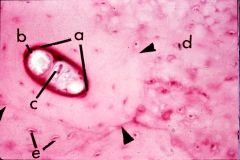
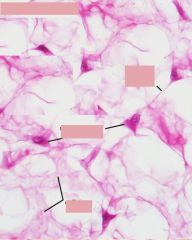
Intracellular fat can be demonstrated if lipid solvents are avoided and special stains are used. The lipid (a) occupies almost all of the cytoplasm and forces the nucleus (arrow) to the periphery of the cell. In many areas fat cells and mast cells (b) are associated with small vessels such as capillaries (c) and lymphatics (d). Rat mesenteric spread. Oil red O and methylene blue stain.
|
|
|

|
Ground substance is present in all connective tissues to some degree but it is very difficult to demonstrate because of its amorphous character. In this slide the ground substance appears as a nearly homogenous pale-staining matrix in which the darker-staining fibers, fibroblasts (a). a mast cell (c) and small vessels (b), are embedded. Human connective tissue. Azan stain
|
|
|
|
LOOSE CONNECTIVE TISSUE
Stained with iron haematoxylin 1 - fibroblasts 2 - collagen fibers 3 - elastin fibers |
|
|
|
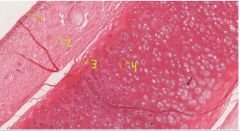
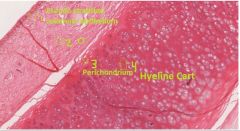
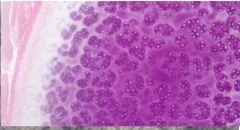
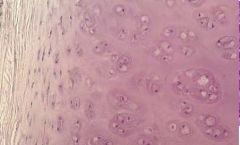
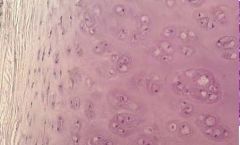
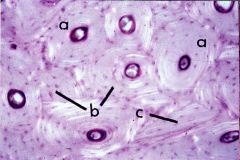
HYALINE CARTILAGE
Stained with haematoxylin and eosin 1 - cells of the cartilage (chondrocytes, chondroblasts) 2 - intercellular cartilage matrix 3 - perichondrium |
|
|

|
HYALINE CARTILAGE
Stained with haematoxylin and eosin 1 - cells of the cartilage (chondrocytes, chondroblasts) 2 - intercellular cartilage matrix 3 - perichondrium |
|
|
|
HYALINE CARTILAGE
Stained with haematoxylin and eosin 1 - cells of the cartilage (chondrocytes, chondroblasts) 2 - intercellular cartilage matrix 3 - perichondrium |
|
|
|
ELASTIC CARTILAGE
Stained with iron haematoxylin 1 - cells of the cartilage (chondrocytes, chondroblasts) 2 - intercellular cartilage matrix 3 - perichondrium |
|
|
|
ELASTIC CARTILAGE
Stained with iron haematoxylin 1 - cells of the cartilage (chondrocytes, chondroblasts) 2 - intercellular cartilage matrix |
|
|
|
Elastic cartilage superficially resembles hyaline cartilage when stained with routine histological stains. However, when it is stained specifically to demonstrate elastic fibers marked differences between the two tissues are evident. The brown-staining elastic fibers are most numerous in the matrix of the mature cartilage (a) although they also are present in the chondrogenic (b) layer of the perichondrium and mixed with the green-staining collagen fibers in the fibrous perichondrium (c). Human epiglottis. Orcein stain.
|
|
|
|
Hyaline cartilage is the most common of the three types of cartilage found in man. It is characterized by a homogenous-appearing matrix (a) containing scattered cells, chondrocytes, which may exist singly or in isogenous groups (b). The groups of cells are formed by division of a single chondrocyte which results in interstitial growth of the cartilage. Each chondrocyte is located within a lacuna; its nucleus is usually visible as is a large cytoplasmic vacuole which, in life, is usually filled with glycogen. The newly formed matrix immediately around each lacuna is slightly more basophilic than the older interlacunar matrix. Human trachea. Hematoxylin and eosin stain.
|
|
|
|
Fibrocartilage appears to be a transition between dense collagenous connective tissue and hyaline cartilage and is limited in its distribution. Transition between cartilage and connective tissue is visible from one side of this slide to the other. Note the relative amount of fibers and matrix as well as the cell arrangement. This tissue is characterized by isogenous groups of chondrocytes (arrows) scattered among bundles of collagen fibers; the matrix is visible only close to the chondrocytes. Fibrocartilage does not possess a clearly definable perichondrium. Mammal pubic symphysis. Hematoxylin and eosin stain.
|
|
|
|
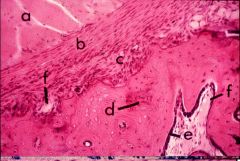
ones, as organs, are composed of several tissues. Osseous or bony tissue is the main structural component and exists in two configurations. As compact bone it forms the external shell of the organ and in long bones it makes up the entire wall of the diaphysis (a). Spongy or cancellous bone (b) forms a lightweight web of supporting trabeculae and, in long bones, it occupies the metaphysis and epiphysis. The osseous tissue is covered by a specialized connective tissue layer, the periosteum (e), which, at joints, is continuous with the dense connective tissue of the joint capsule (f). The articular surfaces of the joint are covered by hyaline cartilage (d). Synovial membranes which line the non-articular surfaces within the joint cavity may project inward as folds (c); they secrete the synovial fluid necessary for smooth action of the joint. Human finger. Hematoxylin and eosin stain.
|
|
|
|
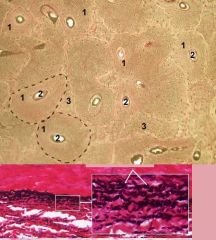
Compact bone is, for the most part, made of units called osteons or haversian systems (a). Each osteon is a cylindrical structure composed of many concentric layers or lamellae of osseous tissue in which the fibers are spirally oriented and easily demonstrated with polarized light. Bones continue to change their shape throughout life, chiefly in response to mechanical stress. Evidence of these changes is manifested by the presence of complete osteons (a) superimposed on partial osteons (b) and fragments of interstitial lamellae (c) which they have replaced. Human humerus. Hematoxylin and eosin stain. Polarized light.
|
|
|
|
The typical osteon (arrows) is composed of concentric lamellae arranged around a canal (a) which contains both blood vessels (b) and nerves (c) along with a few connective tissue fibers and cells. Areas of woven bone (d) which are not arranged in lamellae occupy the space between many of the osteons. Osteocytes (e), each within its own lacuna, appear between the lamellae in the woven bone. Human humerus. Hematoxylin and eosin stain.
|
|
|
|
In osteogenesis, small masses of osseous tissue are formed by secretion of an uncalcified ground substance, osteoid (d), by osteoblasts (c). The osteoblasts move outward depositing osteoid behind them; as the mass of osteoid enlarges, a few osteoblasts are trapped by the forming tissue and become osteocytes (b). The osteoid soon calcifies to become bone (e). As the mechanical stresses change in response to growth, osseous tissue is removed by osteoclasts (a) and the bone changes shape. Human fetus, calvarium. Hematoxylin and eosin stain.
|
|
|
|
During embryonic development, most bones, except for those of the face and vault of the skull, are formed by the replacement of preexisting cartilage models. The midportion of the model is replaced by the formation of a primary center of ossification (a) while the epiphysis of the model (b) continues to form as cartilage for some time. Human fetus, foot. Hematoxylin and eosin stain.
|
|
|
|
As embryonic development continues, the primary center of ossification in the diaphysis expands to incorporate the metaphysis (a). Simultaneously a secondary center of ossification is established in the epiphysis (c). The small mass of cartilage that remains between these centers of ossification is the epiphyseal plate (b) and hereafter is the only point at which the bone can increase in length. Human fetus, knee. Ouad stain.
HUMAN FETUS KNEE |
|
|
|
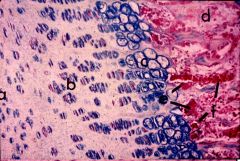
The epiphyseal plate may be divided into zones on the basis of changes in morphology of its chondrocytes. Closest to the secondary center of ossification is a zone of resting or reserve cartilage (a). Deeper in the plate, the chondrocytes are undergoing mitosis and forming typical isogenous groups; this is the zone of proliferation or multiplication (b). Closer to the metaphysis is the zone of hypertrophic cartilage (c) in which the chondrocytes and their lacunae begin to enlarge because of changes in their nutritional status. At the point of contact between the epiphyseal plate and the metaphysis a thin zone of calcified cartilage (d) is rapidly eroded away by osteoclasts (e) as invading capillaries (f) push forward bringing cells which will transform into osteoblasts. Human fetus, knee. Quad stain.
|
|
|
|
As bones continue to grow, their walls thicken. New bone is deposited on the outer surface by the osteoblasts in the osteogenic layer of the periosteum (c) while the fibrous layer of the periosteum (b) serves as the attachment site for muscle fibers (a). A layer of osteoblasts lining the marrow cavity, the endosteum (e), deposits tissue on the inner surface of the shaft. Spicules of calcified cartilage (d) may be incorporated into the forming bone; they are eventually removed during remodeling. Closely associated blood vessels (f) will eventually be surrounded by developing bone and thus become the vessels of the haversian systems. Mammal pubic symphysis. Hematoxylin and eosin stain.
|
|
|
|
In an adult bone, the circumferential lamellae (a) which were deposited by the endosteum (or periosteum) are arranged more or less parallel to the free surface of the bone in contrast to their concentric arrangement (b) around a central canal (d) in a typical osteon. In most bones of the adult the space within the shaft is occupied by yellow or fatty marrow (c). Human mandible. Hematoxylin and eosin stain.
|
|
|
|
The final product of bone growth results in a fully formed organ, a bone. Its outer shell is dense or compact bone tissue (b). The center of the bone is occupied by thin sheets of the same tissue, spongy bone (a) and marrow, a tissue related to bone only topographically. The outer surface of the bone is covered by a fibrous layer, the periosteum (c), which is continuous with the walls of joint capsules, and synovial tunnels (d) through which the tendons (e) pass. Human metacarpal. Azan stain.
|
|
|
|
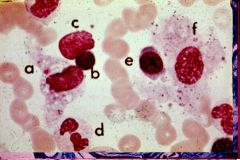
reticular cell (f) which provides the basic cellular stroma of the bone marrow is occasionally found in smear preparations and can be compared with a macrophage (a) which contains some phagocytized cellular debris in its cytoplasm. Other cells include a lymphocyte (b), an early normoblast or polychromatophilic erythroblast (e), a mature neutrophil (d) and a damaged cell (c) with distorted nucleus and no cytoplasm. Human bone marrow.
|
|
|
|
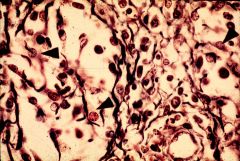
Lymphocytic organs have a basic composition of reticular cells, reticular fibers and lymphocytes. Reticular fibers selectively stained (brown-black) and reticular cells (arrows) are arranged in loose networks. Lymphocytes are scattered randomly within this cellular and fibrous stroma or, as will be noted in succeeding slides, may be collected in dense compact masses or in organized nodules. Reticular cells are stellate in contour with abundant but ill-defined cytoplasm and oval nuclei. Reticular cells may be intimately associated with the reticular fibers. Human lymph node. Silver reticulum stain with fast green counterstain.
|
|
|
|
elastic c.t.
|
|
|
|

|
|
|

|
|
|
|
|
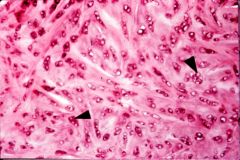
The myocardium is composed of branching bundles of spirally arranged cardiac muscle fibers separated by small amounts of connective tissue, perimysium, containing numerous blood vessels. Human heart. Masson stain.
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|
|
|

|
|
|
|
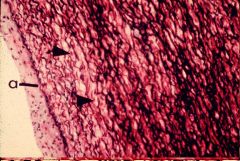
In your slide, find the reticular layer of the dermis. The following photograph shows reticular dermis with elastic fibers (specially stained dark). This is dense, irregular connective tissue.
|
|
|
|
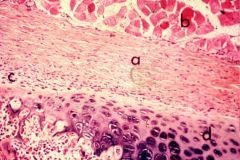
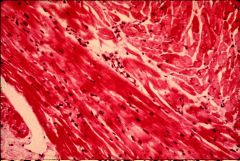
This section is through the dermis of the skin over the nipple of the breast. There are bundles of smooth muscle (lighter staining) running in the dense pink stained connective tissue. Be able to find these on your slide 79.
|
|
|
|

|
|
|
|
|
|
|
|
|
|
|
|
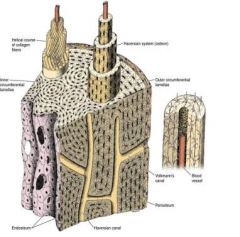
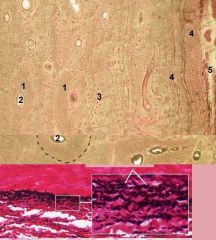
LAMELLAR (MATURE) BONE
Stained with thionin and picric acid 1 - Haversian system (for better understanding, two Haversian systems are bordered with dotted line) 2 - Haversian canal 3 - interstitial system (older, partially resorbed, Haversian system) |
|
|
|
LAMELLAR (MATURE) BONE
Stained with thionin and picric acid 1 - Haversian system (osteon) 2 - Haversian canal 3 - interstitial system (older, partially resorbed, Haversian system) 4 - outer cortical lamellae (cortical bone) 5 - periosteum |
|
|
|
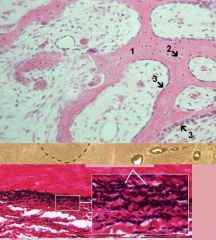
WOVEN (IMMATURE) BONE
Stained with haematoxylin and eosin 1 - intercellular bone matrix 2 - osteocytes 3 - periosteum |
|
|
|
WOVEN (IMMATURE) BONE
Stained with haematoxylin and eosin 1 - intercellular bone matrix 2 - osteocytes 3 - periosteum 4 - osteoclast |
|
|
|
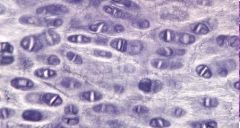
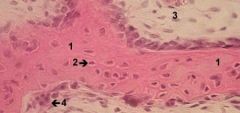
Slide 254/ileum/20x
Observe the parasympathetic ganglion nerve cell here. They can be identified by their pale staining nucleus and promininet nucleoli |
|
|
|
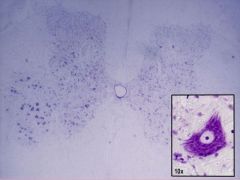
Slide 163/spinal cord/1x
Identify motoneurons found in the ventral horn of the spinal cord. Inset is a higher magnification of a motoneuron. Once again, notice how Nissl Substance is not found in the axon hillock. |
|
|
|
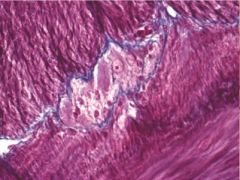
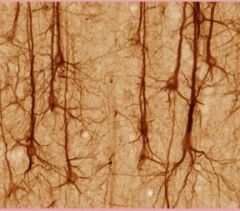
pyramidal cells
|
|

