![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
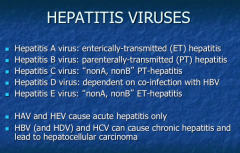
Identify with Hepatitis A-E:
1. nonA, nonB PT-hepatitis 2. nonA, nonB ET-hepatitis 3. dependent on co-infection with HBV 4. enterically-transmitted (ET) hepatitis 3. parenterally-transmitted (PT) hepatitis
Which two cause ACUTE hepatitis only? Which three cause chronic hepatitis and lead to hepatocellular carcinoma? |
|
|
|
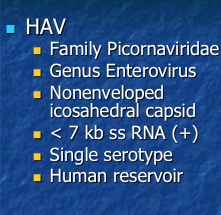
HAV: Which family? Which genus? What type of capsid? Large or small? RNA or DNA? How many serotypes? What is the reservoir? |
|
|
|
HEV: Which family? Which genus? What type of capsid? Large or small? RNA or DNA? How many serotypes? What is the reservoir?
Most prevalent in which countries (developing or developed)? Is there a high fatality rate in pregnant women? |
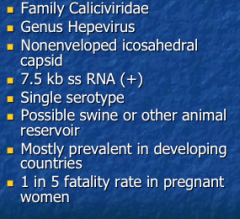
Really pay attention to the 1 in 5 fatality rate in pregnant women! |
|
|
What is the most common age of HAV diagnosis? What proportion of population has had HAV? |
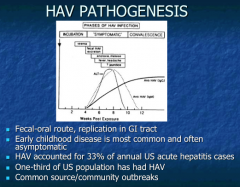
Short incubation period with Hep A (again, people are infectious before they show symptoms). |
|
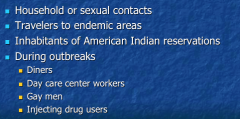
These groups are all at risk for what? |
HAV
NOT CONSIDERED A SEXUALLY TRANSMITTED DISEASE!
Specific sorts of groups during outbreaks! |
|
|
How often does a hepatitis A outbreak occur? |
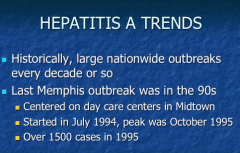
|
|
|
Why have HAV numbers declined? |
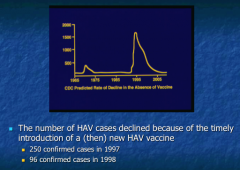
|
|
|
What is the HBV virus type? Enveloped or non enveloped? What is it called? DNA or RNA? |
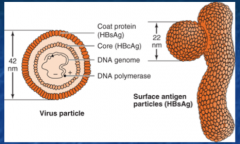
Hepadnavirus
HepaDNAvirus Only hepatic DNA virus.
Very small genome
Surface antigen attachment protein acts as a smoke screen for immune system, allows to attach to hepatic cells and gain entry. |
|
|
What are the five major proteins of HBV? (enzyme, surface antigen, core antigen, serologic marker, one that influences gene expression) |
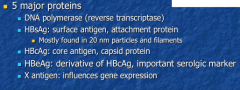
Know the serology for HepB. |
|
|
Draw the replication process of HBV.
What is used as a template for reverse transcription? What then integrates into genome? How is the genome mostly maintained in chronic infections? |
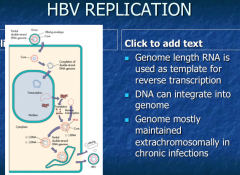
1. Completion of double stand DNA 2. Make full length of mRNA (reverse transciptase comes in and transcribes as DNA = negative sense strand) => RNA chops up and uses as a primer, then synthesizes the second positive sense strand (partially complete DNA like the original).
Random integration into human genome => could lead to cancer. Don't have to know to this level of detail. |
|

|
|
|
|
What "fluids" contain HBV and are involved in its transmission?
What is the route of transmission? |
IS CONSIDERED TO BE A SEXUALLY TRANSMITTED DISEASE.
At risk groups = MSM, injection drug users, healthcare workers, hemophiliacs, Asian-Americans, prison populations. |
|
|
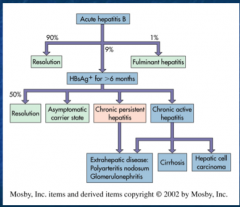
What is the pathogenesis of HBV?
When should it resolve? What is it considered if not by that point? What will it progress to? |
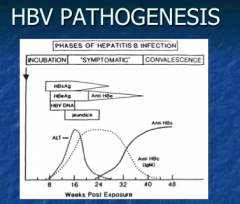
If not resolved in 6 months => chronic => asymptomatic until cirrhosis or HCC appears |
|
Identify:
IgM Anti-HBc Anti-HBe Anti-HBc HBsAg Anti-HBs HBeAg |
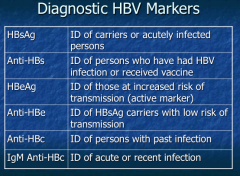
KNOW THIS! |
|
|
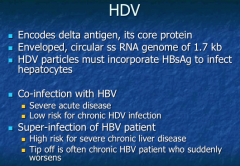
HDV: Enveloped or nonenveloped? Must incorporate HBsAg to infect hepatocytes?
What is the difference between a co-infection with HBV and a super-infection of HBV? (which is acute and low risk for HDV infection, which is high risk for severe chronic liver disease and tip off is often chronic HBV patient who suddenly worsens)? |
|
|
|
What family does HCV belong to? What type of capsid? RNA or DNA genome? |
|
|
|
What are the six major subtypes of HCV? Which two are the most common in the US? |
|
|
|
What age group is the US has the highest incidence of HCV?
|

Alcohol is especially a problem with hepatitis C. |
|
|
HCV: Are the acute infections milder or worse than HBV?
Why do chronic patients have multiple bouts?
|
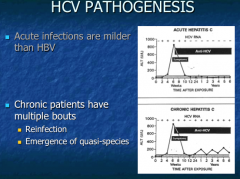
Quasi-species. Immune system attacks and other type builds ups. |
|
|
Are hepatitis viruses cytologic? What leads to liver disease? |
|
|
|
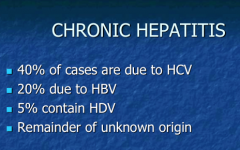
Chronic hepatitis: What percent of cases are due to HCV? What percent due to HBV? What percent contain HDV?
|
|
|
|
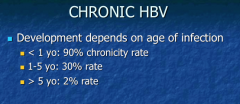
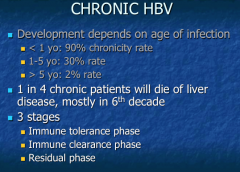
What does development of chronic HBV depend on? Which age group has a higher chronicity rate? |
|
|
|
What percent of patients with chronic HBV will die of liver disease? In what decade?
What are the three stages? |
|
|
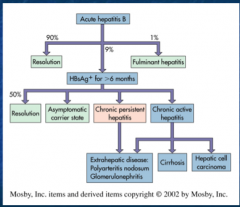
HBV summary |
HBV summary |
|
|
What percent of untreated HCV will lead to chronic infection? |
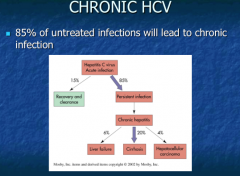
|
|
|
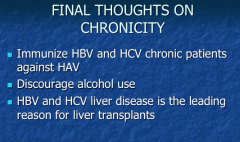
Should you immunize HBV and HCV chronic patients against HAV? Discourage the use of which fun activity? What are the two leading causes of liver transplants? |
|
|
|
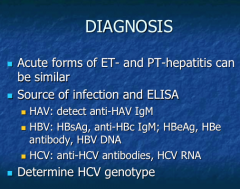
What can you detect for diagnosis of HAV? What about HBV? HCV?
|
|
|
|
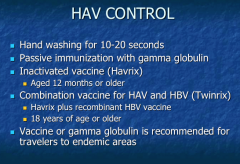
What is the vaccine for HAV? What ages? Is there a combination for A and B? |
|
|
|
|
|

|
|
|
|
HAV would seem to be a candidate for eradication, at least in developed nations. What conditions and properties of HAV make it a viable candidate? Why is HAV eradication not a high priority? |
There is only one serotype which facilitates making a good vaccine. Humans are the only reservoir.
Mostly self-limiting (rarely fulminant). Infectious before you are symptomatic (makes it problematic for eradication). Not really a very high level of infection. |
|
|
Risk factors of HAV? (question stem in class)
|
Kid in daycare Social drinking in restaurants Age (28) |
|
|
Entecavir and tenofovir are nucleoside analogs that inhibit HBV replication. Which polymerase is inhibited by these drugs and what property of the polymerase is exploited for antiviral purposes? |
Reverse transcriptase activity Hep B encodes polymerase that has reverse transcriptase activity.
Many of the same HIV drugs can also treat HBV but not HCV because HCV is RNA virus and does not have reverse transcriptase. |
|
|
What would be an adverse effect of HBV treatment drugs? |
Toxicities arise from action on polymerase (not specific for just viral polymerase). |
|
|
62 yo man in need of liver transplant. Lost blood, history of alcohol abuse, Right upper quadrant pain for many years as adult.
What other medical history is likely? |
Blood transfusion = more likely to contract from a blood transfusion (didn't start screening for C until 1990s for C). Hep C Cirrhosis
Most people with Hep B don't have symptoms for many years. If it's C, there will be flare ups often like in this case. |
|
|
Why does it take numerous years for complications such as hepatocellular carcinoma to develop in HBV or HCV patients? |
They do not CAUSE cancer via protooncogenes; rather, cancer arises from slow destruction of liver over years => replication of liver cells => accumulation of mutations with age => cancer. |
|
|
In pharm, why would you use any other drugs besides tenofovir and entecavir? |
Resistance! |
|
|
Why does chain termination occur with some drugs? |
Drug is incorporated and lacks 3-OH group => chain termination. |
|
|
What is the big picture of all Hep B drugs (ADME slide)?
What patients should you worry about? |
Secreted unchanged in the urine => no drug-drug interactions via CYP.
May need to make dose adjustment in patient with renal dysfunction. |
|
|
What is located in the renal AND hepatic cells? (in regards to toxicity) |
Mitochondrial DNA which has very similar enzyme to that which is inhibited by tenofovir => toxicities |
|
|
Bone pain, renal toxicity... which drug? |
Tenofovir |
|
|
What is the difference between interferon alpha 2b and 2a? |
Difference in one amino acid... not much difference in drug action. |
|
|
What are interferon, ribavirin both associated with in terms of adverse effects? |
Anemia
|
|
|
Which is associated with hemolytic anemia? How will it present? |
Ribaviran
Jaundice, dark urine, schistocytes on smear |
|
|
Why does HCV have increased resistance? |
High mutation rate because it is an RNA virus. |
|
|
What is the difference between protease inhibitors and the drugs like tenofovir in terms of metabolism? |
Protease inhibitors => substrates for CYP3A4 and p-gp. Changes in these components can change oral bioavailability.
Lots of drugs (phenytoin, etc.) will upregulate p-gp => decreased levels of the protease inhibitors. |

