![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
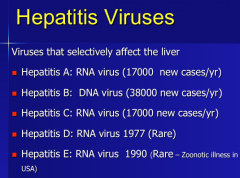
What is the most common strain of hepatitis? |
|
|
|
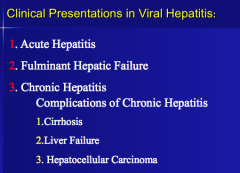
What are the three general presentations in viral hepatitis? What are the three complications of chronic hepatitis? |
|
|
|
Which virus cause acute hepatitis? What percent and which virus type lead to fulminant liver failure?
Which viruses cause chronic hepatitis? |
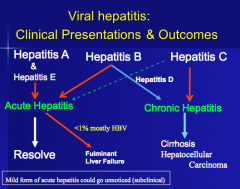
Most B in US is acute but can progress to chronic. |
|
|
Which strains usually cause acute hepatitis in the US? Which strain associated with zoonosis? Which strain with IV drug users?
How will the AST/ALT, bilirubin, prothombin time be affected?
What does a very high INR indicate? |
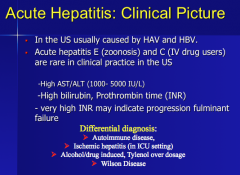
Diagnosed by AST/ALT and high IgM |
|
|
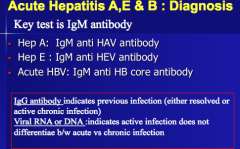
The diagnosis of acute HAV infection is confirmed during the acute or early convalescent phase of infection by the presence of __ antibodies to HAV (__ anti-HAV). __ anti-HAV is generally present 5-10 days before the onset of symptoms and is no longer detectable in the vast majority of patients __ months later. __ anti-HAV, which also appears early in the course of infection, remains detectable for the lifetime of the individual and confers lifelong protection against infection. Commercial tests are available for the detection of __ and total (IgM and IgG) anti-HAV in serum. |
The diagnosis of acute HAV infection is confirmed during the acute or early convalescent phase of infection by the presence of IgM antibodies to HAV (IgM anti-HAV). IgM anti-HAV is generally present 5-10 days before the onset of symptoms and is no longer detectable in the vast majority of patients 6 months later. IgG anti-HAV, which also appears early in the course of infection, remains detectable for the lifetime of the individual and confers lifelong protection against infection. Commercial tests are available for the detection of IgM and total (IgM and IgG) anti-HAV in serum. |
|
|
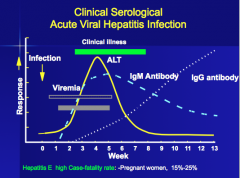
In infected persons, HAV replicates in the liver, is excreted in __, and is shed in the __. Peak infectivity occurs during the 2-week period before onset of jaundice or elevation of liver enzymes, when the concentration of virus in stool is __. The concentration of virus in stool declines after __ appears. Children and infants can shed HAV for longer periods than adults, up to several months after the onset of clinical illness. Chronic shedding of HAV in feces does not occur; however, shedding can occur in persons who have __ illness. Viremia occurs soon after infection and persists through the period of liver enzyme (alanine aminotransferase [ALT]) elevation. |
In infected persons, HAV replicates in the liver, is excreted in bile, and is shed in the stool. Peak infectivity occurs during the 2-week period before onset of jaundice or elevation of liver enzymes, when the concentration of virus in stool is highest. The concentration of virus in stool declines after jaundice appears. Children and infants can shed HAV for longer periods than adults, up to several months after the onset of clinical illness. Chronic shedding of HAV in feces does not occur; however, shedding can occur in persons who have relapsing illness. Viremia occurs soon after infection and persists through the period of liver enzyme (alanine aminotransferase [ALT]) elevation. |
|
|
HAV RNA can be detected in the __ and stool of most persons during the __ phase of infection by using nucleic acid amplification methods, such as __, and nucleic acid sequencing has been used to determine the relatedness of HAV isolates. These methods, however, are available in only a limited number of research laboratories and are not used generally for diagnostic purposes. |
HAV RNA can be detected in the blood and stool of most persons during the acute phase of infection by using nucleic acid amplification methods, such as PCR, and nucleic acid sequencing has been used to determine the relatedness of HAV isolates. These methods, however, are available in only a limited number of research laboratories and are not used generally for diagnostic purposes. |
|
|
|
|
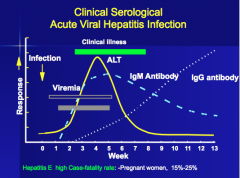
|
What is the most common outcome of acute hepatitis?
Which strain often professes to chronic infection?
Which stain can cause fulminant liver failure? |
|
|
|
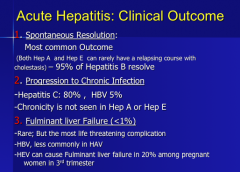
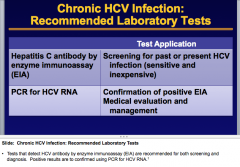
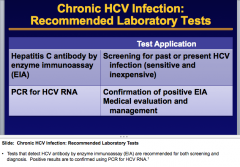
What is the KEY test for acute hepatitis A, E, and B diagnosis?
Which antibody indicates PREVIOUS infection? What indicates active infection but DOES NOT differentiate between acute vs. chronic infection. |
|
|
|
What is the most serious complication of acute viral hepatitis? Which strains usually cause this? (one in pregnancy also) What is the presentation (think brain effects specifically)? What is the only cure? |
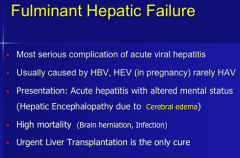
Acute hepatitis + confusion = fulminant hepatic failure |
|
|
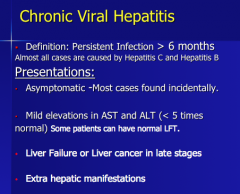
What is the definition of chronic viral hepatitis?
How does it present?
Mild elevations of what two labs?
What serious conditions can occur in late stages? |
|
|
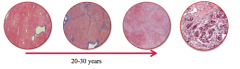
Identify normal, fibrosis, cirrhosis, HCC
What are four things that can accelerate fibrosis? |
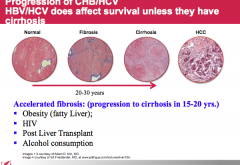
30 years to progress to cirrhosis. |
|
|
Which race is 2.7 times more likely to develop HCC and 2.4 times more likely to die from HCC? |
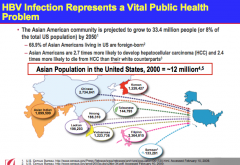
Highest rates of Hep B are in far east countries (China, india, etc.), in the US it is on the West Coast. |
|
|
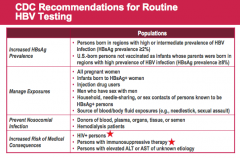
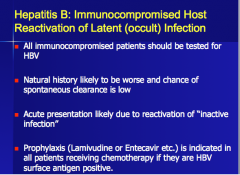
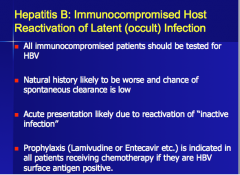
Which group of patients with HBV experience an increased risk of medical consequences? |
|
|
|
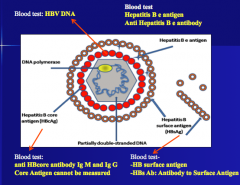
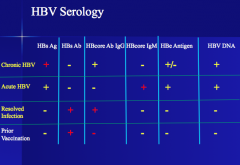
What are six possible blood tests for HBV? Can the core antigen be measured? |
|
|
|
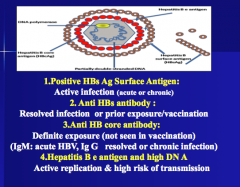
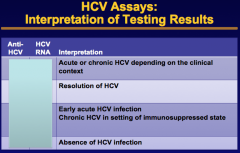
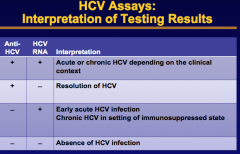
What will indicate active infection (acute or chronic)? What will indicate resolved infection or prior exposure/vaccination? What will indicate definite exposure? (which one for acute and which for resolved or chronic) What will indicate active replication and high risk of transmission?
1. Anti HBs antibody 2. Anti HB core antibody 3. Hepatitis B e antigen and high DNA 4. Positive HBs Ag surface antigen |
|
|
Complete |
|
|
|
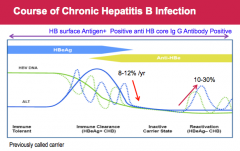
The phases of chronic HBV infection consists of four successive phases: |
The phases of chronic HBV infection consists of four successive phases: |
|
|
|
|
|
Not all patients go through all the four phases. The immune clearance phase is most common in young __ patients with perinatally acquired HBV infection. Some patients remain in the inactive carrier phase with no evidence of reactivation, these patients have better prognosis than those who develop reactivation. The immune clearance phase and reactivation phase may be prolonged with recurrent exacerbations of hepatitis and fluctuations in serum HBV DNA levels. |
Not all patients go through all the four phases. The immune clearance phase is most common in young Asian patients with perinatally acquired HBV infection. Some patients remain in the inactive carrier phase with no evidence of reactivation, these patients have better prognosis than those who develop reactivation. The immune clearance phase and reactivation phase may be prolonged with recurrent exacerbations of hepatitis and fluctuations in serum HBV DNA levels. |
|
|
When do you treat chronic HBV (two things)? |
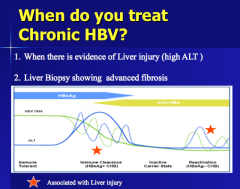
1. When evidence of liver injury. 2. When there is evidence of advanced fibrosis. |
|
|
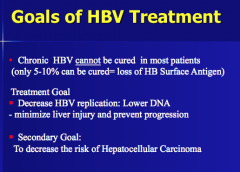
Can chronic HBV be cured in most patients? What is the goal of treatment? What is the secondary goal? |
|
|
|
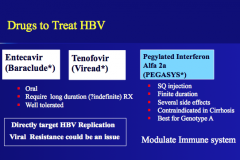
What are three drugs to treat HBV?
Which two are oral, require a long duration, and are well tolerated?
Which one is SQ, has finite duration, several side effects, contraindicated in cirrhosis, and best for GENOTYPE A? |
|
|
|
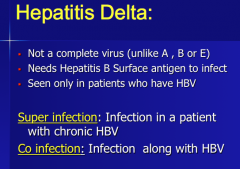
Is hepatitis D a complete virus? What does it need to infect? Seen only in patients who have what other hepatitis?
What are the two infections types? |
|
|
|
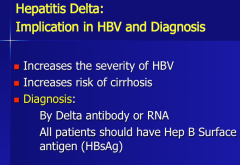
What is the effect of hepatitis delta on the severity of HBV and the risk of cirrhosis?
How can you diagnose it? What should all patients have? |
|
|
|
What is the most common chronic viral hepatitis in the US? |
Hepatitis C
"C for chronic" |
|
|
How many people in the US have chronic hep c infection? |
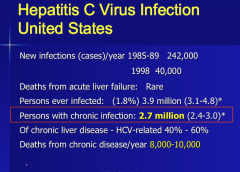
|
|
|
|
|
|
|
|
|
|
|
|
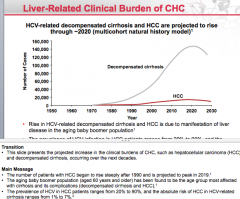
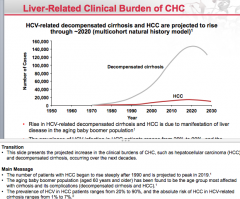
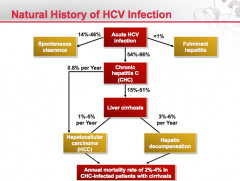
Draw out the natural history of hepatitis C infection from acute infection to development of disease complications. |
|
|
|
|
|
|
|
|
|
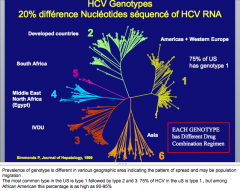
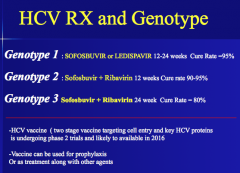
How many HCV genotypes are there? 75% in the US are which type? |
|
|
|
Draw the HCV life cycle. |
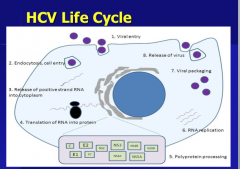
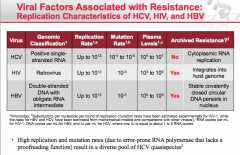
Hepatitis C always stays outside the nucleus. |
|
|
Is HCV curable with treatment? What can you use? |
|
|
|
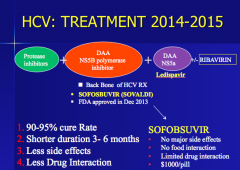
What are the three-four drug types used for HCV treatment?
Which drug has no major side effects, no food interaction, limited drug interactions, and is $1,000 per pill? |
|
|
|
Which drug is this?
|
Havaroni
Indicated for chronic hep c (type 1) infection in adults |
|
|
What two drugs are used to treat type 1 with a cure rate of 95%
Which two drugs for types 2 and 3? |
|
|
Complete |
|
|
|
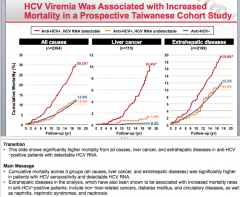
Does achieving sustained virologic response result in reductions in HCC incidence? |
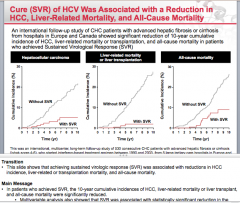
Yep |
|
Just be aware. |
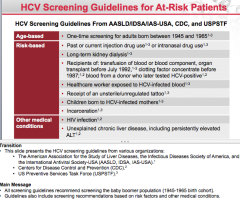
Transition Main Message |
|
|
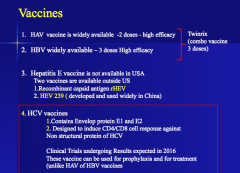
Is there a hepatitis A vaccine? Hepatitis B vaccine?
What envelope proteins does the HCV vaccine contain? What type of response will it induce against non structural protein of HCV? |
|
|
|
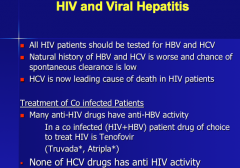
All HIV patients should be tested for which two hepatitis viruses? Why?
What is the leading cause of death tin HIV patients?
Do many anti-HIV drugs have anti-HBV activity? |
|
|
|
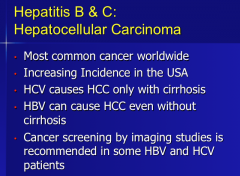
What is the most common cancer worldwide? Which hepatitis causes HCC only with cirrhosis? Which can cause HCC without cirrhosis? |
|
|
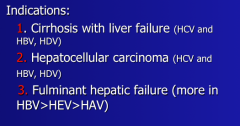
These are all indications for what? |
Liver transplantation in viral hepatitis |
|
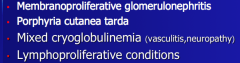
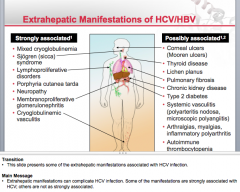
What are all of these associated with? |
Extra hepatic manifestations in viral hepatitis |
|
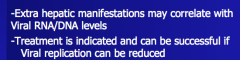
|
Do extra hepatic manifestations correlate with viral RNA/DNA levels? When is treatment indicated and can be successful? |
|
|
Look over |
|
|
|
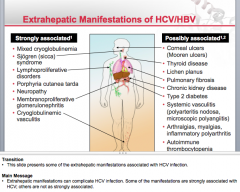
What are three other viral infections that can cause acute hepatitis?
What range will the ALT and AST be in? Are most self-limiting? Serious infections can result in which patients? |
CMV EBV Herpes |
|
|
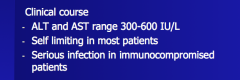
What are the clinical symptoms of CMV hepatitis? How will the ALT and AST change?
How can diagnose? What is the treatment (and prophylaxis) |
|
|
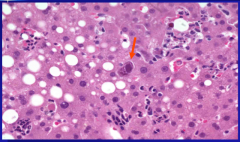
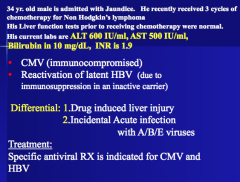
What is the arrow pointing to? What is the condition? |
Inclusion bodies
CMV hepatitis |
|
|
|
|
|
|
|
|
58 year old white male No symptoms No risk factors Everything looks normal
What test should he get? |
HCV antibody (based on the screening guidelines). |
|
|
32 yo w/ jaundice Drink 6 pack beer during weekends Icterus and mild upper Rt quadrant pain BMI 31 Normal liver ultrasound but stones seen in gall bladder ALT 1500, AST 1400, Bilirubin 12
|
Acute hepatitis E |
|
|
22 yo medical student seen for checkup Born in US, parents from Taiwan Liver function tests normal Hepatitis B surface antigen positive HBcore IGG antibody positive HBV DNA very high HBe antigen positive => previously vaccinated for hep A and B |
He's in the immune tolerant stage! No treatment
Chronic HBV immune tolerant stage |
|
|
24 yo jaundice Active IV drug user High AST/ALT/bilirubin => acute hepatitis
Acute hepatitis C
What is the best management for this patient? |
Just wait, most people will resolve Repeat HCV RNA in 3 months |
|
|
50 year ol referred for HCV NO medical history HepC positive, HCV RNA negative HB surface antibody positive
What do you do?
Exposed to hepatitis C but does not have active infection. |
No further tests. |
|
|
32 yo w/ history of HBV presents with jaundice Entecavir regularly Recent traveled to mediterranean countries and uses heroin Chronic hepatitis B with acute hepatitis.
What is most likely cause of present illness? |
Super infection with Hepatitis Delta |

