![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
location of esophagus
|
extends from the oropharynx to the stomach, has 3 parts: upper, middle and lower thirds.
|
|
|
where are mucous glands in the esophagus
|
Mucous glands are present in the submucosa of all regions, but only the upper and lower 1/3rds have mucous glands in the lamina propria
|
|
|
muscularis externa in the esophagus
|
upper 1/3, a continuation of the pharynx, is skeletal muscle. The lower 1/3, continuation of the stomach, is composed of smooth muscle. The middle 1/3 is a blending of the 2 varieties of muscles.
|
|
|
component that guide to identifying esophagus
|
muscularis externa
|
|
|
Characteristics of mucosal epithelium, muscularis externa, adventitia.
|
mucosal epithlium: muscularis mucosa and lamina propria.
muscularis externa: circular and longitudinal smooth muscle. adventitia: fibroelastic connective tissue that binds the esophagus to adjoining structure |
|
|
types of epithelium of esophagus
|
stratified squamous epithelium (non-keratinizing)
|
|
|
features of esophagogastric junction
|
1. abrupt change from stratified squamous epithelium (esophagus) to the simple columnar, mucus secreting epithelium (stomach)
2. presence of mucosal glands (cardiac glands) in the terminal esophagus (located in the submucosa in the rest of the esophagus) |
|
|
3 regions of stomach
|
cardiac, fundic body and pylorus
|
|
|
cardiac stomach is recognized by? fundus body of the stomach is recognized by?
|
Cardiac stomach is recognized by pure mucous gastric glands. The fundus body of the stomach is recognized by fundic glands, which is continuous with gastric pits.
|
|
|
rugae of the stomach is made of what 2 structural layer?
|
regae are made of mucosa and submucosa.
|
|
|
Grooves that subdivide the mucosal surface of stomach into slightly bulding gastric area
|
mammillated area
|
|
|
Cells that protect the lining of stomach from the gastric juices
|
mucous cells
|
|
|
Pepsinogen are secreted by?
|
Chief cells
|
|
|
HCl and intrinsic factor (essential for Vit B12 absorption) are secreted by?
|
parietal cells
|
|
|
Function HCl in the stomach?
|
HCl activates the pepsinogen secreted by the chief cells into pepsin.
|
|
|
Structure of pyloric junction (sphincter)
|
1. thickening of the circular layer of the muscularis externa, which forms the pyloric sphincter
2. columnar enterocytes (absorptive cells) are present on the surface of the villus protrusions 3. Glnds of Brunner, neutralize the acidic chyme) |
|
|
Function of the pyloric sphincter
|
controls the passage of the chyme from the stomach into the duodenum
|
|
|
Function of the duodenum
|
1. receives digested bolus from the stomach
2. receives digestive enzymes from the stomach, pancreas and liver 3. secretes an alkaline mucus to neutralize the acidic chyme |
|
|
structure of the duodenum
|
1. 25cm in length
2. enterocytes is the main cells of the epithelial layer 3. goblet cell: secret mucus 4. Paneth cell line the intestinal crypt of Lieberkuhn 5. Brunner's glands |
|
|
Function of the jejunum
|
1. chemical breakdown of the food chyme
2. absorption |
|
|
structure of the jejunum
|
1. 2.5m in length
2. plicae circulares are the most numerous in the proximal part and morm most of the submucosa 3. goblet cell 4. paneth cell line the intestinal crypts of lieberkuhn 5. brunner's glands are absent |
|
|
Paneth cells functions in?
|
host defense, and they are next to stem cells
|
|
|
Function of ileum
|
1. absorption of Vit B12 and bile salts, things not absorbed by the jejunum
|
|
|
Structure of ileum
|
1. 3.5m in length (longest of the small intestine)
2. the plicae circulares are smaller and fewr 3. presence of lymphatic nodules (Peyer's patches) 4. absence of Brunner's glands |
|
|
Structure that characterizes the ileum
|
lymphatic nodules of the Peyer's patches
|
|
|
function of the Ileocecal junction
|
1. prevents retrograde movement of fecal contents back into the ileum
|
|
|
structure of ileocecal junction
|
1. reduction in size and number of villi
2. muscularis mucosa continues uninterrupted like submucosa and muscularis externa |
|
|
Enteric nervous system
|
2 layers of neurons located on the wall of GI tract. Meissner's plexus and auerbach's (myenteric) plexus
|
|
|
Meissner's plexus is located btw? Auerbach's (myenteric) plexus located btw?
|
Meissner's plexus: btw submucosa and muscularis externa layers. Auerbach's (myenteric) plexus: between muscularis externa and longitudinal layer of smooth muscle.
|
|
|
Function of the appendix
|
1. immunologic role
2. potential B cells gains immunocompetence |
|
|
structure of appendix
|
1. 2.5 - 13cm in length
2. lacks both plicae circularis and villi 3. mucosa is similar to that of the colon 4. large lymphatic nodules 5. appendix may or may not be there in some adults |
|
|
function of the colon
|
1. reabsorption of electrolytes and water
2. elimination of undigested food and other waste material |
|
|
structure of the colon
|
1. 1.5m in length
2. simple columnar epithelium made of goblet cells, absorptive cells, and enteroendocrine cells 3. paneth cells are absent 4. teniae coli: expansions of parts of outer longitudinal layer of the mascularis externa 5. crypts of Lieberjuhn |
|
|
T/F
Stomach has crypts, no villi. Small intestine has villi, no crypts. |
true
|
|
|
structure of the rectum
|
mucosa of the rectum is the same as that of the colon: columnar epithelium
|
|
|
structures of the anal canal
|
1. stratified epithelium, nonkeratinized (upper portion of the anal canal)
2. keratinized stratified squamous epithelium at the lower portion of anal canal 3. the lower portion of the anus is associated with sebaceous flands and hair follicles |
|
|
anocutaneuous junction
|
1. muscularis mucosa ends at the junction
2. the smooth muscles of the circular level of the muscularis externa thickens to become the internal anal sphincter 3. the external sphincter is formed by the striated muscles of the pelvic Fl and perineum 4. sebaceuous glands |
|
|
crypt of Lieberkuhn are found where?
|
It's found in the small intestine and colon
|
|
|
liver function
|
1. has both exocrine and endocrine functions
2. hemopoiesis beginning in the 3rd month of gestation |
|
|
liver: 2 largest what?
|
largest internal organ and largest mass of glandular tissue in the body
|
|
|
structure of liver
|
1. receives blood from the hepatic portal vein (venous blood from GI, pancreas and spleen)
2. lobules or acini are the functional units 3. blood sinusoid, separates acini |
|
|
vessels of the liver
|
arterial blood come from the hepatic artery, venous blood come from the portal vein. central veins carry clean blood from the sinusoid. portal vein and hepatic vein come together at the central vein.
|
|
|
blood flow in the liver
|
portal vein and hepatic artery -> hepatic sinusoids -> central (hepatic) vein -> leaves the liver
|
|
|
Kupffer cells and hepatocytes
|
kupffer cells (macrophages) and hepatocytes clean the blood, before the blood reaches the central vein.
|
|
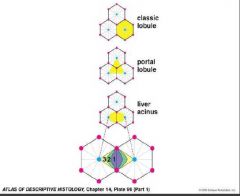
Classic liver lobule: what's in the center? corners are consist of what?
Portal lobule: what's in the center? the corners are consist of what? hepatic acinus: arranged around what? what's on the corners? |
Classic liver lobule: central vein is at its center. portal triads lie at the corners of hexagonal classical liver.
Portal lobule: portal triad is at its center. centeral veins are at its 3 corners. Hepatic acinus: with 2 portal triads and 2 central veins at its corners. branches of portal artery, vein and bile duct running btw the portal triads. |
|

the 3 concentric elliptical zones
|
1. these cells are the 1st to receive O2, nutrients, and toxins from the sinusoidal blood and to show morphological changes; they are last to die and the first to regenerate
2. are the first to show ischemic necrosis due to limited circulation and the 1st to show fat accumulation 3. cells have functional and morphological characteristics and responses intermediate to those of zone 1 and 3. |
|
|
Functional units of livers (3 units) and its shapes
|
1. classic liver lobule (hexagon)
2. portal lobule (triangle) 3. hepatic acinus (diamond) |
|
|
Can hemopoesis resume if bone marrow losses its ability to produce blood cell?
|
yes to some degree
|
|
|
where's RBC's located in the liver
|
btw the liver parenchymal cells and the endothelium lining the vascular sinuses
|
|
|
Flow of bile in the liver from cells to the duct
|
bile canaliculus (intercellular space) -> bile ductule (periphery of the lobule) -> bile ducts (portal traid) -> left and right hepatic ducts -> gall bladder
|
|
|
portal triads are composed of 3 structures
|
branches of portal vein, hepatic artery and bile duct
|
|
|
bile contains
|
conjugated bile salts, cholesterol, phospholipids and bilirubin
|
|
|
structure and cells of gallbladder
|
1. tall, columnar, absorptive epithelial cells
2. attach to the surface of the liver 3. muscularis resembles the muscularis externa in the intestine (consists of smooth muscle bundles) 4. adventitia contains nerves and blood vessels 5. no muscularis mucosa and submucosa 6. basolateral intercellular space 7. lymphocytes 8. mucus-secreting glandFuFun |
|
|
what is Rokitansky-Aschoff sinuses, what organ does it belong to?
|
They are outpouches of the epithelial lining that can extend thru the muscularis. It's found in the gallbladder and is associated with gallstones.
|
|
|
Function of pancreas
|
1. source of enzymes that break down fats, CHO, proteins, substance that neutralize stomach acid.
2. insulin, glucagon and somatostatin |
|
|
Structure of pancreas
|
exocrine: serous secreting acinar cells. endocrine: islets of Langerhans
|
|
|
islet of Langerhans
|
B cells: insulin
A cells: glucagon D cells: somatostatin |
|
|
course of enzyme secretion in pancreas
|
Acini -> intercalated ducts -> intralobular ducts (simple cuboidal) > pancreatic duct
|

