![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Layers in Ovary
|
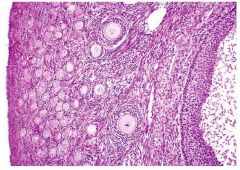
1. Tunica Albuginea: dense irregular connective tissue
2. Germinal Epithelium: simple cuboidal epithelium 3. Cortex: ovarian follicles, cellular connective tissue smooth muscle cells 4. Medulla loose connective tissue contorted blood vessels lymphatic vessels nerves |
|
|
Pathway of the Oocyte (has to rupture through)
|
|
|
|
Fetal life to Menopause Oocytes
|
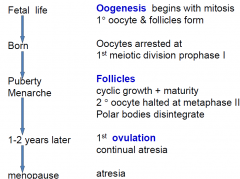
|
|
|
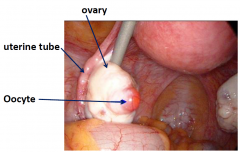
Oocyte emerging
|
|
|
|
FOLLICLE DEVELOPMENT stages
|
1. Primordial
2. Growing 3. Mature Graafian |
|
|
Ovarian follicles
|
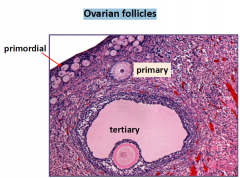
|
|
|
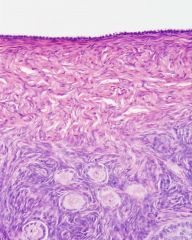
Primordial Follicle
|
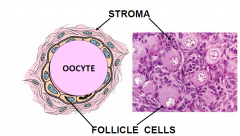
flattened epithiel cells begining of a primodial follicle (Differentiate and become secretory as they mature)
1. Oocyte 30um diameter large nucleus Balbiani Bodies = organelles 2. Follicle cells; simple, squamous epithelium basal lamina |
|
|
GROWING FOLLLICLE (PRIMARY)
|
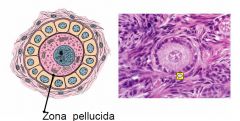
Z.P; secreted by the oocyte and like a shell
- need to sperm to be able to pentrate the zona pellucida (allowing only one sperm to eneter - acrosomal reaction) Follicle cells: cuboidal follicel cells - from the squamous before |
|
|
GROWING FOLLICLE CELLS 2
|
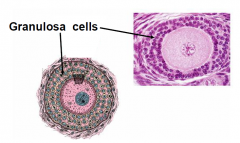
3-layers (follicle cells now called granulosa cells)- now have a secretory function
no blood supply enters here; there is a BM that the macromolecules have to cross but since there isnt any tight junction around here then the nutrients diffuse throughout (no blood ova barrier verses blood testies barrier- (because sperm is foreign in a male) |
|
|
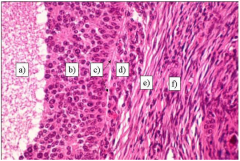
GROWING FOLLLICLE (SECONDARY)
|
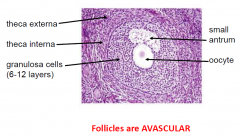
follicle cells = granulosa cells
* Stroma 1. theca interna cuboidal secretory cells vascular produce Oestrogen precursor 2. theca externa connective tissue smooth muscle cells collagen |
|
|
Growing oocyte requires?
|
growing oocyte requires FSH, IGF-1, EGF, Ca2+
|
|
|
MATURATION PROCESS
|
1. Zona pellucida layed down
2. Theca cells producing oestrogen precursor 3. Balbiani bodies disperse 4. Secretory vesicles appear close to oocyte which contain proteases 5. fluid-filled antrum develops & is secreted by granulosa cells - OMI inhibits further growth of oocyte 6-12 layers of granulosa cells 6. Oocyte pushed to side 125um diameter follicle now 10mm diameter 7. Granulosa cell changes increase in microvilli on antral surface :. increase in LH receptors 6-12 layers of granulosa cells |
|
|
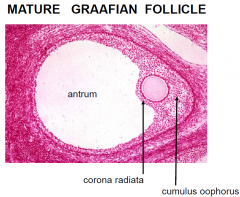
MATURE GRAAFIAN FOLLICLE
|
|
|
|
Cumulus Oophorus
|
The cumulus oophorus (Latin cumulus=heap, Greek oo=egg + phor=carrier; latinized ending "-us"),
|
|
|
Corona Radiata
|
The corona radiata is the innermost layer of the cumulus oophorus and is directly adjacent to the zona pellucida, the outer protective layer of the ovum
|
|
|
MATURE GRAAFIAN FOLLICLE
|
|
|
|
Pituiatary Control over Hormones produced by oocyte
|
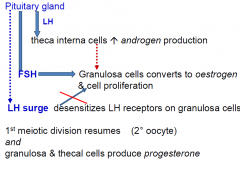
|
|
|
OVULATION
|
1. Increase in antrum fluid
2. proteolysis of follicular wall 3. deposition of glycosaminoglycans around oocyte 4. smooth muscle contraction in theca externa due to prostoglandins 5. blood flow stops on ovary surface 6. surface ruptures 7. oocyte, corona radiata, cumulus oophorus expelled |
|
|
Theca lutein cells
|
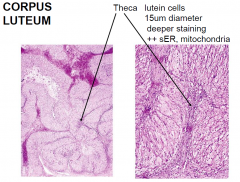
|
|
|
Granulosa Lutein Cells
|
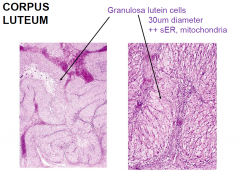
|
|
|
Corpus Luteum
|
remaining follicle after ovulation
bleeding capillaries in theca interna = clot forms stromal connective tissue invades antrum blood vessels grow into granulosa layer granulosa and thecal cells = lutein cells progesterone and oestrogen production |
|
|
CORPUS
LUTEUM no fertilization |
14 Day life then degenerates gradual decrease in hormone production becomes a scar = corpus albicans (or white corpus) which degenerates over 2 months
|
|
|
CORPUS
LUTEUM yes fertilization |
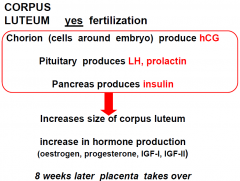
|
|
|
FERTILIZATION from the oocytes perspective
|
sperm must penetrate the
corona radiata, zona pellucida & oocyte plasma membrane several sperm penetrate ZP BUT polyspermy blocked by… 1. large, prolonged depolarization of oocyte plasma membrane 2. proteases released from oocyte degrade sperm receptors 3. proteases create the perivitelline barrier with the ZP |
|
|
MAMMARY GLANDS Hormones
|
Oestrogen
• promote breast development by stimulating duct & connective tissue growth • accummulation of adipocytes Progesterone • prepare breast for lactation by promoting lobe proliferation Prolactin from adenohypohysis • initiates milk secretion by the cells Oxytocin from neurohypophysis • initiates ejection of milk from the mammary glands |
|
|
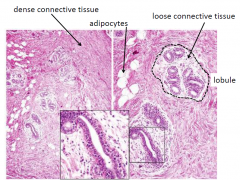
MAMMARY GLANDS;
structure |
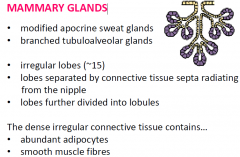
|
|
|
Areola & Nipple
|
Areola contains
sebaceous glands, sweat glands, increased pigmentation & sensory nerve endings Nipple Numerous sensory nerve endings Lactiferous ducts lined with stratified squamous epithelium open onto nipple |
|
|
Ductal cells
|
gradual transition in the epithelium
From simple cuboidal or columnar epithelium near secretory cells To Stratified squamous epithelium |
|
|
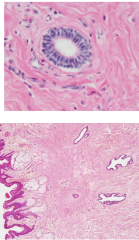
INACTIVE BREAST
|
|
|
|
LACTATING BREAST
|
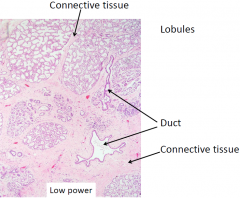
|
|
|
Lactating Breast High Power
|
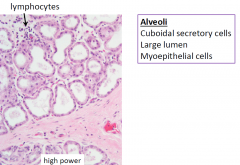
myoepithelial cells contract
|
|
|
UTERINE TUBES
Wall of uterine tubes composed of 3 layers: |
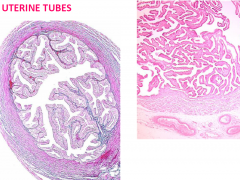
Mucosa
longitudinal folds project into the lumen lined with ciliated & non-ciliated columnar epithelial cells Muscularis inner circular, outer longitudinal smooth muscle layers Serosa (peritoneum) Mesothelium & thin connective tissue layer |
|
|
Uterine Tube lumen
|
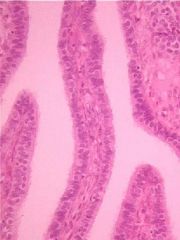
- lined with cilia allowing for motility
|
|
|
ECTOPIC PREGNANCY
|
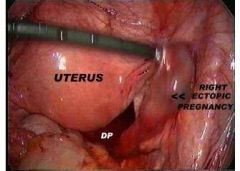
disater @ 6 weeks of growth the female gets Sx (blleding, crampng, nausea, rupture, death, sever back pain on that side)
- a lot worse than normal ovarian pain |
|
|
Menstrual Cycle
|
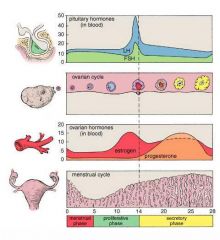
|
|
|
UTERUS WALL LAYERS
|
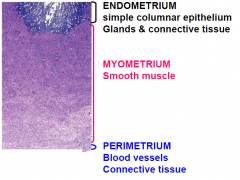
ENDOMETRIUM simple columnar epithelium Glands & connective tissue
MYOMETRIUM Smooth muscle (INC. in pregnancy, hypertrophy and hyperplasia to deliver the baby) - lots of muscle in different directions for contraction PERIMETRIUM Blood vessels Connective tissue |
|
|
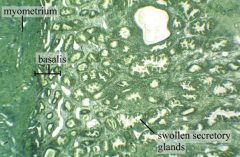
Endometrium
|
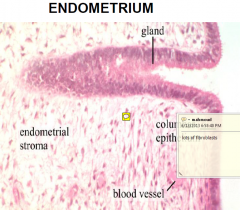
stratum functionalis
• Adjacent to lumen • Changes with the menstrual cycle • Shed during menstruation stratum basalis • provides basal cells for regeneration of stratum functionalis |
|
|
Uterine wall Blood vessels
|
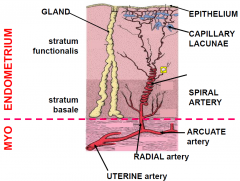
spiral allows strech and moves
LACUNAW: fill with blood suppling the surface - shed and can expose the spiral aa. |
|
|
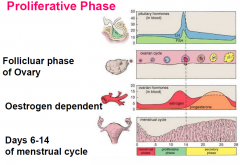
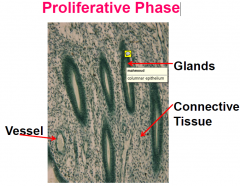
Proliferative Phase
|
|
|
|
Proliferative Phase: Histology
= regeneration and growth |

Doubles in thickness (c 5mm)
Glands tightly packed and coiling +/- Oedema in connective tissue |
|
|
Proliferative Phase Glands
|
|
|
|
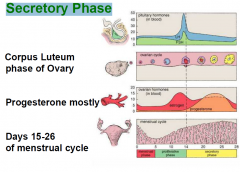
Secretory Phase: Menstrual Cycle
|
|
|
|
Secretory Phase: Histology
|
• Glands appear saw-tooth shaped (INC> SA to INC. production)
• Spiral Arteries – lengthen, more coiled • Oedema |
|
|
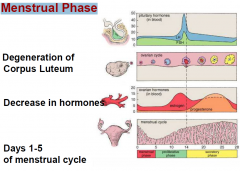
Menstrual Phase: Cycle
|
|
|
|
Menstrual Phase: Process
|
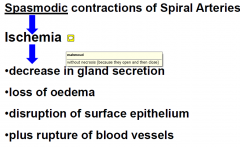
|
|
|
Menstrual Phase Histology
|
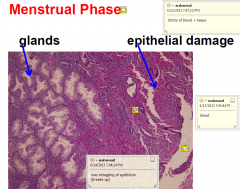
|
|
|
Menstrual Cramps
|
Sm contraction of myometrium (menstrual cramps)
|
|
|
The different stages of the endometrial lining LOW POWER
|
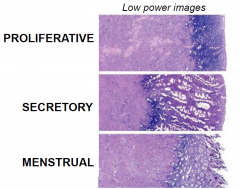
|
|
|
The different stages of the endometrial lining HIGH POWER
|
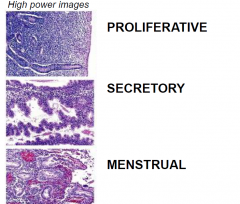
|
|
|
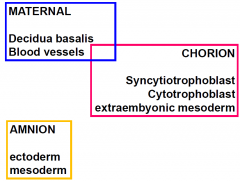
Placenta cells Overview
|
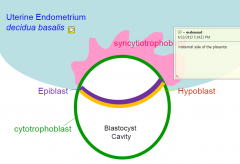
|
|
|
Placenta - Maternal Blood
|
|
|
|
Placenta fetal surface to maternal surface
|

CP: Chorionic plate; solid plate that makes the chorionic villi (with the fetal vessles inside)
maternal blood filtering around the villispaces DC: decidua basalis |
|
|
Fetal Circulation to maternal circulation
|
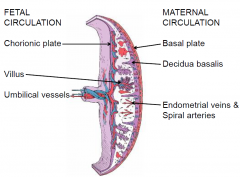
|
|
|
intervillous spaces
|
Chorionic villi emerge from the chorion, invade endometrium
& allow transfer of nutrients from maternal blood to fetal blood |
|
|
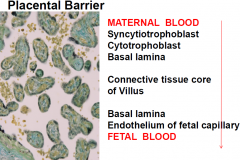
Placental Barrier
from maternal to fetal |
|
|
|
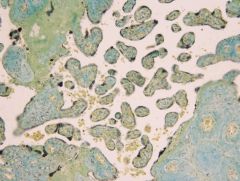
Placental Villi
- high power |

2 outer cell layers:
OUTER: smaller and cuboidal shaped (syncorto) INNER: larger and can be multi-nucleated) |
|
|
Problems with the Placenta
|
1. Placenta previa Covers the cervix
2. Placental abruption Comes away from uterine wall 3. Pre-eclampsia Hypertension + proteinuria |
|
|
CERVIX ENDOTHELIUM
|

large glands change with cycle (allows or inhibts sperm passage)
No spiral arteries Not shed during menstruation |
|
|
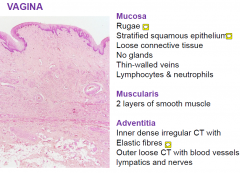
VAGINA
3 layers |
|
|
|
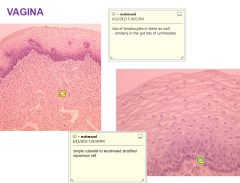
VAGINA HIGH POWER
|
|

