![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
172 Cards in this Set
- Front
- Back
|
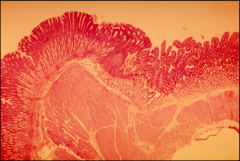
What type of epithelium is the esophagus
|
Stratified squamous cell non ketatinizng
|
|
|
What is the submucosa of the esophagus:
|
seromucous glands
|
|
|
What are the specialized cells in the epithelium of the esophagus ?
|
Langerhans cells (antigen presenting) lympocytes, merkel cells (neuroendocrine cells)
|
|
|
What is the muscularis externa of the esophagus comprised of:
|
Upper: 1/3 skeletal
Middle: 1/3 skeletal and smooth lower: 1/3 smooth |
|
|
What is the status of lymph nodules in the esophagus:
|
rare but may be encountered along the esophagus
|
|
|
What causes barrett's esophagus?
|
chronic inflammation perhaps dude to esophageal reflux disease (GERD) is associated with metaplastic response
|
|
|
What can barrett's esophagus cause?
|
Increase risk of carcinoma
|
|
|
Esophageal varices occur toward what portions of the esophagus?
|
Lower
|
|
|
What do esophageal varices induce?
|
portal hypertension which can lead to life threatening bleeding risks
|
|
|
What is the primary treatment for esophageal varices?
|
surgical treatment TIPS-transjugualr intraheptatic portosytematic shunt
|
|
|
temporary treatment for esophageal varices is designed to do what? and what tool is usually used
|
stabilize the vessels and usually involves use of esophageal ballon tamponade
|
|
|
esophageal junction has what type of epithelium?
|
simple columnar
|
|
|
What do glands from the esophagus do?
|
protect the esophagus from acid reflux by secreting bicarbonate, mucous
|
|
|
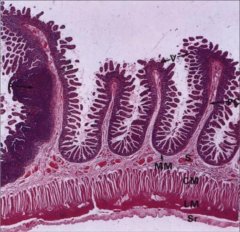
What is is the musclaris mucosa for the stomach
|
inner-circular, outer longitudnal, rugae:
|
|
|
What are rugae?
|
folding of mucosal linning that flatten with stomach distention
|
|
|
Indentify the type of sumucosa of the stomach?
|
Dense connective tissue and no glands
|
|
|
what are the layers of the Musclaris externa for the stomach?
|
Inner: oblique (limtted to views in histo slides)
middle: circular outer: longitudinal |
|
|
where are cardia and cardiac glands present?
|
only present close to gastro-esophagel junction
|
|
|
Parietal cells (oxyntic) are stained in which way?
|
eosinphillic
|
|
|
What do parietal cells produce?
|
Hydrogen ions for generation of HCL which activates pepsiongen to produce active pepsin
|
|
|
what do parietal cells synthesize?
|
intrinstic factor
|
|
|
what is the purpose of the instrinsic factor
|
to allow the abosoportion of b12 in the small intestine and necessary for red blood cell maturation
|
|
|
what happens if intrinisic factors are lost?
|
pernicious anemia
|
|
|
where are intrinsic factors sent to?
|
ileum
|
|
|
Chief cells (zymogenic) are stained in which way
|
Basophillic
|
|
|
What do chief cells produce
|
pepsiongen
|
|
|
Generate HCL:
|
Generate HCl: CO2 + H2O------>H+ + HCO3-
�� |
|
|
In parietal cell's where does K+ and cl- exit the cell
|
into the cannilculli
|
|
|
what type of pump do parietal cells use?
Is it is with or against the concentration gradient? |
H+/K+ pump ATPase
against |
|
|
In parietal cells histamine is realsed from what type of cells?
|
enterochromaffin cells (ECL cells)
|
|
|
what type of cells release gastrin?
|
enteroendrocrine cells( G cells)
|
|
|
what section of the partietal cell is bicarbonate exchanged?
|
basal side
|
|
|
Why are chief cells heavily basophilic?
|
due to high volume of rER
|
|
|
What intitates pepsinogen release?
|
gastrin
|
|
|
Gastrin is released by what nerve
|
Vagus
|
|
|
what type of glands secrete a bicarbonate rich solution to neutralize the acidic chyme entering the small intestine?
|
Brunner's glands
|
|
|
Where do all stems of the gi system reside?
|
in the crypts adjacent to paneth cells
|
|
|
where does the vast majority of colon cancers begin
|
in the crypts
|
|
|
enterocytes produce?
|
Secretory Piece
|
|
|
What do seceretory pieces do?
|
Allows dimeric secretory IGA to be escorted through the cells to lumen. Protecting it from intra and extracelluar degradation.
|
|
|
IgA is produced by
|
plasma cells
|
|
|
pancreatic zymogens are absorbed onto the?
|
glyocalyx
|
|
|
what is so significant about the glyocalyx?
|
it is critical for intestinal absorption
|
|
|
What type of enzymes does it harbor?
|
converting carbohydrates to disaccharide and monosaccharides. breaks down short-chain peptides their constituent amino acids
|
|
|
What type of cells produce enterokinase?
|
enterocytes
|
|
|
enterocytes activate which zymogen
|
they convert tyrpinsogen to trypsin
|
|
|
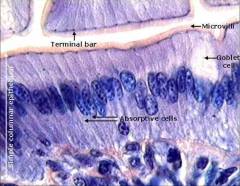
what part of the small intestine are goblet most numerous
|
illeum
|
|
|
what is the function of glycoprotien mucins
|
used to lubricate and protect intestinal lining
|
|
|
what type of cells produce glycoprotien mucins?
|
goblet cells
|
|
|
which cells have larger secretory granules than enteroendocrine cells?
|
paneth cells
|
|
|
What do paneth cells secrete?
|
Lysozome, phospholipase A2, Defensin peptide
|
|
|
Lysozome, phospholipase A2 and defensin peptide primary fucntions are to?
|
breakdown bacterial cell walls
|
|
|
Enteroendocrine cells secrete hormones exerting what type of effects on digestion?
|
paracrine and endocrine
|
|
|
stem cells are always adjacent to?
|
Paneth cells
|
|
|
what type of signaling molecules do paneth cells secrete?
|
Wnt, EGF, and notch ligands
|
|
|
Paneth or enteroendocrine cell granules are located apically?
|
Paneth granuels
|
|
|
Paneth or enteroendocrine cell granules are located basally?
|
Enteroendocrine granules
|
|
|
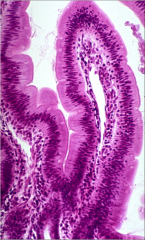
which section of the small intestine has the longest villi?
|
jejunum
|
|
|
In the jejunum, what type of glands are missing?
|
brunner's glands
|
|
|
the contents of the jejenum are always?
|
isotonic
|
|
|
what happens if the entire jejunum is lost?
|
illeum will take over absorptive roles
|
|
|
Enamel covers the
|
crown
|
|
|
what is the hardest tissue
|
Enamel 96% hydroxapatite
|
|
|
What is the organization of enamel
|
6 enamel rods
|
|
|
enamel is a product of?
|
ameloblasts
|
|
|
why are the six enamel rods oriented perpendicular to the tooth surface?
|
strength
|
|
|
what are caries? and what are their purpose?
|
bacteria (streptococcus mutans and lactobacilli) convert carbohydrates into acids
|
|
|
what are tooth cavities caused by?
|
tooth cavites are caused when acids deminerlize enamel hydroxyapatte
|
|
|
what is the cause of tetracycline teeth?
|
tetracyline antibiotic intake before 8 years old or through pregnant mother
|
|
|
tetracycline antibiotic does what?
|
chelates Calcium and incorprates it into hydroxyapatite
|
|
|
what is product of odontoblasts?
|
dentin
|
|
|
what type of matrix do odontoblasts lie down
|
predentin
|
|
|
what is the composition of dentin
|
68% hyroxapatite and type I collagen
|
|
|
Primary dentin is produced:
|
before eruption
|
|
|
secondary dentin produced:
|
after eruption
|
|
|
tertiary dentin produced:
|
in response to irriation
|
|
|
Odontoblast processes extend into the?
|
dential tublues
|
|
|
why are odontoblasts processes extending into the dentinal tubules?
|
odontoblasts move pulpward as they produce dentin but leave their processes behind
|
|
|
What all structures extend into the dental tubules
|
fiber nerve endings( pain fibers) and odontoblasts
|
|
|
Hydrodynamic mechanism is induced how?
|
thermally induced movement dentinal fluid
|
|
|
where does the pulp lie
|
a restricted rigid chamber
|
|
|
what type of tissue is pulp?
|
very celluar loose connective tissue
|
|
|
what structure of the tooth is a rich supply of small vessels and nerves?
|
pulp
|
|
|
Which tooth structure or structures is/are avascular?
|
enamel and dentin
|
|
|
A- delta fibers create
|
sharp pain
|
|
|
C-fibers create
|
dull poorly localized pain, which we associate with toothaches
|
|
|
Teeth are supplied with what type of fibers
|
pain and sympathetic
|
|
|
A delta fibers are assoicated the
|
dentin
|
|

primary defintion: erupts between
Primary detention erupts between |
6 months to 3 years
6 years and 25 years |
|
|
B cells are expressing B cell receptors (BCR) capable of recognizing both?
|
soluble and membrane-bound antigens.
|
|
|
Upon activation, B cells differentiate into plasma cells, which are dedicated to synthesize?
|
antibodies (the soluble forms of the B cell receptors).
|
|
|
TH cells express T cell receptors (TCR) and ?
|
CD4
|
|
|
TCRs recognize antigens presented on cell surface by
|
class II MHC complex.
|
|
|
which one of these statments is untrue about how TH cells are crucial for defense against both extracellular and intracellular pathogens?
help to activate TC cells to kill virus infected target cells stimulate B cells to make antibodies to activate or eliminate extracellular pathogens [TH2] activate macrophages to destroy intracellular pathogens multiplying within the phagosomes [TH1] also stimulate dendritic cells (DCs) to remain in an activated state �� |
stimulate B cells to make antibodies to activate or eliminate extracellular pathogens [TH2]
|
|
|
T cell receptor (TCR) complexes. Recognize antigens only if they are presented by?
|
histocompatibility complex Class I and II (MHC-I and MHC-II) molecules.
|
|
|
The ‘cytoplasmic tail’ of a BCR is too short to initiate signaling on its own, how does it initiate a signaling cascade?
|
it relies on coreceptors and adapter molecules
|
|
|
Antibodies (Abs) are produced in what types of forms:
� |
either secreted or membrane-bound forms.
|
|
|
In Membrane-bound ABs serve as B cell receptors that initiate?
|
the antigen-triggered activation of B cells,
|
|
|
while secreted Abs function as
|
mediators of humoral immunity.
|
|
|
CD4 is expressed on:
|
TH (helper) cells and binds MHC Class II molecules
|
|
|
CD8 is expressed on:
|
TC (cytolytic) cells and binds MHC Class I molecules
|
|
|
in the process called V(D)J recombination� how are things arranged
|
randomly
|
|
|
Antigen Receptor Gene Rearrangements occu�r primarly in?
|
lymphoid organs (thymus bone barrow)
|
|
|
Antigen Receptor gene rearragnments do or do not rely on the presence of antigens?
|
they do not. they are antigen independent
|
|
|
What are naive matured lymphocytes:
|
lymphocytes that left the primary lymphoid organs with fully capable receptors, but have not yet encountered with their cognate antigen
� |
|
|
each lymphocyte expresses a cell-surface receptor that is specific for a particular ‘________ antigen �
|
abstract
|
|
|
where does a lymphocyte generally encounter its specific antigen
|
perphial lymphoid organ
|
|
|
multiple sets of lymphocytes (clones) are generated, with varying affinity and specificity to the antigen that incited the immune response is referred to as?
� |
polyclonal
|
|
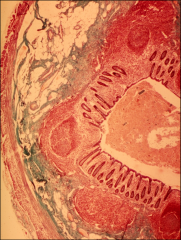
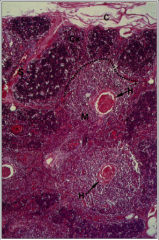
identify the ogran two parts
|
Pyloric stomach (left)
Right (duodenum) |
|
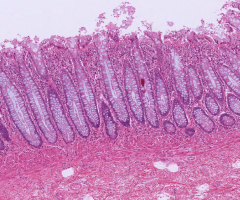
1)identify the organ?
2) what type of glands are on the bottom |
1) duodenum
2) brunners gland |
|
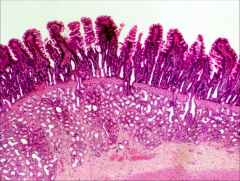
1) what is the classification of this epithelium
|
1) duodenum epithelium (eneroyctes)
|
|
1) identify this structure?
2) what type of cells are in its lamina propina? 3) what type of tissue |
1) central lacteal
2) endothelial cells, lymphocytes, etc. 3) connective tiissue � |
|
|
What is the plicae circularis?
|
a fold of intestinal wall that increases surface area beyond that obtained via villi.
� |
|
|
where is plicae circularis most abundant
|
jejunum
|
|
1) identify the organ
2) Identify the large circular structure to the left? 3) what up the projecting pinpoint structure? |
1)illeum
2) peyer's patches 3) plicae circularis |
|
|
the ileum is involved in the absorption of?
|
Involved in absorption of bile salts (essential for absorption of fats and fat soluble vitamins) and vitamin B12 �
|
|
|
60-70% of all immune system cells of the body reside in the intestines. �true or false
|
True
|
|
|
Ileum is most important for conservation of?
|
). Ileum is most important for conservation of fluid and electrolytes
� |
|
|
Loss of bile salts recycling following ileal resection leads to less _________, and affects ability of _________ to reabsorb water and salt, leading to chronic diarrhea
� |
fat reabsorption
Colondoyctes |
|
|
what are the prominent strctures missing from the appendix that are present is the illeum and jejenum?
|
villi and crypts
|
|
identify the organ?
|
appendix
|
|
|
what cells are present in appendix?
|
Enteroycytes, goblet cells, and m cells
|
|
1) identify the organ?
2) What structures are missing from this organ? |
1) Colon
2) vili and Plicae |
|
|
which of the following is not antigen presenting cell?Antigen presenting cells (APCs)
macrophages Langerhan’s cells T helper cells dendritic cells |
T helper cells
|
|
|
What are the two primary functions of APC (antigen presenting cells)?
|
phagocytosis
antigen presenting cell |
|
|
T cells effectors are_________ and deal with with type of organisms?
|
cells
intracelluar pathogens (viruses and carcinomas) |
|
|
B cells effectors are_________ and deal with with type of organisms?
|
antibody molecules
extracelluar pathogens bacteria, opsonize targets |
|
|
Binding of antigen binding site of antibody with antigen causes the following for
Neutralization: |
cover or coat
|
|
|
Binding of antigen binding site of antibody with antigen causes the following for
Agglutnination: |
cross linking cells forming a clump
|
|
|
Binding of antigen binding site of antibody with antigen causes the following for
Precipitation: |
preciptiation
|
|
|
where is thymus located?
|
anterior superior mediastinum
|
|
|
What epitheliorectiular cells are associated with the cortex
|
type 1-3
|
|
|
1) Type I erc shape of cells are:
2) what type of junctions do type 1 cells have? separate thymic parenchyma from CT capsule & vessels; functional isolation of devel T cells from CT & vessels |
1) squamous cells
2 z. occludens & desmosomes |
|
|
Type II cells are what type:
|
stellate cells with long cytoplasmic process
|
|
|
Type II cells express what type of anitigen
|
MHC-1 and MHC-2
|
|
|
type iv cells contriubte to barrier what type of junction?
|
ctx/medulla junction
|
|
|
type 3 express which type of anitgens
|
MHC I and MHC II
|
|
|
Which epithelioreteciluar cells are found in the medulla
|
4-6
|
|
|
what type of epithelioretcular cellscontain keratohyalin granules, intermed filaments, lipid droplets; desmosomally connected & concentrically arranged to form Hassall’s corpuscles; keratinization may be evident in thymic corpuscle center; secrete cytokines for : i) local dendritic cell activity control ii) thymic education -- IL-4 and IL-7
|
type VI
|
|
|
type VI--keratinization may be evident in ______ corpuscle center; secrete __________ for : i) local dendritic cell activity control ii) thymic education -- IL-4 and IL-7
� |
thymic
cytokines IL-4 and Il-7 |
|
|
which types of epitheliorectial cells use z occulends
|
Type 1, 3, 4
|
|
|
which type of epitheliorectal cells use desmosomes?
|
Type 1, 2, and 5
|
|
|
what is the purpose of the blood thymus barrier:
|
prevents lymphocytes that
reach the cortex from interacting with antigens |
|
|
what are the components of the blood thymus barrier?
|
type I ercs w/ occlud junctions
+ basement membrane 2. perivascular CT + macrophages (can phagocytose antigens that escape capillaries) 3. endothelium w/ occluding junc.; + basement membrane and ocassional pericyte |
|
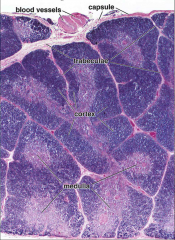
1) identify organ
2) what is the light region? 3) what is the dark region? |
1) thymus
2) medulla 3) cortex |
|
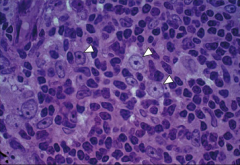
identify the cell pointed by white arrow?
|
eptheliorectiular cell
|
|
identify the red structure?
|
Hassall's corpsule
|
|
|
what does the hassall's corpsule produce?
|
interulukin 4 and 7
|
|
|
what is the purpose of interulkin 4 and 7
|
- thymic differentiation
- T lymphocyte education |
|
|
medullary erc’s (merc’s) express
transcription factor : |
AIRE
|
|
|
what does AIRE do?
|
controls merc differentiation program that
allows tissue-restricted antigens to be expressed, required for self-tolerance |
|
|
what a defect in the AIRE signify?
|
autoimmune
polyendocrine syndrome type 1 (APS-1)- dysfunction of multiple endocrine glands due to autoimmunity |
|
|
What is the difference between positive and negative cell selection?
|
in positive selection if binding does not occur the cell dies apoptosis. uses cortical epithelal cells. Negative is the reverse and use dendritic cells.
|
|
|
how do t cells exit the thymus?
|
via postcapillary venules at the corticomedullary junction and medulla
� |
|
|
where is lymphoid tissue found?
|
Found in alimentary canal, respiratory passages, genitourinary tract
� |
|
|
1) Lympathtic Nodules- are supported by?
2) do they have a complete capsule? 3) how nodules usually dispersed - |
1) reticular cell meshwork
2) no complete capsule; some partially encapsulated 3) randomly dispersed singly or locally clustered (tonsils, Peyer’s patches, vermiform appendix) |
|
|
what is the difference between the a primary lymph nodule and secondary?
|
Primary are mostly small and secondary are usually around germ centers
|
|
|
1) describe the mantle and what types cells are in it?
|
• darkly-stained rim surrounding germinal center • contains darkly-stained resting B cells, TH cells,
macrophages and dendritic cells |
|
|
lymph nodule has no afferent or efferent lymphatics
what type of cells are in the lymph nodule |
afferent
b cell |
|
|
what do germinal centers form
|
post-antigen recognition by lymphocytes & return of lympho’s to 1o nodule to proliferate
� |
|
|
what are the contents of the germinal center?
|
- many euchromatic immature
lymphocytes (lymphoblasts and plasmoblasts) – contributes to lightly-stained appearance - follicular dendritic cells dispersed between B lymphocytes |
|
|
what are the tonsils and where are they located?
|
they are a large irregular mass of lymphoid tissue and located mucosa of posterior oral cavity and nasal pharynx
� |
|
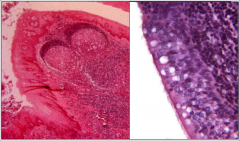
identify organ on left
|
palatine tonisl
|
|
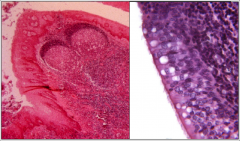
indentify organ on righ
|
pharyngeal tonsil
|
|
|
what is the difference in epithelium between palanine tonsil and a pharyngeal tonsil
|
palatine- stratified squamous epithelium
pharyngeal-respitorary epithelium (psuedo stratified cilliated columnar) |
|
|
lymphoid follicle-associated epithelium (FAE) is important because?
� |
Only site in gut epithelium that is permeable to macromolecules and microorganisms
� |
|
|
what are some autoimmune diseases associated with b lymphocytes?
|
hyperthyroidism (Graves’disease)
antibodies to thyroid hormone receptor stimulate the receptor |
|
|
what are some autoimmune diseases associated with t lymphocytes?
|
- CD8+-autoimmune diseases
based on aberrant recognition of “self”antigen example: multiple sclerosis Cytotoxic T cells attack myelin sheaths in CNS |
|
|
where is the palatine tonsil located?
|
opposite side of oropharnyx
|
|
|
what is it covered by?
|
SSNK epithelium
|
|
|
what is considered the first line of defense against the bacteria entering the oral cavity?
|
palantine tonsil
|
|
|
do palantine and pharyngeal tonsils have CT capsules?
|
palatine-underyling dense CT that as a partial CT capsule
pharyngeal-thin underlying capsule |

