![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
DECUBITUS ULCERS |
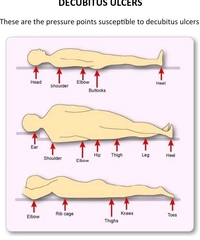
These are the pressure points susceptible to decubitus ulcers: Items that contribute to Decubitus Ulcers:•Pressure (oxygen mask tubing can cause sores behind ears)•Irritants (feces, urine, crumbs, wrinkled sheets)•Diabetes-Nutrition (protein balance)-Age decreases “padding” and mobility•Dehydration = less “cushion” and less circulation. Circulation is important to carry nutrients, oxygen, and medications.
|
|
|
ASSESSMENT OF DYSPNEA |
AMA classifications of dyspnea: Class I: Dyspnea on severe exertion. Class II: Client can keep pace with person of the same age and build on level ground without breathlessness, but not on stairs or hills. Class III: Client can walk a mile at own pace without dyspnea, but cannot keep pace with persons of same age and build on level ground. Class IV: Dyspnea present after walking 100 yards on level ground or climbing one flight of stairs. Class V: Dyspnea with slight activity or at rest. |
|
|
Indicators of dyspnea in adults |
Physical: • Feeling of suffocation • Tightness in chest • Pain • Congestion • Fatigue • GI distress • Palpations • Clamminess or flushed sensations • Vertigo • Memory/concentration problems Emotional: • Anxiety • Anger • Claustrophobic reactions • Panic |
|
|
CALCULATING KILOGRAMS |
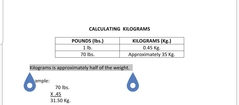
Kilograms is approximately half of the weight.
|
|
|
Calculating Height |
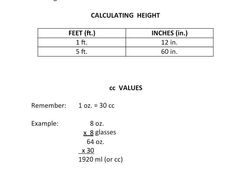
Convert height of 5 feet 2 inches to centimeters.First, convert 5 feet to inches: 5 feet × 12 inches/foot = 60 inchesAdd up our inches: 60 + 2 = 62 inchesConvert inches to cm: 62 inches × 2.54 cm/inch = 157.48 cm Convert height of 144.5 centimeters to inches.Convert cm to in144.5 cm × 0.3937 in/cm = 56.89 inchesAlternately, 144.5 cm / 2.54 in/cm = 56.89 inches |
|
|
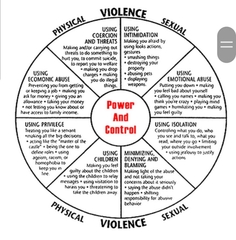
Definition and Types of Violence |
•Domestic Violence – Any assault, aggravated assault, battery, aggravated battery, sexual assault, sexual battery, stalking, aggravated stalking, kidnapping, false imprisonment, or any criminal offense resulting in physical injury or death of one family or household member by another who is or was residing in the same single dwelling unit.•Elder Abuse – Physical, psychological, or sexual acts that jeopardize an individual’s medical care, health status, right to self-determination, personal property or income, and the failure to perform acts that make the environment safe and clean.•Adult Vulnerability – One who is at risk for abuse or neglect due to impaired physical or mental function, or emotional status.
|
|
|
Definition and Types of Violence 2 |
• Battering (abuse) – To strike, beat or assault. Battering can be a pattern of behavior that seeks to establish control over another person through fear and intimidation. It can include emotional, physical, financial, and sexual abuse. It may also include threats, intimidation, and isolation. • Neglect – The failure or omission on the part of a caregiver to provide the care, supervision, and services necessary to maintain the physical and mental health of the individual. • Sexual Abuse – Acts of sexual nature committed in the presence of the individual without that person’s informed consent. |
|
|
Definition and Types of Violence 3 |
• Psychological Injury – Any injury to the intellectual functioning or emotional state of an individual evidenced by the reduction in the individual’s ability to function within the customary range of performance and behavior. • Exploitation – The improper or illegal use or management of another’s property. The use of power of attorney or guardianship for personal advantage. |
|
|
Forms of Abuse |
• Physical – abuse ranges from pushes and shoves to slaps, kicks, punches, burns, knife/gunshot wounds. • Emotional – degrading verbal behavior is common. • Sexual – rape after physical abuse, forced sex, forced use of objects in sexual acts, or unprotected sex. |
|
|
Forms of Abuse |
• Economic – enforced poverty, lack of food, clothes, or health care. • Destruction of Pets and Property – Pets or treasured objects may be destroyed. • Threats – “If you leave, I will find you and kill you…or you will never see the children again.” |
|
|
Forms of Abuse |
• Stalking – the individual is followed and watched in a threatening manner. |
|
|
Different kinds of abuse |
|
|
|
Phases of the Abuse Cycle |
• Tension Building Phase – Verbal or other minor battery occurs. The victim takes the blame or accepts responsibility and attempts to calm the abuser. • Acute Battering Incident Phase – Follows the 1st phase, characterized by uncontrollable discharge of tension, and is rarely triggered by victim’s behavior. • Loving Reconciliation Phase – This phase can begin within a few hours to several days after an acute battering incident. The abuser and the victim show an enormous sense of relief that the incident is “over”. Also called the “calm, loving phase or honeymoon phase”. |
|
|
HEAT AND COLD APPLICATIONS |
Heat dilates (expands) blood vessels and increases circulation, providing more oxygen and nutrients necessary for tissue repair. Heat may also reduce inflammation and relieve pain. Cold constricts / shrinks swelling (narrows) blood vessels and helps to prevent or reduce bleeding and swelling. Cold may also be used to reduce fever and pain. Cold is usually first. |
|
|
Guidelines for Safe Application of Heat and Cold |
Follow facility policies and procedures regarding the application of heat and cold. Maintain a temperature of heat applications between 105°F and 115°F (37.8°C and 46.5°C, respectively) Check the water temperature of solutions with a bath thermometer. Keep electrical equipment away from water. Place a waterproof pad under moist heat to keep the bed dry. Add ice to cold applications as necessary to maintain constant temperature. Check for leaks in ice bags, collars, packs, and water bottles. Be sure ice bags are dry before applying. Cover ice bags, hot water bottles, or vinyl containers with cloth before applying to the skin. Be sure that caps or firm parts of bags are away from the skin. Do not fill ice bags or water bottles more than half full. Check the skin frequently under the application and report pale, cyanotic, red, white, or dark coloring. Report patient complaints of discomfort to the nurse promptly. Apply the treatment for the length of time ordered (usually 20 minutes on and 20 minutes off). |
|
|
MAINTAINING FLUID BALANCE |
In order to maintain a fluid balance, the amount of fluid taken into the body must be equal to the amount that is eliminated or used by the body. Adequate hydration for the adult is between two and three quarts (2500 cc) daily. Complications that can occur when the body is not in fluid balance include edema and dehydration. Edema is an accumulation of fluid in the tissues. It usually affects the hands and feet first, although it can occur in other parts of the body. The patient with edema may be on a sodium-restricted diet and fluids may be limited (ice chips are helpful). |
|
|
MAINTAINING FLUID BALANCE 2 |

Dehydration is lack of adequate fluid in the body. It can be caused by vomiting, diarrhea, or bleeding. (Check for skin turgor on hands and chest.) Symptoms of dehydration include dry skin and mucous membranes, sunken eyes, weight loss, decreased urinary output (strong smell or dark odor), constipation, or fever. Fluids should be offered frequently (every two hours) and the amount taken should be measured and recorded.(Dehydration can mean less circulation; less circulation = less nutrients in circulation; decreased O2 ; decreased medication circulation)(Also less fluid = less plump/less padding)Anuria = no urineOliguria = 500 cc or less per day
|
|
|
ELIMINATION (Bowel and Bladder Training) |
Urinary Incontinence Although incontinence is not a normal change of aging, some changes do contribute to incontinence because they make it more difficult to control elimination. Other causes include disease, confusion, medications, decreased mobility, and failure to toilet frequently. |
|
|
ELIMINATION (Bowel and Bladder Training)2 |
Fecal Incontinence It can be caused by poor muscle tone, a change in peristalsis, nervous system damage, or confusion. An illness such as infectious diarrhea may cause temporary incontinence. Fecal incontinence can cause skin breakdown and urinary tract infection. Feelings of embarrassment, guilt, loss of control, and depression may result. Act promptly and professionally when assisting the patient after an incontinent episode. |
|
|
ELIMINATION (Bowel and Bladder Training) 3 |
Preventing Incontinence Incontinence may be prevented by using the following measures: • Offer toileting at regular intervals (minimum of every 2 hours) • Answer call signals promptly • Remind confused patients to use the bathroom on a regular basis • Observe for signs of the need for toileting, such as restlessness, crying, or holding genitals |
|
|
ELIMINATION (Bowel and Bladder Training) 4 |
Constipation Constipation can be caused by poor fluid intake, eating the wrong foods, medication, disease, lack of exercise, or ignoring the urge to defecate. Constipation can often be prevented by adequate fluid intake, increasing exercise, and eating foods that are higher in fiber and bulk. |
|
|
ELIMINATION (Bowel and Bladder Training) 5 |
Cleansing Enemas A cleansing enema involves introducing 750 to 1,000 cc of a solution ordered by a doctor into the patient’s rectum and colon. SSE = soap suds enema. The water temperature for the enema solutions should be 105°F. Sometimes an oil retention solution is used to soften and lubricate the stool. Oil = non-cleansing. |
|
|
Understand Food |
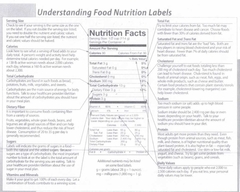
Food |
|
|
RESIDENT’S RIGHTS |
Under F.S. 400.002, residents have the following rights: You, the resident, have the right to: 1. A dignified existence, self-determination, and communication with an access to persons and services inside and outside the facility. You have the right to exercise your rights as a resident of the facility and as a citizen or resident of the United States. 2. Be free from interference, coercion, discrimination, or reprisal from the facility in exercising your rights. 3. Inspect and purchase photocopies of all records pertaining to you upon written request and 24-hour notice to the facility. |
|
|
RESIDENT’S RIGHTS 2 |
4. Be fully informed in language you can understand of your rights and all rules and regulations governing resident conduct during your stay at this facility. 5. Refuse treatment and refuse to participate in experimental research. 6. Manage your own financial affairs. The facility shall not require you to deposit your personal funds within the facility. 7. Choose a personal attending physician. (This physician MUST agree to see you in the facility within 48 hours of your admission and at least once a month thereafter.) 8. Be fully informed in advance about care and treatment that may affect your well-being. 9. Participate in planning care and treatment or changes in care and treatment. 10. Have personal privacy and confidentiality of your personal and clinical records. Personal privacy includes accommodations, medical treatment, written and telephone communications, personal care, visits and meeting of family and resident groups. |
|
|
RESIDENT’S RIGHTS 3 |
11. Approve or refuse the release of personal and clinical records to any individual outside the facility. The right to refuse release of personal and clinical records does not apply when the resident is transferred to another health care institution or when record release is required by law or third party payment contract. You and your legal representative have the right to have access to your medical records within 24 hours of a request, except on weekends and holidays. 12. Voice grievances with respect to treatment or care without discrimination or reprisal. 13. The facility must respond promptly to grievances and make a concerted effort to solve problems. 14. Examine the results of the most recent Federal and State surveys. The resident also has the right to examine the plans of correction in effect at the facility. Survey results shall be posted by the facility in a place readily accessible to the residents. |
|
|
RESIDENT’S RIGHTS 4 |
15. Receive information from agencies acting as client advocates and be afforded the opportunity to contact those agencies. 16. The resident has the right to refuse to perform services for the family. 17. If you choose, you may perform services for the facility when: a. The faculty has documented the desire to work in the plan of care. b. The plan of care specifies the nature of the services performed and whether the services are voluntary or paid. c. Compensation for paid services is at or above prevailing rates. d. The resident agrees to the work arrangement. 18. Privacy in written communications and to send and |
|
|
RESIDENT’S RIGHTS 5 |
18. Privacy in written communications and to send and receive mail promptly and unopened. 19. Have access to stationary, postage, and writing implements at your own cost. 20. Receive visitors during facility visitation hours. Subject to the resident’s right to withdraw or deny consent at any time, the facility shall provide the resident’s immediate family or other relatives immediate access to the resident. Immediate access to the resident will be provided to others who are visiting with the resident’s consent, subject to reasonable restrictions, and the resident’s right to deny or withdraw consent at any time. |
|
|
RESIDENT’S RIGHTS 6 |
1. Regular access to the private use of a telephone. 22. Retain and use personal possessions, including some furnishings and appropriate clothing as space permits, unless to do so would infringe upon the rights or health and safety of other residents. 23. Share a room with your spouse if your spouse is also a resident of this facility AND if both you and your spouse agree to share a room. 24. Self-administer medications unless the interdisciplinary care plan team has determined that this practice is unsafe for you. 25. Be free of any physical restraints or psychoactive medications which are not required to treat your medical symptoms and which are administered for the purpose of discipline or convenience. 26. Be free of physical, verbal, and mental abuse, corporal punishment, and involuntary seclusion. 27. Choose activities, schedules, and health care consistent with your interests, assessments, and plan of care. |
|
|
RESIDENT’S RIGHTS 7 |
28. Interact with members of the community both inside and outside the facility. 29. Make choices about aspects of your life in the facility which are significant to you. 30. Organize and participate in resident groups in the facility. 31. Reside and receive services in the facility with reasonable accommodation of individual needs and preferences, except when the health or safety of you or other residents would be endangered. 32. Receive notice before your room or roommate assignment in the facility changes except in emergencies. The facility reserves the right to determine room assignments of resident placement. The facility shall endeavor to honor the requests of the resident whenever possible. The resident has the right to refuse a transfer to another room in the facility that is skilled to a portion of the facility that is not such skilled nursing facility, without jeopardizing the resident’s eligibility for Medicare or Medicaid benefits. 33. File a complaint with the State survey and certification agency concerning resident abuse, neglect, misappropriation of resident property in the facility, and noncompliance with the advance directive requirements. ** If the resident has been adjudicated incompetent, the person appointed under state law to act on his or her behalf shall exercise the resident’s rights. |
|
|
What are Indirect Care Skills? |
Candidates often ask, “What are indirect care skills?” Indirect care skills are one of the five skills on which the candidate is scored during the Clinical Skills Test and are behaviors that are a part of the performance of every skill. The five categories of indirect skills are: • Resident’s Rights – Did you show respect for the resident’s dignity and privacy? Did you knock before entering the resident’s room? Did you avoid unnecessary exposure of the resident? Were you gentle in your handling of the resident? • Safety – How did you leave this resident when the skill was complete? Was the call light positioned within reach of the resident? Was the resident moved and positioned in a safe manner that did not place the resident at risk of a fall or injury? Was the bed left in the lowest position at the conclusion of the skill? |
|
|
What are Indirect Care Skills? 2 |
• Standard (Universal) Precautions/Infection Control Measures – Did you wash your hands when needed? Did you use gloves when necessary, such as when providing mouth care, handling dentures or when handling a wet incontinent pad or providing perineal care? Did you remove the gloves without contaminating yourself? Did you dispose of soiled items correctly? Did you contaminate yourself or the resident’s personal items? • Communication – How did you verbally interact with the resident? Did you keep the resident informed of what you were doing as you performed the skill? Did you interact with the resident? Were your communications respectful? • Comfort – How did you leave the resident at the end of the skill? Did you ensure the resident’s comfort? Did you address the resident’s comfort throughout each skill? |
|
|
Assessing Listening Skills |
• Listen for restatement and reflection to check understanding. The candidate who actively listens will rephrase what they’ve heard (restatement) and communicate feeling as well as content (reflection). • Look for the candidate to focus on what you are saying at that particular moment. Since listening speed is faster than talking speed, the candidate should be analyzing the factual content and emotional tone and body language. If the candidate reacts with surprise, excitement or concern over what you’re communicating, you will know that he/she is focused on your delivery. • If the candidate maintains eye contact with you, it shows that he/she is interested in what you have to say. Typically, active listeners maintain eye contact 80 percent of the time. • Active listeners use silence effectively. Most people are uncomfortable with silence and have an impulse to break it. • Watch for nods and smiles from the candidate to indicate that he/she has heard what you’ve said and is interested in hearing more. If the candidate seems preoccupied with other things, such as ringing cell phones, beeping palm pilots, etc., he/she is not providing his/her full attention to the situation. |
|
|
BASIC DIABETES
|
I. What is diabetes? (Hyperglycemia) A. Diabetes is a disorder of metabolism, the way our bodies use digested food for growth and energy. (Everything turns to sugar – some slower and some faster). B. When we eat, the pancreas automatically produces the right amount of insulin to move glucose from blood into our cells. In people with diabetes, however, the pancreas produces little or no insulin, or the cells do not respond appropriately to the insulin produced. |
|
|
BASIC DIABETES 2 |
II. What are the types of diabetes? A. Type I Diabetes (called Juvenile Diabetes in the past) 1. A person who has Type 1 diabetes must take insulin daily to live (IDDM – injection or pump) 2. Symptoms usually develop over a short period and include increased thirst and urination, constant hunger, extreme fatigue, weight loss and blurred vision. 3. If not diagnosed, it can cause diabetic ketoacidosis, a debilitating diabetic coma. B. Type 2 Diabetes (NIDDM) (Adult onset) 1. The most common form of diabetes. 2. Need oral form of medication to increase efficiency of the pancreas. 3. The pancreas produces insulin, but the body cannot use it effectively (insulin resistance). After a while, insulin production decreases and it can lapse into Type 1 diabetes. (Another problem is due to weight increase – it’s not enough.) 4. Symptoms develop gradually and may include weight loss, frequent urination, increased hunger and thirst, blurred vision, slow healing of wounds and fatigue. C. Gestational Diabetes 1. Some women develop gestational diabetes late in pregnancy and it usually goes away after the birth of the child. 2. It is caused by the shortage of insulin caused by the hormones of pregnancy. 3. There are usually no symptoms. |
|
|
BASIC DIABETES 3 |
III.How is diabetes diagnosed?A.The fasting blood glucose test is most reliable for children and adults who are not pregnant.B.Otherwise, blood glucose levels are measured.IV.What is pre-diabetes?A.Pre-diabetes is when glucose levels are higher than normal, but not high enough to be diagnosed as diabetes.B.It is also known as Impaired Fasting Glucose (IFG) or Impaired Glucose Tolerance (IGT), depending on the method of testing used for diagnosis. Having both is a possibility.
|
|
|
Summary Diabetes |

Diabetes is a chronic, debilitating disease affecting every organ system. There are two major types of Diabetes: Type 1 and Type 2. Type 1 diabetes is an autoimmune disease in which a person’s pancreas stops producing insulin, a hormone that enables people to get energy from food. Type 1 diabetes usually strikes in childhood, adolescence, or young adulthood, but lasts a lifetime. People with Type 1 diabetes must take multiple injections of insulin daily or continuous infusion of insulin through a pump just to survive. Type 2 diabetes is a metabolic disorder in which a person’s body still produces insulin but is unable to use it effectively. Type 2 is usually diagnosed in adulthood and does not always require insulin injections. However, increased obesity has led to a recent “epidemic” in cases of Type 2 in young adults. Taking insulin does not cure any type of diabetes nor prevent the possibility of its eventual and devastating effects: kidney failure, blindness, nerve damage, heart attack and stroke.
|
|
|
HYPERGLYCEMIA: Diabetic EMERGENCY |

|
|
|
HYPOGLYCEMIA: diabetic Emergency |

Symptoms |
|
|
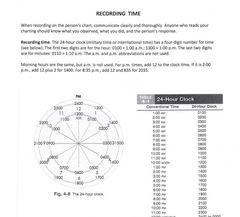
Recording Time |
|
|
|
supination |
Su |
|
|
syncope |
Sy |
|
|
trendelenburg position |
Tr |
|
|
vital signs |
Vs |
|
|
dorsal recumbent position |
Dr |
|
|
dorsiflexor gait |
D |
|
|
dorsiflexion |
D |
|
|
pitting edema |
Pe |
|
|
food pyramid |
Fp |
|
|
skin turgor |
St |
|
|
Miscellaneous Medical Terms |
Dys – bad, difficult, abnormal Phagia – to eat or consume Phasia – speaking (aphasia) Hemiplegia – ½ body Paraplegia – 2 limbs Quadriplegia – 4 limbs Homeostasis – a relative constancy in the internal environment adaptive responses that promote healthy survival. Alzheimer’s A = ADL changes B = Behavior changes C = Cognition changes 3 Stages I – mild/beginning forgetfulness and ABC’s II – middle/mental medication III – total care needed |
|

|
• Sudden numbness or weakness of the leg, arm, or face • Sudden confusion or trouble understanding • Sudden trouble seeing in one or both eyes • Sudden trouble walking, dizziness, loss of balance or coordination • Sudden severe headache with no known cause • Ask person to stick out their tongue. If tongue is “crooked”, if it goes to one side or the other, that is also an indication of a stroke. If someone shows any of these symptoms, immediately call 9-1-1 or emergency medical services. |
|
|
Systolic vs. Diastolic Blood Pressure |

Diastolic pressure occurs near the beginning of the cardiac cycle. It is the minimum pressure in the arteries when the pumping chambers of the heart — ventricles — fill with blood. Near the end of the cardiac cycle, systolic pressure, or peak pressure, occurs when the ventricles contract. As the heart beats, it pumps blood through a system of blood vessels, which carry blood to every part of the body. Blood pressure is the force that blood exerts on the walls of blood vessels. All or any of the events related to the flow or blood pressure that occurs from the beginning of one heartbeat to the beginning of the next is called a cardiac cycle. Problems in the cardiac cycle can cause low or high blood pressure
|
|
|
Good |
Done |

