![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
Name 4 chemical (serum or urine) markers that are increased with hemolysis.
|
LDH, indirect bilirubin, urobilinogen, plasma free hemoglobin
|
|
|
What is the mechanism the causes esophageal spasm and nonhealing skin ulcers?
|
Free hemoglobin scavenges nitric oxide.
|
|
|
On which chromosome are alpha globin chains encoded? Beta globins?
|
Chromosomes 16 and 11, respectively.
|
|
|
Name the types of beta globin chains.
|
Epsilon (embryonic).
Gamma (fetal, subtypes A and G) Delta (adult) Beta (adult) |
|
|
Name the types of alpha globin chains.
|
Zeta (embryonic)
Alpha (adult, subtypes 1 and 2) |
|
|
Describe the postembryonic Hemoglobin molecules Hgb A, Hgb A2, and Hgb F.
|
Hgb A = alpha-beta
Hgb A2 = alpha-delta Hgb F = alpha-gamma |
|
|
What effects does 2,3-BPG have on the oxygen-binding affinity of hemoglobin?
|
It decreases oxygen affinity.
|
|
|
What differentiates thalassemia major from minor?
|
Thalassemia major is used to denote transfusion-dependence.
|
|
|
What contributes to the hypercoagulability of thalassemia?
|
RBC membrane damage with increased surface expression of anionic phospholipids; platelet activation; changes in hemostatic regulatory proteins.
|
|
|
There is an increased incidence of what infection associated with iron overload?
|
Yersinia enterocolitica bacteremia.
|
|
|
Other than target cells, what finding on peripheral smear is characteristic of thalassemia? Are the abnormal findings on peripheral smear absent after splenectomy?
|
Basophilic stippling (as well as anisopoikilocytosis). The abnormal findings increase after splenectomy.
|
|
|
What is the expected level of Hgb F in patients with beta thalassemia trait? What is the expected level of Hgb A2?
|
4-7% for Hgb F, above 3.5% for Hgb A2.
|
|
|
In beta thalassemia major, at what level of ferritin is iron chelation therapy initiated?
|
1000 mcg/dL
|
|
|
What is the role of HSCT in beta thalassemia?
|
Over 1,000 patients have been treated with stem cell transplant and most have been cured.
|
|
|
Why is alpha thalassemia more heterogenous than beta thalassemia?
|
Because there are 2 copies of the alpha globin gene in each chromosome 16, providing for more combinations of normal and abnormal gene products.
|
|
|
How common is the silent carrier state of alpha thalassemia in African Americans?
|
Present in 1 in 3.
|
|
|
Which is more common in Asians vs Africans or Mediterranean peoples, alpha thalassemia which is --/aa or -a/-a?
|
--/aa is more common in Asians, whereas the trans configuration is more common in Africa/Mediterranean peoples
|
|
|
Which hgb is a a common nondeletion form of alpha+ thalassemia common in Southeast Asia, and results in abnormally elongated alpha chains?
|
Hgb Constant Spring.
|
|
|
What is the term for the hgb formed by excess gamma chains in alpha thalassemia?
|
Hgb Bart. This results in hydrops fetalis.
|
|
|
What is the term for the hgb formed by excess beta chains in alpha thalassemia?
|
Hgb H.
|
|
|
Why does alpha thalassemia not result in the severe ineffective erythropoiesis characteristic of beta thalassemia?
|
Hgb Bart and Hgb H are more soluble than the Hgbs associated with beta thalassmia.
|
|
|
What is the clinical difference between patients with Hgb Bart and Hgb H, and what is the underlying pathophysiology?
|
Hgb Bart is very soluble but has such a high oxygen affinity that it does not deliver oxygen to tissue, leading to hypoxia, edema, heart failure and death. Hgb H is unstable; in precipitates and cells are hemolyzed, causing a moderatlely severe hemolytic anemia.
|
|
|
What is the expected Hgb A:S ratio in patients with sickle cell trait?
|
60:40
|
|
|
Coexistence of alpha thalassemia with sickle cell disease does what to the risk of stroke and the overall severity of hemolysis?
|
Sickle-cell/alpha thal. reduces risk of CVA and severity of hemolysis.
|
|
|
How does the A:S ratio and peripheral smear finding help differentiate between sickle cell trait and HgbS/beta+ thal?
|
A:S is 60:40 in sickle trait and 15:85 in S/B+ thal. Microcytosis, target cells, anemia and symptoms occur only with S/B+ thal.
|
|
|
What is the RBC life span in sickle cell disease? What is the expected baseline Hgb range?
|
10-25 days. Hgb usually falls between 6-9 g/dL.
|
|
|
What is another mechanism of sudden anemia in sickle cell disease other then aplasia/bone marrow suppression?
|
Sequestration, usually splenic but hepatic is also possible.
|
|
|
What are typical findings on peripheral smear with Hgb SC disease?
|
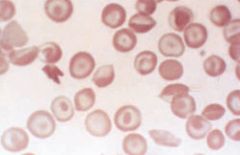
No irreversibly sickled cells; large numbers of target cells; dense; contracted, folded cells containing aggregated and polymerized Hgb.
|
|
|
Incentive spirometry has what effect in patients with sickle cell pain crisis presenting with chest or back symptoms?
|
Reduces pulmonary complications.
|
|
|
Is blood transfusion indicated in the treatment of routine painful episodes in sickle cell patients>
|
No.
|
|
|
Which types of sickle cell crisis events require exchange transfusion? What is the target Hgb S level and Hgb level?
|
Stroke, ocular events, severe acute chest syndrome. Goal is to get <30% Hgb S and overall Hgb to 9-10. Transfusion also have a role in preventing recurrent stroke, treating high-output heart failure, and treating osteomyelitis.
|
|
|
Incentive spirometry has what effect in patients with sickle cell pain crisis presenting with chest or back symptoms?
|
Reduces pulmonary complications.
|
|
|
Is blood transfusion indicated in the treatment of routine painful episodes in sickle cell patients>
|
No.
|
|
|
Which types of sickle cell crisis events require exchange transfusion? What is the target Hgb S level and Hgb level?
|
Stroke, ocular events, severe acute chest syndrome. Goal is to get <30% Hgb S and overall Hgb to 9-10. Transfusion also have a role in preventing recurrent stroke, treating high-output heart failure, and treating osteomyelitis. Hgb 11-12 or Hgb S over 30% can cause hyperviscosity.
|
|
|
Are exchange transfusions part of the normal treatment of sickle cell patients with uncomplicated pregnancy?
|
No
|
|
|
What percentage of chronically-transfused sickle cell patients will become alloimmunized? What antigens are involved?
|
About 30%. E, C and Kell are usually involved.
|
|
|
How is the fluid management different in patients with acute chest syndrome vs. routine pain crisis?
|
In ACS, fluid (oral + IV) should not exceed 1-1.5x maintenance.
|
|
|
What is the term for rupture of collateral vessels in the CNS of sickle cell patients?
|
moyamoya. ("Puff of smoke" in Japanese)
|
|
|
What is the target Hgb S percentage in the acute treatment of sickle cell-related CVA? How long is this maintained?
|
<20-30% Hgb S acutely, then <30%. Some physicians may liberalize to <50% after 5 years or so.
|
|
|
Is hydroxyurea equivalent to chronic transfusion in prevention of recurrent stroke in sickle cell patients?
|
No. The SWiTCH trial was stopped early as patients did better with transfusions and iron chelation.
|
|
|
What is the incidence of spontaneous abortion in sickle cell patients?
|
5%.
|
|
|
What is the phenotype of heterozygous Hgb E? Homozygous?
|
Heterozygoes have no anemia, mild microcytosis and about 30% Hgb E.
Homozygotes have mild anemia, more pronounced microcytosis (65-69) and substantial numbers of target cells. |
|
|
What is the phenotype for patients with Hgb CC or Hgb C-beta thal?
|
Mild, chronic hemolytic anemia and splenomegaly.
|
|
|
Hgbs E, A2, O and C co-migrate on cellulose acetate elelctrophoresis. How are they distinguished?
|
Acid agar gel electrophoresis, isolectric focusing gel electrophoresis, of HPLC.
|
|
|
When should an unstable hemoglobinopathy be suspected?
|
In a patient with heriditary nonsherocytic hemolytic anemia, bite cells, possible basophilic stippling. Crystal violet is used to stain Heinz bodies (denatured hgb) and the isopropanol stability or heat stability test will be abnormal.
|
|
|
What test is ordered to evaluate of oxygen affinity mutants?
|
In patients with heriditary erythrocytosis or asymptomatic anemia, the P50 (partial pressure of oxygen at which the Hgb is 50% saturated) is checked. There is no treatment indicated.
|
|
|
What are the important distinctions between methemoglobinemia and sulfhemoglobinemia?
|
Sulfhemoglobinemia is not reversible but is rarely symptomatic and can be treated by withdrawing the offending agent.
|
|
|
What is Hemoglobin H?
|
an inherited form of alpha thalassemia related to the ATRX gene. It can also be associated with MDS.
|
|
|
What is the difference between hereditary spherocytosis (HS) and hereditary elliptocytosis (HE) in terms of protein-lipid interactions?
|
HS is generally based on abnormal vertical interactions; HE is generally based on horizontal interactions.
|
|
|
What type of presentation should prompt suspicion of hereditary spherocytosis?
|
Intermittent jaundice, mild refractory anemia, possibly splenomegaly.
|
|
|
Which of the RBC indices is helpful in diagnosing hereditary spherocytosis?
|
MCHC will be elevated due to cellular dehydration.
|
|
|
What is the definitive treatment for hereditary spherocytosis?
|
Splenectomy.
|
|
|
Is pigmented gallstones an indication for splenectomy in patients with hereditary spherocytosis?
|
Yes.
|
|
|
What is the phenotype for patients with hereditary elliptocytosis?
|
Most are asymptomatic.
|
|
|
What genetic disorder is associated with spur cells?
|
Abetalipoproteinemia.
|
|
|
In what conditions are stomatocytes found on peripheral smear?
|
Hepatobiliary disease, acute alcoholism, Rh null/deficiency mostly. Can also be inherited or associated with malignancy or heart disease.
|
|
|
What should be done if a patient with suspected G6PD deficiency has a normal screening test?
|
Repeat it in a few months, as a a brisk reticulocytosis can throw off the result. Also, consider other less common enzyme deficiencies.
|
|
|
What is the characteristic abnormality of RBCs on peripheral smear in PK deficiency?
|
Echinocytes (burr cells)
|
|
|
Which causes direct agglutination of RBC's, cold or warm autoantibodies?
|
Cold, due to the larger size of IgM
|
|
|
Cold agglutinins are associated with what infections? What type of malignancy?
|
Mycoplasma, EBV. In the elderly, cold agglutinins are commonly associated with B-cell lymphoproliferative disorders.
|
|
|
What type of autoantibodies are seen in paroxysmal cold hemoglobinuria?
|
Cold-reacting IgG
|
|
|
What should be done if a patient with suspected G6PD deficiency has a normal screening test?
|
Repeat it in a few months, as a a brisk reticulocytosis can throw off the result. Also, consider other less common enzyme deficiencies.
|
|
|
What is the characteristic abnormality of RBCs on peripheral smear in PK deficiency?
|
Echinocytes (burr cells)
|
|
|
Which causes direct agglutination of RBC's, cold or warm autoantibodies?
|
Cold, due to the larger size of IgM
|
|
|
Cold agglutinins are associated with what infections? What type of malignancy?
|
Mycoplasma, EBV. In the elderly, cold agglutinins are commonly associated with B-cell lymphoproliferative disorders.
|
|
|
What type of autoantibodies are seen in paroxysmal cold hemoglobinuria?
|
Cold-reacting IgG
|
|
|
In hapten/drug adsorption - mediated autoimmune hemolysis, what is the latency and time to resolution usually?
|
Begins 7-10 days after taking the drug and resolves a few days to 2 weeks after cessation.
|
|
|
What is the treatment for IgG mediated warm antibody hemolysis?
|
Prednisone 1/mg/kg/d until remission, decreased by 10 mg/week until 30 mg, then tapered more slowly. Weaning completely is possible if the DAT becomes negative. 2/3 will respond, 20% with complete remission.
|
|
|
When should splenectomy be considered in warm-agglutinin AHA?
|
If steroids fail, up to 2/3 will have a complete remission, but relapses are common.
|
|
|
What is the role of Rituxan in treating warm-agglutinin AHA?
|
Useful if steroids and/or splenectomy fails. 40-100% response rate.
|
|
|
How is the treatment of cold-agglutinin AHA different than warm agglutinin?
|
Steroids and splenectomy don't work. Keeping the patient warm may be all that is required. Rituxan may have up to 50% response rate. Plasmapheresis has been used.
|
|
|
What is the mechanism of the clinical findings of erectile dysfunction, esophageal spasm, renal insuffieciency and (to some degree) thrombosis in PNH?
|
free plasma hgb scavenges nitric oxide
|
|
|
PMH clones are also found in what other diseases?
|
About 20% of both aplastic anemia and MDS cases
|
|
|
What is the first line treatment in PNH? Second line?
|
Steroids may work (given QOD). Eculizumab is the second line and must be continued indefinitely. The drug treats hemolysis and thrombophilia, but not marrow failure.
Immunosuppression with cyclosporine or ATG also has a role. |
|
|
What is the most serious side effect of the PNH drug eculizumab?
|
Neisseria infections. Patients should be vaccinated two week before starting treatment and every 3-5 years thereafter.
|
|
|
What is the role of HSCT in PNH?
|
Allogeneic HSCT can be curative in patients who do not have an adequate response to eculizumab
|
|
|
Which chemotherapy agents have been associated with microangiopathic hemolytic anemia?
|
Mitomycin, gemcitabine. Also cyclosporine and tacrolimus, as well as clopidigrel
|
|
|
Ribavarin for treatment of hepatitis C has been associated with what hematologic side effect? How is this managed?
|
Hemolysis. Decreasing the dose or adding EPO are treatment options.
|
|
|
What is the treatment for Wilson disease?
|
Penicillamine, which mobilizes copper stores. Acute hemolysis can be treated with plasmapheresis.
|
|
|
What type of anemia can be associated with Strep, Staph, and enterococcus infections/sepsis?
|
Hemolytic anemia. Clostridium and typhoid can do the same.
|
|
|
What are the characteristics of hemolytic anemia associated with Mycoplasma pneumonia?
|
Cold agglutinins against the RBC I antigen. Rapid hemolysis, usually after respiratory symptoms resolve. Self-limited and usually mild.
|
|
|
Identification of which type of malarial parasite is most important due to the potential severity of illness?.
|
Plasmodium falciparum. Usually 2 or more parasites per RBC and >5% of RBCs infected is characteristic.
|

