![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
54 Cards in this Set
- Front
- Back
|
alpha 2, gamma 2 - is associated with which hemoglobin type
|
HGB F
which occurs in 60 - 90% of newborn hint: gamma baby |
|
|
alpha 2, delta 2 - is associated with which hemoglobin type
|
HGB A2
hint: A2D2 |
|
|
alpha 2, beta 2 - is associated with which hemoglobin type
|
HGB A
which occurs in 10 - 40% of newborn hint: alpha beta ADULTS |
|
|
what is important about Methemoglobin
|
Fe 2+ OX to Fe 3+ = brown and cannot bind O2
Fe 2+ ferrous Fe 3+ ferric |
|
|
what is important about Carboxyhemoglobin
|
increase in carbon monoxide poisoning & smokers = cherry red
|
|
|
what two components is needed for conversion of HGB to cyanmethemoglobin
|
potassium cyanide & potassium ferricyanide
|
|
|
what does anticoagulant heparin do to blood
|
it is an antithrombin agent that prevents formation of clots & naturally occurring anticoag is produced by baso + mast cells
|
|
|
what is EDTA
|
ethy-lene-diamine-tetra-actate - which chelates Ca++ so its unavailable to participate in the coag cascade
|
|
|
which cells does the following functions - O2 transport to tissue & CO2 removal from tissues, cell nutrition
|
RBC
|
|
|
which 2 cells does the following functions - phagocytic response to bacteria
|
neutrophil & monocyte
|
|
|
which cells does the following functions - humoral & cell mediated immunity
|
lymphocyte
|
|
|
which cells does the following functions - inflammatory response mediator
|
basophils
|
|
|
which cells does the following functions - allergic response regulator
|
eosinphil
|
|
|
which cells does the following functions - clotting
|
platelets
|
|
|
which cell is increased in bacterial infections
|
neutrophils (50-70%)
|
|
|
which cell is increased in viral infections
|
lymphocytes (20-40%)
|
|
|
which cell is increased in TB, syphilis, malignancies
|
monocytes (3-10%)
|
|
|
which cell is increased in allergies, PA, CML
|
eosinphil (0-3%)
|
|
|
which cell is increased in immediate hypersensitivity, CML
|
basophil (0-2%)
|
|
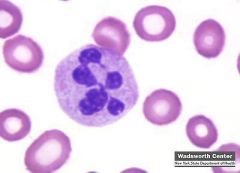
hypersegmented neutrophils is associated with
|
pernicious anemia
|
|
|
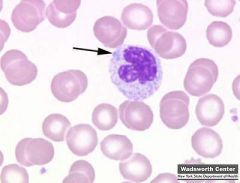
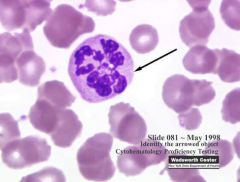
hyposegmented neutrophils is associated with (4)
|
Pelger Huet Anomaly
Pseudo-Pelger Huet Anomaly AML AIDS Pelger-Huet anomaly has an autosomal dominant pattern of inheritance. Is a benign dominantly inherited defect of terminal neutrophil differentiation secondary to mutations in the lamin B receptor (LBR) gene. Acquired or Pseudo-Pelger-Huet anomaly Develops in the course of acute or chronic myelogenous leukemia and in myelodysplastic syndromes. In patients with these conditions, the pseudo–Pelger-Huët cells tend to appear late in the disease and often appear after considerable chemotherapy has been administered. |
|

toxic granulation & vacuoles is associated with (3)
|
Burns
Bacterial infections Chemotheraphy |
|
dohle bodies (rna) is associated with (3)
|
Bacterial infections
Burns May Hegglin Döhle bodies appear as a small, light blue-gray staining area in the cytoplasm of the neutrophil. They are found in poisoning, burns, infections, and following chemotherapy. |
|
|
atypical lymphs (increase size + basophilia) is associated with
|
Infectious mono
& other viral infections |
|
|
rouleaux is found in what 2 conditions
|
Mx myeloma & Macroglobulinemia
|
|
|
what disease is related to the key lab findings for:
decrease Fe decrease % Saturation INCREASE TIBC |
iron defncy
Low % saturation as there is insufficient iron. High Transferrin/TIBC. The liver produces more transferrin, presumably attempting to maximize use of the little iron that is available. |
|
|
what disease is related to the key lab findings for:
decrease Fe decrease TIBC |
chronic disease/inflammation
Low TIBC. The body produces less transferrin (but more ferritin), presumably to keep iron away from pathogens that require it for their metabolism. Total iron-binding capacity (TIBC) is a medical laboratory test which measures the blood's capacity to bind iron with transferrin measuring the maximum amount of iron that it can carry, which indirectly measures transferrin since transferrin is the most dynamic carrier |
|
|
what disease is related to the key lab findings for:
basophillic stippling increase blood lead level increase FEP |
lead poisoning
|
|
|
what are the key lab findings for:
normal Fe normal TIBC increase A2 increase F |
thalassemia trait
|
|
|
what disease is related to the key lab findings for:
decrease B12 decrease Retics pancytopenia oval macrocytes hypersegmented polys howell jolly (HJ) bodies |
B12 defncy
b12: coemz for conversion methylmalonyl CoA to Succinyl |
|
|
what disease is related to the key lab findings for:
Anti IF + (intrinsic factor) increase MMA (methylmalonic acid) increase homocysteine Normal Schilling Test with IF |
pernicious anemia
|
|
|
what disease is related to the key lab findings for:
Anti IF - (negative) Abnormal Schilling test with and WITHOUT IF |
malabsorption
|
|
|
what disease is related to the key lab findings for:
round macrocytes target cells increase in liver emz |
liver disease/alcoholism
|
|
name 7 lab key findings that is associated with Folate defncy
|
decrease serum/erythrocyte folate levels
decrease retics increase homocysteine Anti IF - (negative) oval macrocytes hypersegmented polys 2.5-20 ng/ml |
|
|
which antibody mediated disease is associated with the following lab key findings
increase Bili decrease Haptoglobin DAT + Donath Landsteiner Ab |
PCH - a polyclonal IgG anti-P autoantibody binds to red blood cell surface antigens in the cold
Paroxysmal cold hemoglobinuria (PCH) (also known as Donath-Landsteiner syndrome) is a disease of humans that is characterized by the sudden presence of hemoglobin in the urine (called hemoglobinuria), typically after exposure to cold temperatures. |
|
|
which antibody mediated disease is associated with the following lab key findings
increase Bili decrease Haptoglobin DAT + IgM Ab Cold Agglutinin Titer + |
Cold agglutinin disease
|
|
|
which antibody mediated disease/anemia is associated with the following lab key findings
increase Bili decrease Haptoglobin DAT + IgG Ab |
Warm autoimmune hemolytic anemia
|
|
|
which membrane defect disease is associated with the following lab key findings
increase Osmo frag increase MCHC Spherocytes |
Hereditary spherocytosis
|
|
|
which antibody mediated disease is associated with the following lab key findings
elliptocytes (>15% to 100%) |
hereditary elliptocytosis
|
|
|
which antibody mediated disease is associated with the following lab key findings
CD 55 - (neg) CD 59 - (neg) Hams test + Sucrose hemolysis + |
PNH
sometimes referred to as Marchiafava-Micheli syndrome, is a rare, acquired, potentially life-threatening disease of the blood characterised by complement-induced hemolytic anemia (anemia due to destruction of red blood cells in the bloodstream), red urine (due to the appearance of hemoglobin in the urine) and thrombosis. PNH is the only hemolytic anemia caused by an acquired (rather than inherited) intrinsic defect in the cell membrane |
|
|
which enzyme defncy is associated with the following lab key findings
heniz bodies decrease G6PD |
G6PD
|
|
|
which enzyme defncy is associated with the following lab key findings
NO heinz bodies decrease PK |
Pyruvate kinase
|
|
|
which anemia is associated with the following lab key findings
"dry tap" bone marrow hypocellular BM decrease retics pancytopenia |
Aplastic anemia
|
|
|
which anemia is associated with the following lab key findings
normal BM increase retics |
acute blood loss
|
|
|
what are some key lab findings for Hemoglobin defects (2)
|
Definitive Poikylocytes on smear (HbC crystals, sickle cells, SC crystals)
HB Electrophoresis |
|
|
name the following classification of anemia with problem with heme (3)
|
Fe defncy
Sideroblastic Chronic dz/inflamtx |
|
|
name the following classification of anemia with problem with globin (2)
|
Thalassemia
Hemoglobin E |
|
|
name the following classification of anemia with antibody destruction (3)
|
HDN
Transfusion rtx Autoimmune hemolytic anemia |
|
|
name the following classification of anemia with RBC membrane defect (3)
|
HS/HE
Paroxysomal nocturnal hemoglobinuria (PNH) |
|
|
name the following classification of anemia with emz defncy (2)
|
G6PD
Pyruvate kinase (PK) |
|
|
name the following classification of anemia with decrease production/loss (2)
|
aplastic anemia
acute blood loss |
|
|
name the following classification of anemia with hemoglobinopathies (2)
|
Hb S
Hb C |
|
|
name the following classification of anemia with megaloblastic maturation (2)
|
B12 defncy
Folate defncy |
|
|
name the following classification of anemia with non-megaloblastic maturation
|
liver disease
|

