![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
Which liver enzymes are produced in hepatocytes? Which are produced in the cells that line the bile canaliculi?
|
Hepatocytes: alanine transaminase (cytosol), aspartate transaminase (mitochondria).
Bile canaliculi cells: gamma-glutamyltransferase (GGT), serum alkaline phosphatase (ALP) |
|
|
Which liver enzymes will be increased in viral hepatitis?
|
ALT and AST are elevated. Generally, ALT is greater than AST, because ALT is a specific marker for liver cell necrosis. GGT, ALP, and bilirubin will be normal, but will rise later in the course of the disease.
|
|
|
What liver enzymes will be increased in alcoholic hepatitis?
|
AST > ALT, because AST is present in the mitochondria of hepatocytes and EtOH uncouples the mitochondria. EtOH also induces the P450 system which increases GGT.
|
|
|
What liver enzymes are increased in cholestasis?
|
ALP and GGT.
|
|
|
What is the cellular organelle that GGT (gamma-glutamyl transferase) is found in?
|
Smooth endoplastic reticulum. Therefore when the P450 system is increased, GGT is increased. Break down of alcohol, drugs (phenytoin, barbituates, etc.).
|
|
|
What are the three broad categories of causes of jaundice?
|
Unconjugated (CB<20%): increased production of UCB (increased urine UBG) or decreased uptake or conjugation of UCB (normal urine UBG).
Mixed (CB 20-50%): defect in uptake, conjugation, and secretion; viral hepatitis; increased in urine bilirubin and urine UGB. Obstructive (CB > 50): increase urine bilirubin, absent urine UBG. |
|
|
What is the defect in the following disorders:
1) Crigler-Najjar (type I and Arias) 2) Gilbert syndrome 3) Dubin-Johnson syndrome 4) Rotor's syndrome |
1) Deficiency of bilirubin glucuronyl transferase.
2) Minor reduction in glucuronyl transferase activity. 3) (AR) genetic defect in secretion of bilirubin into bile duct; black pigment 4) (AR) same as D-J but without the black pigment |
|
|
Baseline bilirubin in a patient is 1. You ask a patient to fast for 24 hours and they come back and their bilirubin is now 2.5 (more than double!). Diagnosis?
|
Fasting test to determine Gilbert syndrome: unconjugated type of hyperbilirubinemia; most common hereditary cause of jaundice.
|
|
|
Name some causes of extravascular hemolysis.
|
Pyruvate kinase deficiency, G-6-P dehydrogenase deficiency, sickle cell anemia, malaria, hereditary spherocytosis. Hemolytic disease of newborn (Rh or ABO). Crigler-Najjar syndrome (deficiency in glucuronyl transferase), Gilbert syndrome (defect in uptake of UCB), jaundice in newborn.
|
|
|
What effect does extravascular hemolysis of RBCs have on the following substances:
unconjugated bilirubin (UCB) conjugated bilirubin (CB) urobilinogen (UBG) AST |
UCB, CB, and UBG are all increased, thus, turning stool and urine darker. Hemolysis of RBCs cause an increase in AST.
|
|
|
How does viral hepatitis effect these substances:
UCB in blood CB in bowel CB in urine UBG in bowel UBG in urine |
Viral hepatitis (mixed): liver dysfunction involving uptake and conjugation of UCB, secretion of CB into bile ducts, and recycling of UBG.
UCB in blood - elevated CB in bowel - normal CB in urine - elevated (normally zero) UBG in bowel - normal UBG in urine - elevated |
|
|
How does an obstructive liver disease (gallstones) effect these substances:
UCB in blood CB in bowel CB in urine UBG in bowel UBG in urine |
UCB in blood - normal
CB in bowel - absent CB in urine - elevated (normally zero): dark urine. UBG in bowel - absent UBG in urine - absent |
|
|
Hyperbilirubinemia (causing icterus) can be due to an obstruction in the hepatobiliary circulation. What are some examples?
|
Decreased intrahepatic bile flow.
Primary biliary cirrhosis. Dubin-Johnson and Rotor's syndrome. Decreased extrahepatic bile flow: gallstone in common bile duct or carcinoma of head of pancreas. |
|
|
Patient presents with jaundice, epigastric pain and weight loss. History reveals the patient has pale stool. Examination reveal a palpable gallbladder (positive Courvoisier's sign). What is the gold standard test to diagnose this patient?
|
This patient has all the clinical features of a carcinoma of head of the pancreas. An increased CA19-9 is the gold standard tumor marker.
|
|
|
Besides liver enzymes, what test can be used to access hepatocyte function?
|
Serum albumin: hypoalbuminemia indicates cirrhosis.
Prothrombin time (PT): factors II,VII, IX, X are synthesized by the liver. Blood urea nitrogen (BUN): urea cycle is in the liver; decreased BUN indicates cirrhosis. Serum ammonia: ammonia is metabolized in the urea cycle; increased ammonia indicates cirrhosis or Reye syndrome. |
|
|
Which viral hepatitis is transmitted via fecal-oral route and can cause a fulminant hepatitis (very rare)? What family is this virus in?
|
Hepatitis A virus (HAV) is a naked icosahedral capsid (capsid is antigenic) with a positive ssRNA. Picornaviridae. Transmitted via fecal-oral. This virus does not cause chronic hepatitis. Vaccine is available.
|
|
|
What microscopic changes could be found in acute viral hepatitis?
|
Lymphocytic infiltrate with destruction of hepatocytes: apoptosis of hepatocytes (Councilman bodies).
|
|
|
Patient presents with a fever, painful hepatomegaly, jaundiced, and elevated levels of liver function enzymes. What is the most likely diagnosis?
|
Acute viral hepatitis. Hepatitis A is the most common viral hepatitis and cause of jaundice
|
|
|
What viral family does hepatitis B belong to and how is this virus contracted?
|
Hepatitis B is from the hepadna viridae, a dsDNA, enveloped icosahedral capsid. The intact virus is referred to as the Dane particle. Transmission occurs via parenteral, sexual, pregnancy, breast feeding.
|
|
|
Serology studies of HBsAg, Anti-HBsAg, HBeAG, Anti-HBeAg, and Anti-HBcAg are shown in the following patients (if not shown, assume neg.). What is the status of these patients:
1) HBsAg+, HBeAg+, Anti-HBcAg IgG 2) Anti-BsAg+, Anti-HBeAg+, Anti-HBcAg IgG 3) Anti-HBsAg+ 4) HBsAg+, Anti-HBeAg+, Anti-HBcAg IgG 5) HBsAg+, Anti-HBc IgM 6) Anti-HBc IgM |
1) Chronic HBV w/ high infectivity
2) Recovery from HBV 3) Immunized from HBV 4) Chronic HBV w/ low infectivity 5) Acute HBV 6) Window phase (serology gap between 4-5 months) |
|
|
When does hepatitis B surface antigen (HBsAg) appear after exposure in serology reports?
Persistence of HBsAg in serology for how long indicates chronic HBV? When does the window phase or serologic gap occur in the timeline of a HBV infection? |
2-8 weeks after exposure.
6 months. 4-5 months. This is the gap between HBsAg disappearing and appearance of Anti-HBsAg |
|
|
What are possible complications of a hepatitis B infection?
|
Chronic hepatitis (asymptomatic or symptomatic), fulminant hepatitis.
Co-infection with hepatitis D virus. Cirrhosis: fibrosis, nodules. Hepatocellular carcinoma: viral DNA incorporates into hepatocyte DNA and triggers malignant growth. Serum sickness prodrome. Polyarteritis nodosa. Membranous glomerulopathy. |
|
|
What viral family does Hepatitis C come from and how is it transmitted?
|
Flavivirus: + ssRNA, enveloped icosahedral capsid.
Transmitted via blood transfusion, needle sticks, sexual, and across the placenta. |
|
|
What test would determine that a patient is currently infective with Hep C? How would the results differ if the patient had recently recovered from Hep C?
|
Infection: + RIBA (recombinant immunoblot assay) and + HCV RNA (via PCR).
Recovery: + RIBA and - HCV RNA. |
|
|
What viral family does Hepatitis E belong to and how is it transmitted?
|
Caliciviridae: + ssRNA, naked icosahedral.
Transmitted via fecal-oral route. |
|
|
Is Anti-HCV IgG protective?
Is Anti-HAV IgG protective? Is Anti-HBV IgG protective? Is Anti-HEV IgG protective? |
HCV - no
HAV - yes HBV - yes HEV - yes |
|
|
Immigrant from Mexico presents to your office with a recent history of bloody diarrhea and abdominal pain. Examination of the stool reveals RBC in the cytoplasm of a trophozoites. Cysts are also present. Why should you also do a CT scan on this patient?
|
Entamoeba histolytica, a protozoa, is transmitted via the fecal-oral route. Most patients are asymptomatic carriers. Bloody diarrhea occurs when trophozoites penetrate the intestinal mucosa. CT scan should be performed because this protozoa can form a liver abscess (right lobe).
|
|
|
Patient presents with fever, right upper quadrant pain and jaundice. Liver enzymes also show raised ALP and GGT. What's the most likely diagnosis?
|
Ascending cholangitis due most often to E.coli or Klebsiella. This condition is characterized by inflammation of the bile ducts (cholangitis), infection and bile duct obstruction. Ascending cholangitis is the most common cause of multiple liver abscesses.
|
|
|
What playhelminth (flat worm) is contracted by the ingestion of fish and infects the common bile duct? Patients with this infection are also at a risk of cholangiocarcinoma.
|
Clonorchis sinensis (Chinese liver fluke).
|
|
|
Patient presents with abdominal pain, palpable liver mass, and biliary obstruction. CT scan reveal large cysts in the liver. You inform the patient that his dog transmitted the disease to him and that the cysts must be removed. What was your diagnosis and why must the cysts be removed?
|
This patient has sheepherder's disease. Infection with echinococcus granulosus. Rupture of these cysts can cause a massive anaphylactic reaction.
|
|
|
Miliary spread of what bacteria can result in granulomatous hepatitis?
|
Mycobacterium tuberculosis, histoplasma capsulatum.
|
|
|
What effect does schistosomiasis have on the liver?
|
Schistosomiasis is caused by shistosoma mansoni, a platyhelminth (flat worm), that penetrates through the skin. The intermediate host of this helminth is fresh water snails. The eggs of shistosoma incite a fibrotic response in the portal vein causing cirrhosis.
|
|
|
What serum markers could be found in a patient with autoimmune hepatitis?
What serum markers could be found in a patient with autoimmune primary biliary cirrhosis? |
Antinuclear antibody and anti-smooth muscle antibodies. Occurs mostly in younger women: fever, jaundince hepatosplenomegaly.
Antimitochondrial antibody and serum IgM. |
|
|
A biopsy of a liver in a neonatal hepatitis patient would reveal......
|
Multinucleated giant cells. This is an idiopathic disease. It is also associated with infections or errors of metabolism.
|
|
|
What triggers Reye's syndrome in children younger than four years of age?
What manifests clinically and whats the underlying pathology? |
Reye syndrome often follows chickenpox or influenza and salicylates. The mitochondria is damaged leading to an increase in serum ammonia and defective beta-oxidation. Clinical findings include vomiting, encephalopathy and hepatomegaly (fatty change).
|
|
|
Name two syndromes that can occur during pregnancy that results in liver disease?
|
Acute fatty liver of pregnancy: defect in beta-oxidation. Liver is typically small. Fetus must be removed/delivered.
Preeclampsia can lead to HELLP syndrome: hemolytic anemia with schistocytes, elevated serum transaminases, low platelets (due to DIC). Liver cell necrosis around portal triads. |
|
|
Define fulminant hepatic failure.
|
Acute liver failure with encephalopathy within 8 weeks of hepatic dysfunction. Causes: viral hepatitis (most common), acetaminophen, Reye syndrome.
|
|
|
Patient presents confused and jaundiced. His liver is rapidly shrinking, bilirubin is rapidly rising, PT is markedly high, and transaminases are falling. What is the mortality rate of patients with this condition?
|
This is fulminant hepatitis (most commonly caused by hepatitis B and D, sometimes E and rarely A). Patients who fall into a common > 80% chance of dieing.
|
|
|
What is the most common cause of centrilobular hemorrhagic necrosis?
|
Combine LHF (decreased cardiac output) and RHF (back up of systemic blood). Liver becomes enlarged with a mottled red appearance: nutmeg liver. Clinical findings: painful hepatomegaly, jaundice, and increased transaminases.
|
|
|
Peliosis hepatis is characterized by multiple blood filled cysts throughout the liver, resulting in sinusoidal dilation. What are the commonest causes of this rare vascular disease?
|
Bartonella henselae, causing bacillary angiomatosis, in AIDS patients.
Anabolic steroids. |
|
|
Budd-Chiari syndrome (occlusion of the hepatic veins or IVC) results in a liver which is grossly enlarged and tender, and severe intractable ascites is present. Heart failure signs are absent. What are the causes of this syndrome?
|
Hepatic vein-thrombosis: polycythemia vera (most common), oral contraceptive pills, and hepatocellular carcinoma.
|
|
|
Define hematobilia.
|
Blood in the bile in patients with trauma to the liver.
|
|
|
How does alcohol consumption lead to fatty change?
|
Metabolism of alcohol results in the excess production of NADH which stimulates the conversion of dihydoxyactone phophate to glycerol-3-phosphate. The end product of EtOH metabolism (acetone) is made into acetyl CoA which is used to make FA. The glycerol backbone and FA are combined to form TG's. Additionally, protein production is reduced therefore apolipoproteins are not produced. TG's accumulate in the liver.
|
|
|
What systems are used in the liver to breakdown alcohol?
|
EtOH (via alcohol dehydrogenase) is broken down to acetaldehyde.
Acetaldehyde (via aldehyde dehydregenase, non-inducible enzyme) is broken down to acetone. Acetaldehyde is also broken down by MEOS (an inducible system using P-450). This system produces radical oxygen species. |
|
|
What are the consequences of excess acetaldehyde in the body?
|
All the hangover symptoms and it also directly damages hepatocytes.
|
|
|
What are the microscopic findings in:
(1) Alcoholic fatty change (2) Alcoholic hepatitis |
1) Fatty accumulation in hepatocytes, no fever or neutrophilic leukocytosis
2) Fatty change with neutrophil infiltration, Mallory bodies (damaged intermediate filaments in hepatocytes), and perivenular fibrosis. |
|
|
What are the most common drug/toxin causes of these liver tumors:
1) Angiosarcoma 2) Liver cell adenoma 2) Hepatocellular carcinoma 4) Cholangiocarcinoma |
1) Vinyl chloride, arsenic, thorium dioxide
2) Oral contraceptive pills 3) Aflatoxin due to aspergillus mold 4) Thorium dioxide |
|
|
What are the most common drug/toxin causes of these liver disease:
1) Acute hepatitis 2) Cholestasis 3) Fatty change 4) Fibrosis |
1) Isoniazid, halothane, acetaminophen, methyldopa
2) Oral contraceptive pills (estrogen prevents bile secretion), anabolic steroids 3) Amiodarone, methotrexate 4) Amiodarone, methotrexate, retinoic acid |
|
|
Name the common causes of cholestatic liver disease, both extrahepatic and intrahepatic.
|
Extrahepatic: stones originating from the gallbladder, primary sclerosing pericholangitis, extrahepatic biliary atresia, carcinoma head of pancreas.
Intrahepatic: drugs (OC, anabolic steroids), neonatal hepatitis, pregnancy induced cholestasis (estrogen). |
|
|
What clinical and findings could find in obstructive, cholestatic, liver diseases?
What laboratory findings? |
Jaundice with pruritus, malabsorption, cholesterol deposits in the skin, and light colored stool. Liver is enlarged, green-colored. Bile ducts will be distended with bile.
Lab findings: CB > 50%, bilirubinuria, absent urine UBG, increase in serum ALP and GGT. |
|
|
Three major intrahepatic biliary tract disease are primary biliary cirrhosis, secondary biliary cirrhosis, and primary sclerosing pericholangitis. What are the defining characteristics of primary sclerosing pericholangitis?
|
Primary sclerosing pericholangitis is characterized by obliterative fibrosis of intrahepatic and extrahepatic bile ducts. It is predominantly a male disease (2:1) and 70% of patients will also have ulcerative colitis. Patients are at risk of cirrhosis and cholangiocarcinoma.
|
|
|
What are the three defining characteristics of cirrhosis?
|
(1) Bridging fibrous septae linking portal tracts and portal and tracts with hepatic veins.
(2) Parenchymal nodules containing proliferating hepatocytes encircled by fibrosis. (3) Disruption of the architecture of the entire liver. |
|
|
Describe the relationship betweeen Kuppfer cells and stellate cells during the inflammatory response that leads to cirrhosis.
|
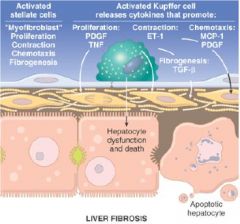
|
|
|
In terms of frequency, what are the most common causes of cirrhosis?
|
Alcoholic liver disease (60-70%)
Viral hepatitis (10%) Biliary diseases (e.g. primary biliary cirrhosis, 5-10%) Primary hemochromatosis (5%) Wilson disease, alpha-antitrypsin deficiency, cryptogenic cirrhosis, galactosemia |
|
|
What are the complications that occur in cirrhosis?
|
Hepatic failure, portal hypertension, ascites, hepatorenal syndrome, hyperestrinism, hepatocellular carcinoma.
|
|
|
What are some common clinical findings in hepatic failure and what test confirms these features?
|
Coagulation defects: inability to synthesize coagulation factors. PT.
Hypoalbuminemia: pitting edema. Decrease albumin. Hepatic encephalopathy: reversible metabolic disorder; increase in ammonia. Decrease BUN. Portal hypertension: Ascites: portal htn and secondary hyperaldosteronism. Hepatorenal syndrome. Hyperestrinism. |
|
|
Hepatic encephalopathy is characterized by altered mental status, disordered sleep rhythms, asterixis, coma, and death. What is the cause of this syndrome?
|
Hepatic encephalopathy is due to the persistence of toxic substance because of decrease liver function and portal hypertension (anastomoses). Ammonia is a key toxin that accumulates and appears to cause neurotransmitter dysfunction. GABA (inhibiotry) is raised. Ammonia also causes astrocytes to swell leading to cerebral edema.
|
|
|
What are the clinical manifestations of hyperestrinism due to hepatic failure?
|
Liver cannot degrade estrogen and 17-ketosteroids. Clinical findings include: gynecomastia, spider telangiectasia, female distribution of hair, palmer erythema, and hypogonadism.
|
|
|
Portal hypertensions (intrasinusoidal hypertension) results in anastomoses and ascites. What are the three main anastomoses?
|
1) Esophageal varices: left gastric vein - esophageal vein.
2) Caput medusa: paraumbilical vein - superficial and inferior epigastric veins. 3) Hemorrhoids: superior rectal vein - middle and inferior rectal veins. 4) Retroperitoneal hemorrhage: ?. Ascites: liver cannot metabolize ALD and doesn't produce albumin (decrease oncotic pressure). |
|
|
What is hepatorenal syndrome?
|
Renal failure without renal parenchymal disease due to hepatic failure. This condition is primarily due to a decrease in renal blood flow.
|
|
|
What is the pathogenesis of primary biliary cirrhosis? What is the epidemiology of this disease?
|
Primary biliary cirrhosis commonly occurs in women (6:1) between 40-50. It is an autoimmune granulomatous destruction of the bile ducts in the portal triads. Antibodies: anti-mitochondrial and anti-IgM.
|
|
|
Patient presents generalized pruritus followed by jaundice, pale stools, and dark urine. Examination reveals hepatomegaly, xanthomas. What autoimmune disorder could cause this patients condition?
|
Primary biliary cirrhosis. Further test could reveal anti-mitochondrial antibodies. Secondary biliary cirrhosis is a non-autoimmue condition that presents the same.
|
|
|
Why are women less likely to show symptoms of hereditary hemochromatosis until there elderly years?
|
This autosomal recessive disorder is characterized by an increase in iron retention. Menses causes a loss of iron which provides protection from hemochromatosis.
|
|
|
What is the defect in hereditary hemachromatosis?
|
HFE gene product is damaged. HFE product facilitates the binding of plasma transferrin to Tf-receptor on intestinal cells. The defective HFE is maximally stimulated, thus, absorption of iron is at a max. (?).
|
|
|
What are some causes of secondary hemachromatosis (hemosiderosis)?
|
Blood transfusions: sickle cell and beta-thalassemia patients.
Alcohol abuse (EtOH increases iron absorption). Well water (iron pipes) |
|
|
Iron cause free radical damage to tissue and subsequent fibrosis. What are the main sites of deposition in the body?
|
Liver: in hepatocytes.
Pancreas: (1) bronze diabetes - damage beta cells. (2) exocrine pancreas - leading to malabsorption. Skin: increases melanin production. Heart: restrictive cardiomyopathy. Joints: degenerative joint disease. |
|
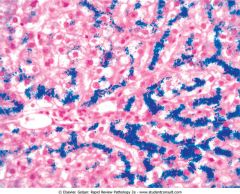
Prussian blue-stained section of the liver.
|
Hereditary hemochromatosis.
|
|
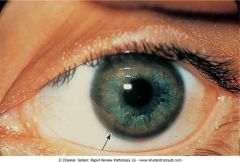
Kayser-Fleischer ring are characteristic of ________.
|
Wilson's disease. Autosomal recessive disorder of ceruloplasmin leading to accumulation of copper.
|
|
|
What are the consequences of the mutation that occurs in Wilson's disease? How does this disease present clinically?
|
Defective hepatocyte transport of copper into bile for excretion. Decreased synthesis of ceruloplasmin. Ceruloplasmin binds 90%-95% of the total serum copper concentration.
CNS symptoms: deposits in putamen resembles parkinsonism, copper in cerebral cortex leads to dementia. |
|
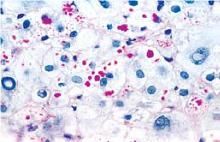
Periodic acid-Schiff stain of the liver.
|
Alpha-antitrypsin deficiency. Red granules.
|
|
|
How does alpha-antitrypsin deficiency cause cirrhosis?
|
PiZZ (wild type = PiMM) variant leads to a defect in the packing and transporting of AAT. AAT builds up to toxic levels in the hepatocytes causing liver damage.
|
|
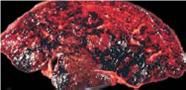
Liver. What hepatic circulatory disorder could lead to this?
|
Thrombosis of major hepatic veins has caused extreme blood retention in the liver: Budd-Chiari syndrome.
|
|
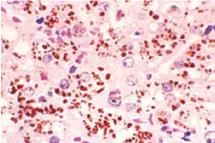
H&E of the liver. Patients with this syndrome will be asymptomatic and have a normal life expectancy.
|
Dubin-Johnson syndrome. Decrease in excretion of biliruin glucuronides across the canalicular membrane.
|
|
|
Female patient, previously on oral contraceptives, develops a liver cell adenomas. What is your primary concern?
|
This is a highly vascularized benign tumor that has a tendency to rupture during pregnancy causing an intraperitoneal hemorrhage.
|
|
|
Female patient, 60, presents with a fever and hepatomegaly. History reveals she has had hepatitis B for many years. Lab work up shows elevated alpha fetoprotein. Diagnosis?
|
Hepatocellular carcinoma.
|
|
|
What are the risk factors for hepatocellular carcinoma?
|
Hep B and C.
Aflatoxin (from aspergillus mold). Hemochromatosis, alcoholic cirrhosis. Primary biliary cirrhosis, AAT deficiency. |
|
|
What is the most common liver tumor of young childhood that is fatal unless resected?
|
Hepatoblastoma.
|
|
|
What is a choledochal cysts?
|
Congenital dilations of the common bile duct, presenting most often in children < 10 years old. Present as abdominal pain with intermittent jaundice. Increased incidence of cholelithiasis, cholangiocarcinoma, and cirrhosis.
|
|
|
What is Caroli disease and what is the inheritance?
|
Autosomal recessive disease associated with polycystic kidney disease. Caroli is characterized by segmental dilation of intrahepatic bile ducts. Increase risk of cholangiocarcinoma.
|
|
|
What are the risk factors for cholangiocarcinoma?
|
Primary sclerosing pericholangitis.
Clonorchis sinensis (Chinese liver fluke). Thorium dioxide. Choledochal cyst and Caroli disease. |
|

What are the risk factors for this particular cholelithiasis?
|
Yellow cholesterol stones with bile pigment staining the center. Risk factors: female over 40, obesity, oral contraceptive pills, rapid weight loss, lipid-lowering drugs, Native Americans.
|
|
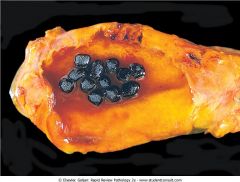
These stones in the gallbladder are a sign of what?
|
Black pigment stones (calcium bilirubinate) are a sign of extravascular hemolysis. Brown pigment stones (not pictured) are a sign of infection in the common bile duct.
|
|
|
Formation of cholesterol gallstones include four simultaneous defects. What are they?
|
Bile must be supersaturated with cholesterol (in excess of lecithin and bile salts).
Gallbladder hypomotility (excess free cholesterol is toxic to the gallbladder). Cholesterol nucleation. Mucus hypersecretion traps the cholesterol crystals. |
|
|
Patient presents with colicky epigastric pain, slight fever, and vomiting shortly after a meal. The pain then radiates to the right scapula. Diagnosis?
|
Acute cholecystitis. 90% of these cases are due to a stone in the cystic duct. Increased intraluminal pressure and ischemia to gallbladder wall. Lecithin is also converted to lysolecithin which is toxic. Mucosal ulceration can predispose to a infection (normally E. coli).
|
|
|
What portion of the bile duct system do these conditions involve (define them):
1) Cholangitis 2) Choledocholithiasis 3) Ascending cholangitis 4) Biliary atresia 5) Cholestasis of pregnancy 6) Caroli 7) Choledochal cysts |
1) Bacterial infection of the bile ducts (any part).
2) Presence of stones within the bile ducts of the biliary tree. 3) Infection of intrahepatic biliary ducts. 4) Obstruction of the lumen of the extrahepatic biliary tree within the first 3 months of life. 5) Estrogen inhibits intrahepatic bile secretion. 6) Segmental dilation of intrahepatic bile ducts. 7) Congenital dilations of the common bile duct. |

