![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
231 Cards in this Set
- Front
- Back
|
What is the best treatment for patients with acute venous thromboembolism and metastatic cancer?
|
Chronic low-molecular-weight heparin at therapeutic doses
|
|
|
Which patients should have an IVC filter?
|
high risk for recurrent thrombosis who have sustained major bleeding and cannot undergo anticoagulation
|
|
|
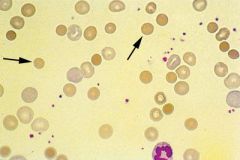
What changes can be seen on peripheral blood smear with iron-deficiency anemia?
|
microcytic, hypochromic red cells; abnormalities in erythrocyte size (anisocytosis) and shape (poikilocytosis); and, occasionally, red blood cells of bizarre shapes, such as cigar-shaped cells. (increases reported red cell distribution width)
|
|
|
How is TTP treated?
|
plasmapheresis
|
|
|
How do you treat warm antibody-mediated autoimmune hemolytic anemia?
|
corticosteroids
|
|
|
How does antibody-mediated autoimmune hemolytic anemia manifest itself on blood smear?
|
spherocytes on the peripheral blood smear
|
|
|
What will you see on a blood smear of a patient with microangiopathic hemolytic anemia?
|
nucleated red blood cells and low platelet counts
|
|
|
What is the primary manifestation of transfusion-related acute lung injury?
|
hypoxemia
|
|
|
What causes transfusion-related acute lung injury?
|
Antileukocyte antibodies in donor plasma react with antigens on the surface of patients' leukocytes, chiefly neutrophils, leading to neutrophil aggregation and leukostasis in the pulmonary vasculature
|
|
|
How is TRALI treated?
|
supportively, avoid diuretics
|
|
|
What are the major diagnostic criteria of polycythemia vera?
|
- Elevated red blood cell mass
- Normal blood oxygen saturation - Presence of splenomegaly. |
|
|
How do you treat polycythemia vera?
|
phlebotomy & low-dose aspirin
|
|
|
What causes the iron deficiency with PCV?
|
reflects the increased use of endogenous iron stores as a consequence of increased bone marrow erythroid activity rather than iron deficiency caused by blood loss or decreased dietary iron consumption
|
|
|
When should hydroxyurea be used in PCV patients?
|
When patient's platelet count were increased to >600,000/μL
|
|
|
What is the hematocrit goal for patients being phlebotomized for PCV?
|
< 45%
|
|
|
How would sickle cell trait appear on Hb electrophoresis?
|
Dark A (fast) band and Dark S band
|
|
|
How would hemoglobin SC appear on Hb electrophoresis?
|
Dark A2 (slow) band and Dark S band
|
|
|
How would hemoglobinS/B+ thalassemia on Hb electrophoresis?
|
Dark S band and faint A and A2 bands
|
|
|
What characterizes MGUS?
|
- Presence of serum monoclonal gammaglobulin without the clinical features of multiple myeloma
- paraprotein level <3.5 g/dL (35 g/L), and - less than 10% plasmacytosis in the bone marrow |
|
|
How should MGUS be managed?
|
routine follow-up to identify signs of progression to multiple myeloma and periodic measurement of serum monoclonal protein concentration
|
|
|
What can be done to minimize the need for donor blood transfusion during surgery?
|
Intraoperative acute normovolemic hemodilution
|
|
|
What is the treatment for multiple myeloma?
|
thalidomide and dexamethasone
|
|
|
What is a common side effect of bortezomib therapy for multiple myeloma?
|
peripheral neuropathy (~30% of patients). Typically sensory. but can be mixed motor & sensory.
|
|
|
80 yr patient with DM and multiple myeloma treated with bortezomib presents with stocking-glove neuropathy. What is the cause?
|
Drug toxicity from bortezomib
|
|
|
What is seen clinically with POEMS syndrome?
|
- Polyneuropathy,
- Organomegaly - Endocrine abnormalities - Monoclonal gammopathy - Skin findings |
|
|
What is POEMS syndrome?
|
rare plasma cell dyscrasia
|
|
|
How should patients with HIT be managed?
|
stopped and alternative anticoagulation with a direct thrombin inhibitor (argatroban or lepirudin) instituted immediately
|
|
|
Which direct thrombin inhibitor should be used in patients with HIT and thrombosis?
|
lepirudin
|
|
|
Young female with antithrombin heterozygosity or Factor V leiden presents requesting OCP. What should be prescribed?
|
She should be prescribed oral progestin-only–containing contraceptives
|
|
|
How should delayed hemolytic transfusion reaction be treated?
|
avoidance of the incompatible antigen. No role for steroids in alloimmunity.
|
|
|
What are signs suggestive of disease transformation from myelodysplastic syndrome to acute myeloid leukemia (AML)?
|
severe pancytopenia and circulating myeloid blasts on peripheral blood smear
|
|
|
What is the induction chemotherapy for AML?
|
cytarabine and anthracycline
|
|
|
If suspecting conversion of myelodysplastic syndrome to AML, what diagnostic test should be performed?
|
Bone marrow aspirate and biopsy (confirms diagnosis and gives cytogenic info)
|
|
|
Which has better response to chemo, transformed AML or de novo AML?
|
transformed AML
|
|
|
What do patients with α-thalassemia trait have on blood smear?
|
- Mild microcytic anemia with
- Pominent target cells |
|
|
What type of defect do patients with alpha-thalassemia trait have? What chromosome is it on?
|
2 gene defect (a,--)/(a, --)
Chromosome 16 |
|
|
Are RBC counts elevated, reduced or normal in pateints with thalassemia?
|
preserved or increased
|
|
|
Are RBC counts elevated, reduced or normal in pateints with tiron deficiency anemia?
|
reduced
|
|
|
Do asymptomatic, pregnant sickle cell patients require transfusions?
|
No, not unless she has cardiovascular difficulties or low retic count
|
|
|
When can patients with delayed-onset heparin-induced thrombocytopenia (HIT) present?
|
3-4 wks after heparin exposure
|
|
|
How is acute chest syndrome (ACS) characterized in sickle patients?
|
- fever
- chest pain, - shortness of breath - hypoxia, and a - radiographically detected chest infiltrate |
|
|
How should acute chest syndrome be treated?
|
erythrocyte transfusion (simple or exhange) to achieve a target hemoglobin of 10 g/dL (100 g/L).
|
|
|
How should transfusion-dependent myelodysplastic disorder be treated?
|
Erythropoietin therapy
|
|
|
What is Imatinib mesylate used for?
|
bcr-abl chromosomal translocation typically found in chronic myeloid leukemia and in some cases of acute lymphoblastic leukemia
|
|
|
Describe the iron stores of patients with myelodysplastic syndrome
|
adequate or elevated
|
|
|
Patient admitted with infection treated with cephalosporine and receives blood transfusion. He later becomes anemic with weakly positive DAT. How do you differentiate drug-induced from warm autoantibody reaction?
|
Patients with a drug-induced antibody reaction do not have indications of hemolysis or evidence of complement activation on direct antibody testing
|
|
|
Cold reactive autoantibodies are IgM antibodies or IgG antibodies?
|
IgM antibodies
|
|
|
What do you see with cold autoantibody reaction?
|
Positive DAT positive for complement but not IgG
|
|
|
Which mutations are the most common mutations predisposing to venous thrombosis in white populations?
|
Factor V Leiden and prothrombin G20210A
|
|
|
Which factor is low in pregnancy and can make testing for thrombophilic disorder difficult?
|
Protein S
|
|
|
If a patient has slight anemia, thrombocytopenia and not responding to prednisone. What should be done next?
|
Bone marrow aspiration and biopsy
|
|
|
How would you describe the bone marrow of AML?
|
hypercellular
|
|
|
What can be used to decrease the need for transfusions in aplastic anemia?
|
antithymocyte globulin and cyclosporine
|
|
|
What treatment can be curative for aplastic anemia?
|
Allogeneic stem cell transplantation (consider age and if has living siblings)
|
|
|
What characterizes inflammatory anemia (anemia of chronic disease)?
|
- low or normal serum iron concentration
- reduced serum total iron-binding capacity, - serum ferritin that is not decreased |
|
|
What is diagnostic of multiple myeloma?
|
- Hypercalcemia,
- Bone pain - Anemia - Clusters of large plasma cells on bone marrow aspirate smear |
|
|
What do you think of when you hear perinuclear halo?
|
multiple myeloma
|
|
|
Which leukemia is associated with Philadelphia chromosome (Ph)-positive?
|
CML
|
|
|
What leads to suppression of CML?
|
Imatinib mesylate
|
|
|
What is thrombotic thrombocytopenia purpura (TTP) is characterized by?
|
-Fever
- Neurologic abnormalities - Thrombocytopenia - Microangiopathic hemolytic anemia - Renal insufficiency |
|
|
What do you see with microangiopathic hemolytic anemia?
|
- anemia
- schistocytes - elevated serum lactate dehydrogenase concentration |
|
|
What is the treatment for TTP?
|
emergent plasma exchange, followed by plasma infusion
|
|
|
Patient with warm autoimmune hemolytic anemia on corticosteroid treatment develops heart failure and full blood serologic evaluation not yet complete. How should the patient be treated?
|
immediate transfusion, even when only incompatible blood (hemolysis may worsen)
|
|
|
When is splenectomy indicated for corticosteroid warm autoimmune hemolytic anemia?
|
when refractory to corticosteroid treatment
|
|
|
What are the causes of Autoimmune hemolytic anemia (AIHA)?
|
- Idiopathic
- Drugs - Lymphoproliferative disorders - Collagen vascular diseases, - malignancies |
|
|
What do you see on peripheral smear with autoimmune hemolytic anemia?
|
polychromatic red blood cells and spherocytes
|
|
|
Patient presents short of breath, anemic, elevated reticulocytes, spherocytes. What is the diagnosis?
|
Autoimmune hemolytic anemia
|
|
|
How should patients with corticosteroid-refractory autoimmune hemolytic anemia?
|
splenectomy, raises hemoglobin in 2/3 of people
|
|
|
When does thrombocytopenia in pregnancy need to be evaluated?
|
when platelet values decrease to lower than 70,000/μL
|
|
|
What should be done with incidental thrombocytopenia found during prenancy?
|
careful follow-up
|
|
|
What are the characteristics of the HELLP syndrome?
|
- Hemolysis with a microangiopathic blood smear
- Elevated liver enzymes - Low platelet count |
|
|
What is the most likely diagnosis for a patient with sepsis, severe neutropenia, and relatively well-preserved hematocrit and platelet counts after ingestion of trimethoprim–sulfamethoxazole?
|
Drug-induced agranulocytosis
|
|
|
How can you treat drug-induced agranulocytosis if the patient is septic?
|
granulocyte colony-stimulating factor - can shorten her recovery period and may be helpful in the treatment of her severe infection
|
|
|
Patient presents with history of mucosal bleeding (as do other family members) and mildly prolonged activated partial thromboplastin time. What is this consistent with?
|
von Willebrand's disease
|
|
|
When you do typically see bleeding in patients with essential thrombocytosis?
|
with really high platelet counts
|
|
|
Where does bleeding usually occur with hemophilia A? What is the laboratory abnormality?
|
- Bleeding into joints
- markedly prolonged aPTT |
|
|
What can improve the response to erythropoietin in patients receiving dialysis?
|
Vitamin C (mobilizes iron stores for erythropoeisis)
|
|
|
What can erythropoietin failure in patients receiving dialysis?
|
- Iron deficiency
- Folate deficiency - Ongoing blood loss - Iron overload |
|
|
54 yo female with lower extremity edema, proteinuria, and monoclonal gammopathy in serum or urine. What should be suspected?
|
amyloidoisis (AL)
|
|
|
How can amyloidoisis AL be diagnosed?
|
kidney biopsy
|
|
|
What causes bleeding symptoms and hematologic abnormalities in patients with autoimmune disorders, malignancy, or in the postpartum setting?
|
acquired factor VIII inhibitor
|
|
|
What can be tested to confirm acquired factor VIII inhibitor?
|
inhibitor screen and factor VIII level
|
|
|
What malignancy is associated with acquired Factor VIII inhibitor?
|
lymphoma
|
|
|
What is characteristically seen with hereditary spherocytosis?
|
- hemolytic anemia
- Coomb's negative - elevated mean hemoglobin concentration - predominantly spherocytes on peripheral smear |
|
|
What conditions should you think of when you see spherocytic red blood cells on peripheral smear?
|
- Hereditary spherocytosis
- Warm-antibody hemolytic anemia |
|
|
Is a new alloantibody is not always detectable in patients with sickle cell disease who have adverse transfusion reactions?
|
NO
|
|
|
What condition should you think of if you see teardrop erythrocytes on peripheral smear?
|
myelofibrosis
|
|
|
What is the clinical presentation for patients with myelofibrosis?
|
- Fatigue
- Weight loss - Massive splenomegaly - Teardrop-shaped erythrocytes on peripheral blood |
|
|
How do you treat myelofibrosis?
|
chronic blood transfusion
|
|
|
When is treatment for ITP generally initiated?
|
when platelets drop < 30.000
|
|
|
Is bone marrow examination required in the diagnosis of ITP?
|
NO
|
|
|
What is the likely diagnosis of isolated thrombocytopenia in an otherwise-healthy young patient?
|
ITP
|
|
|
What treatment provides disease-free and overall survival advantage for patients with multiple myeloma?
|
high-dose chemotherapy and autologous stem cell transplantation
|
|
|
Which treatment should be avoided in multiple myeloma patients that are candidates for autologous stem cell transplantation?
|
Melphalan
|
|
|
What is a side effect of melphalan?
|
cumulative myelotoxicity
|
|
|
What are some of the adverse events with Thalidomide?
|
- major fetal malformations
- increase the risk of thromboembolism - cause somnolence - debilitating neuropathy. |
|
|
What treatment can be used for relapsed and refractory myeloma?
|
Bortezomib
|
|
|
What are potential adverse effects of long-term parenteral bisphosphonate therapy?
|
Renal dysfunction and osteonecrosis of the jaw
|
|
|
What additional treatment should be started in patients with multiple myeloma?
|
Monthly parenteral bisphosphonate therapy
|
|
|
What is the appropriate treatment for a patient with HELLP?
|
delivery of the fetus
|
|
|
What can be given to hasten fetal lung maturity?
|
betamethasone
|
|
|
In whom should inherited thrombocytopenic disorder be suspected?
|
otherwise-healthy patients with
- low platelet count - giant platelets on peripheral blood smear - family history of thrombocytopenia, and -who are refractory to corticosteroids |
|
|
What laboratory study abnormalities are seen in patients with B12 deficiency?
|
- elevated serum lactate dehydrogenase
-elevated unconjugated bilirubin -elevated serum methylmalonic acid -homocysteine concentrations -may have increased forgetfulness |
|
|
What laboratory differences are seen with B12 and folate deficiencies?
|
folate deficiency only has elevated homocysteine concentration
|
|
|
In patients without hemorrhagic risk factors, at what platelet level should phrophylactic transfusions of platelets begin?
|
< 10,000
|
|
|
What platelet level should be maintained for patients with pulmonary hemorrhage and those undergoing most types of major surgery?
|
40,000-50,000
|
|
|
What are symptoms of symptoms of serotonin syndrome?
|
- Tachycardia
- Hypertension - Hyperthermia - Mydriasis - Hyperactive bowel sounds, - Diaphoresis - Hyperreflexia - Clonus - Changes in mental status. |
|
|
What do you see with neuroleptic malignant syndrome?
|
- Slow-onset bradykinesia
- Muscular rigidity - Hyperthermia - Fluctuating consciousness - Autonomic instability |
|
|
What is a major difference between symptom onset of neuroleptic malignant syndrome and serotonin syndrome?
|
NMS symptoms evolve over days and within hours for serotonin syndrome
|
|
|
What treatment can be used for patients with thalassemia with iron overload?
|
Deferoxamine - parenteral iron chelator
|
|
|
If a pateint is pregnant and needs a blood transfusion, but her CMV status is unknown what kind of special blood product requirement is needed?
|
Leukoreduction
|
|
|
What will CMV transmission to a pregnanct female do to the fetus?
|
- Teratogenicity
- Mental retardation or the so-called TORCH syndrome (toxoplasmosis, other [syphilis], rubella, cytomegalovirus, and herpes simplex virus). |
|
|
What does leukocyte reduction do?
|
decreases primary HLA alloimmunization and many nonhemolytic, febrile transfusion reactions, but it also prevents CMV transmission because the donor blood lacks free viremia and contains leukocytes with a reservoir of latent virus
|
|
|
What is Sweets syndrome?
|
neutrophilic dermatosis associated with blood neutrophilia and occurs in the setting of acute myeloid leukemia and other myeloid disorders, and during treatment with trans-retinoic acid and granulocyte colony-stimulating factor
|
|
|
How are all stages of Hodgkins lymphoma treated?
|
systemic chemotherapy with curative intent
|
|
|
What malignancy is associated with Reed-Steinberg cell?
|
Hodgkin's lymphoma
(CD20−, CD15+, and CD30+ expression) |
|
|
What are the distinctive qaulities of Hodgkin lymphoma?
|
- the malignant Reed-Steinberg cell (CD20−, CD15+, and CD30+ expression)
- Disease spread is commonly contiguous, usually emanating from a cervical lymph node; - More than 75% of patients with newly diagnosed disease can be cured with combination chemotherapy, with or without radiotherapy |
|
|
How is Hodgkin's lymphoma staged?
|
- blood tests (including erythrocyte sedimentation rate)
- CT scans of the chest, abdomen, and pelvis - Occasionally, bone marrow biopsy or aspirate. |
|
|
What does ABVD therapy consist of for Hodgkin's lymphoma?
|
- Doxorubicin
- Bleomycin - Vinblastine - dacarbazine |
|
|
How should patients with Hodkins lymphoma be treated if have early-stage disease and a favorable prognosis?
|
- Four cycles of ABVD alone or
- Two cycles of ABVD plus involved-field radiation therapy at 20 Gy |
|
|
How should patients with Hodkins lymphoma be treated if have early-stage disease and a unfavorable prognosis?
|
Four cycles of ABVD plus involved-field radiation therapy at 20 Gy
|
|
|
How should patients with Hodkins lymphoma be treated if have advanced-stage disease and a favorable prognosis?
|
six cycles of ABVD
|
|
|
What are late complications for patients with Hodgkin's lymphoma?
|
- solid tumors (15-25 yrs later due to radiation)
- AML or myelodysplastic syndrome (if received akylating agents - mechlorethamine or procarbazine OR topoisomerase II inhibitors such as etoposide) - MI (>5 yrs) |
|
|
What are potential adverse events associated with akylating treatment (mechlorethamine or procarbazine) for Hodkin's lymphoma?
|
- Azospermia (males)
- amenorrhea (women > 30) |
|
|
What are the chemo regimens for colon cancer?
|
- 5-flourauracil plus leucovorin (FU/LV standard)
- oxaliplatin plus FU/LV (FOLFOX) : Stage III cancer |
|
|
What is a side effect of leuprolide (Gonadotropin-releasing hormone agonists)?
|
bone loss & osteoprosis
(reduced levels of testosterone result in less conversion of testosterone to estradiol, which is needed to protect and strengthen bones) |
|
|
What is the management of patients with localized prostate cancer?
|
- radical prostatectomy
- External-beam radiotherapy - Ccryotherapy, or - Watchful waiting |
|
|
What are useful prognostic factors for prostate cancer?
|
- Serum PSA concentration
- Clinical stage - Gleason score - Number of positive biopsy specimens at diagnosis |
|
|
How are patients with with metastatic prostate cancer usually treated?
|
- Bilateral orchiectomy or Gonadotropin-releasing hormone agonists (GnRH-As) with or without antiandrogen therapy
|
|
|
What types of symptoms do GnRH-agonists cause?
|
- Hot flushes
- Gynecomastia - loss of libido - impotence - tumor flare |
|
|
Descrube tumor flare reactions and how they can be prevented?
|
- treatment with GNRH agonists causes an increase in FSH & LH leading to an increase in testosterone & worsening of prostate ca symptoms.
- use of antiandrogen therapy can reduce reaction |
|
|
What are some anitandrogen agents?
|
- bicalutamide
- nilutamide - flutamide |
|
|
What treatment should be considered in patients receiving long-term androgen-deprivation therapy?
|
Calcium with vitamin D supplementation
|
|
|
Which drug should be avoided in patients who smoke or have an elevated risk of lung cancer?
|
beta-carotene
|
|
|
What should be monitored after orchiectomy for testicular cancer?
|
serial measurements of AFP & B-hCG levels
|
|
|
What is the half-lives of AFP & b-hCG?
|
AFP: 5-7 days
B-hCG: 24 hrs |
|
|
How can you detect recurrent or persistent tumor with testicular cancer?
|
- reappearance of tumor markers or
- the failure of tumor marker concentrations to decline |
|
|
How are Stage I disease or nonbulky (tumor size <5 cm) stage II seminomas treated?
|
orchiectomy followed by retroperitoneal radiation therapy
|
|
|
How are bulky stage II seminoma generally managed?
|
cisplatin-based combination chemotherapy after orchiectomy
|
|
|
How is Stage II nonseminoma managed?
|
orchiectomy and retroperitoneal lymph node dissection, with or without two courses of cisplatin-based chemotherapy
|
|
|
How are Stage II nonseminomas with large retroperitoneal lymph nodes treated?
|
three courses of chemotherapy after orchiectomy and not retroperitoneal lymph node dissection
|
|
|
Is Stage 1 nonseminoma highly curable?
|
Yes, >95% with surgery alone
|
|
|
What is the cornerstone of successful treatment in patients with stage III seminoma and nonseminoma?
|
Chemotherapy
|
|
|
Which testicular cancer patients are candidates for high-dose chemotherapy with autologous stem cell transplantation?
|
Patients who have an incomplete response to first-line therapy and those requiring third-line salvage therapy
|
|
|
What is curative for patients with early-stage ovarian cancer?
|
surgery alone
|
|
|
How should patients with Stage III or IV ovarian cancer be treated?
|
With six to eight cycles of platinum- or taxane-based chemotherapy
|
|
|
Which stages of ovarian cancer should be treated with surgery alone?
|
Stage IA or IB
|
|
|
When would observation for 1 month before performing biopsy be appropriate only in patients with cervical lymph nodes?
|
When the node is <2 cm
|
|
|
What must be considered in patients who have lymphoplasmacytic lymphoma (Waldenström's macroglobulinemia) with an elevated serum IgM concentration?
|
hyperviscosity syndrome
|
|
|
What should be checked in patients suspected of having hyperviscosity syndrome and evidence of heart failure?
|
serum viscosity level
|
|
|
How should patients with hyperviscosity syndrome be treated?
|
- emergent plasmaphoresis PLUS
- administration of immediate systemic treatment, such as rituximab–fludarabine or rituximab–cyclophosphamide–vincristine–prednisone combination therapy |
|
|
When should plasmaphoresis and systemic treatment be started for hyperviscosity syndrome?
|
- serum viscosity >3.0 with suspicious symptoms
OR - a value of >4.0 without suspicious symptoms |
|
|
Who should consider prophylactic oopherectomy?
|
Only women who are at high risk for ovarian cancer
|
|
|
What should females at high risk for ovarian cancer do if they want to preserve child-bearing potential?
|
undergo routine screening for the circulating serum tumor maker, CA-125, in addition to pelvic ultrasonography
|
|
|
Which serum marker is elevated in pancreatic cancer?
|
CA 19-9 (this tumor marker's role has not been proved in the diagnosis or management of pancreatic cancer)
|
|
|
How is pancreatic cancer staged?
|
- Stage I - tumor limited to the pancreas
- Stage II - tumor extending into the duodenum, bile duct, or peripancreatic tissues - Stage III - regional lymph node involvement - Stage IV disease by tumor extending directly into the stomach, spleen, colon, or adjacent large vessels, or by the presence of metastatic disease |
|
|
What is the first-line therapy of choice for patients with metastatic pancreatic cancer and good performance status?
|
gemcitabine
|
|
|
In patients at risk for tumor lysis syndrome, how can hyperuricemia be treated if unable to tolerate oral intake?
|
IV rasburicase (if can tolerate orals, use allopurinol)
|
|
|
How do you treat tumor lysis syndrome?
|
- IV hydration
- urinary alkalinization (bicarb) - Xanthine oxidase inhibitor (allopurinol) OR (rasburicase if cannot tolerate orals) |
|
|
When is re-excision indicated in patients with breast cancer?
|
In patients with positive tumor margins detected after breast-conserving surgery
|
|
|
Which breast cancer patients are better served with mastectomy than breast-conserving therapy?
|
When
- Complete excision cannot be achieved unless mastectomy is performed - Tumor cannot be accessed by radiation - Radiation is contraindicated |
|
|
What are patients with ductal carcinoma in situ at increased risk for?
|
New or locally recurrent breast cancer in the contralateral or ipsilateral breast
|
|
|
Does use of sunscreen decrease risk of melanoma?
|
NO, decreases risk of squamous cell carcinoma
|
|
|
How should patients with testicular cancer metastatic to the brain be treated?
|
whole-brain radiation therapy and combination chemotherapy
|
|
|
What can be done to facilitate sphincter-preserving surgery in patients with distal rectal tumors?
|
Treat with preoperative radiation therapy plus chemotherapy to reduce tumor size
|
|
|
What chemotherapy is used to treat colon cancer?
|
- 5-fluorouracil and leucovorin
- oxaliplatin with 5-fluorouracil and calcium leucovorin |
|
|
Which cancer has a higher rate of local recurrence, rectal or colon cancer?
|
rectal
|
|
|
What tumor location prevents low anterior resection?
|
tumors within 6 cm of the anal verge
|
|
|
How are tumors within 6 cm of the anal verge treated surgically?
|
wide surgical resection with abdominoperineal resection (removing the anus and sphincter muscle) and permanent colostomy
|
|
|
What infectious agent is associated with Gastric mucosa-associated lymphoid tissue (MALT) lymphoma?
|
Helicobacter pylori
|
|
|
How is remission of MALT lymphoma achieved?
|
With eradication of H. pylori with antibiotics and PPI therapy.
|
|
|
How is MALT lymphoma monitored?
|
repeated endoscopies every 3-4 months
|
|
|
What virus is Marginal-zone lymphoma (lymph node and splenic types) associated with?
|
Hep C
|
|
|
What other diseases do patients with MALT usually have?
|
autoimmune diseases such as Hashimoto's thyroiditis and Sjogren's syndrome
|
|
|
How is progression of MALT lymphoma treated?
|
- Radiotherapy
- Rituximab - Gastrectomy, - Chemotherapy or a combination of these modalities |
|
|
What is MALT lymphoma of the small bowel also known as?
|
- immunoproliferative small intestinal disease
- Heavy-chain disease |
|
|
Where is MALT lymphoma of the small bowel usually seen? Who gets it? and what infectious agent is it associated with?
|
- Middle east
- young adults - camplylobacter jejuni |
|
|
Do patients with small cell cell lung cancer and poor performance status respond well to chemo and whole-brain radiation?
|
YES
|
|
|
What helps reduce skeletal-related events in patients with metastatic lung cancer?
|
Bisphosphonates such as pamidronate or zolendronate
|
|
|
What suggests low risk of metastatic prostate cancer?
|
- Low gleason score
- PSA < 10 - Disease stage - # of positive biopsies |
|
|
Besides 5-fluorouracil and oxaliplatin, what other agents can be used to treat colorectal cancer?
|
irinotecan
bevacizumab cetuximab |
|
|
How should patients with histologically confirmed adenocarcinoma of the axillary lymph nodes but no clinically or radiologically detected breast abnormalities be treated?
|
As Stage II breast canver (radiation therapy of the breast and chemo therapy)
|
|
|
How should patients with advanced-stage follicular lymphoma be managed?
|
watchful waiting
|
|
|
What would indicate reasons for starting therapy for advanced-stage follicular lymphoma?
|
- fever
- soaking night sweats - weight loss (>10% baseline weight within 6 months) - leukopenia - thrombocytopenia - severe anemia that is refractory to treatment with growth factors - hydronephrosis - biliary obstruction - very bulky (>10 cm) lymphadenopathy that causes discomfort. |
|
|
what is the median survival for patients with advanced-stage follicular lymphoma?
|
10-14 years
|
|
|
How may localized follicular lympphoma (stage I) may be cured?
|
radiotherapy alone may cure patient
|
|
|
What laboratory abnormalities are seen with tumor lysis syndrome?
|
elevated potassium, phosphorus and uric acid
|
|
|
What therapy decreases breast cancer risk by approximately 50% in pre- and postmenopausal women who have an elevated risk for this disease?
|
tamoxifen
|
|
|
What are potential harms of tamoxifen therapy?
|
- hot flushes
- endometrial cancer - thromboembolic disease - ocular problems |
|
|
What type of cancer is EBV associated with?
|
non-Hodgkin's lymphoma
|
|
|
What does the Gleason score for prostate cancer represent?
|
histologic scoring system, tumors are graded from 1 to 5 based on the degree of glandular differentiation and structural architecture
|
|
|
How do you interpret the Gleason score for prostate cancer?
|
Total Gleason scores of;
- 2 to 4 represent well-differentiated tumors - 5 to 6 represent moderately differentiated tumors - 7 represents moderately poorly differentiated tumors - 8 to 10 represent poorly differentiated tumors |
|
|
Which of the 2 Gleason score is most predictive of outcome?
|
the first
|
|
|
How should mixed seminomatous germ cell tumors be managed?
|
As nonseminomatous germ cell tumors & with chemotherapy
|
|
|
What is the best way to establish a diagnosis in patients with suspicious lymphocytosis?
|
flow cytometry of peripheral blood
|
|
|
What decreases a male's risk for prostate cancer?
|
Finasteride
|
|
|
What are some side effects of finasteride?
|
- reduced volume of ejaculate
- loss of libido - gynecomastia - erectile dysfunction **lower incidence of urinary obstructive symptoms ** higher gleason scores |
|
|
How should patients with squamous cell carcinoma (SCC) of unknown primary site and upper or midcervical lymph node involvement be treated?
|
As if they had locally advanced SCC of the head and neck
|
|
|
How is locally advanced SCC of the head and neck treated?
|
- radiation therapy to the pharyngeal acid and bilteral neck
- radical neck dissection - combination of these two therapies |
|
|
What is more effective than tamoxifen against breast cancer in postmenopausal women with hormone receptor–positive breast cancer?
|
aromatase inhibitors
(anastrozole, exemestane, or letrozole) |
|
|
How should patients with marginal-zone B-cell lymphoma be treated if Hep C not detected?
|
Splenectomy
|
|
|
Young, male patients with poorly differentiated midline carcinoma containing germ cell cancer markers and isochromosome 12p. What is the likely diagnosis and how should he be treated?
|
- extragonadal germ cell cancer
- cisplatin-based chemo |
|
|
What improves survival in men with metastatic prostate cancer refractory to hormonal ablation therapy?
|
Docetaxel and prednisone
|
|
|
Should aromatase inhibitors be used in premenopausal women with hormone receptor negative breast cancer?
|
NO
|
|
|
What is used to treat metastatic HER2-positive breast cancer?
|
trastuzumab and chemotherapy
|
|
|
How should patients with early-stage resectable non–small-cell lung cancer be treated/
|
adjuvant chemotherapy
|
|
|
What is curative for most patients with diffuse large B-cell lymphoma?
|
Combination of:
- Rituximab - CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) - with or without radiation therapy |
|
|
What does bronchioloalveolar cell carcinoma respond to?
|
epidermal growth factor receptor inhibitors (Erlotinib or gefitinib)
|
|
|
What does combination hormone replacement therapy increase the risk of?
|
breast cancer
|
|
|
What does unopposed estrogen therapy increases the risk of?
|
uterine cancer
|
|
|
When does testicular cancer usually relapse?
|
within 2 years after definitive therapy
|
|
|
Where does ovarian cancer usually metastasize to?
|
Pleura and peritoneum
(rarely to bone or liver, and almost never to breast) |
|
|
Where does breast cancer usually metastasize to?
|
pleura, peritoneum, liver and bone
|
|
|
What is the tumor marker for ovarian cancer?
|
CA-125
|
|
|
What malignancies are associated with HHV8 with HIV?
|
- Primary effusion B-cell lymphoma (very rare)
- Castleman's disease (plasmablastic multi-centric) (very rare) - Kaposi's sarcoma (HIV-related) |
|
|
What malignancy is associated with HTLV?
|
Adult T-cell leukemia/lymphoma (very rare)
|
|
|
What malignanies are associated with Hep C?
|
- Lymphoplasmacytic lymphoma (Waldenström's macroglobulinemia)
- Nodal marginal zone B-cell lymphoma - Splenic marginal zone B-cell lymphoma (splenic lymphoma with villous lymphocytes) |
|
|
How is the diagnosis of chronic lymphocytic leukemia established?
|
flow cytometry
|
|
|
What are adverse prognostic factors for follicular lymphoma?
|
- age > 60
- Hb < 12 - increased # of involved lymph nodes - increased disease stage - elevated LDH |
|
|
How is CLL characterized?
|
abnormal accumulation of morphologically mature-appearing lymphocytes with a characteristic immunophenotype (CD5+, CD20+, CD23+)
|
|
|
What is a major cause of death in patients with CLL?
|
hemorrhage & infection (due to pancytopenia)
|
|
|
Which CLL mutation portends a more indolent course?
|
somatic mutations of the immunoglobulin heavy-chain
|
|
|
What disease is associated with a monoclonal serum paraprotein of immunoglobulin M?
|
lymphoplasmacytic lymphoma (Waldenstrom's macroglobulinemia)
|
|
|
What disease is characterized by splenomegaly, varying degrees of leukopenia or pancytopenia and bone marrow infiltration by atypical lymphoid cells with cytoplasmic projections>
|
Hairy cell leukemia
|
|
|
What treatment causes prolonged remission with hairy cell leukemia?
|
pentostatin or cladribine
|
|
|
Of the two types of testicular cancer (seminoma and nonseminoma), which is more radiosensitive?
|
seminoma
|
|
|
Where do nonseminomas metastasize?
|
retroperotineal lymph nodes and lung parenchyma
|
|
|
In which tumor type is AFP elevated, seminoma or nonseminoma?
|
nonseminomatous tumors (if elevated in seminomatous, should treat as nonseminomatous)
|
|
|
What is a potential adverse event to retroperitoneal dissection for testicular ca?
|
retrograde ejaculation
|
|
|
What is a side effect of cisplatin therapy?
|
peripheral neuropathy and subclinical nephropathy
|
|
|
What is a side effect of etoposide-containing treatments?
|
acute nonlymphoblastic leukemia (with chromosomal 11q23 translocation)
|

