![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
What form of heme molecule is found in hemoglobin and myoglobin?
|
Heme b
|
|
|
What molecule contains the iron that binds to the oxygen in oxygen transport storage proteins?
|
heme b
|
|
|
Where is heme C found?
|
In cytochrome C
|
|
|
Where is cytochrome C found?
|
It is an important molecule in the ETC and in the mitochondria, as well as apoptosis.
|
|
|
Where does the majority of heme synthesis take place?
|
In erythroid cells
|
|
|
What form of heme is found in the majority of your body?
|
heme b
|
|
|
Where does the majority of heme synthesis take place besides in the erythroid cells?
|
In the liver
|
|
|
Where does most of the heme synthesized by the liver end up?
|
In the cytochrome p450 superfamily of monooxygenases.
|
|
|
What does cytochrome p450 do?
|
Degrades different classes of molecules and plays a role in the degradation of drugs/pharmacoagents
|
|
|
What amino acid contributes all of its carbons and nitrogens to heme?
|
Glycine
|
|
|
What molecule only contributes carbons to the heme backbone?
|
Acetate
|
|
|
What molecule contributes all of its molecules to the functional component of heme?
|
Glycine
|
|
|
What is the difference b/e porphyrins and heme?
|
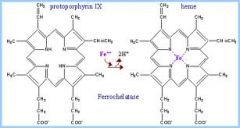
The presence of iron, porphyrin do not have iron. SO if you took a porphyrin and added Fe then you created heme.
|
|
|
What forms the coordination sites for the Fe atom in heme?
|
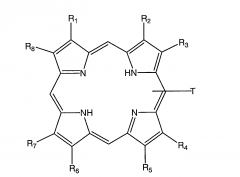
The four pyrrole rings w/ their nitrogen. The four nitrogens point towards the middle to form the coordination sites for Fe.
|
|
|
What determines the different versions of heme? (heme b, heme c, etcetera)
|
The different substituents off of the pyrrole rings in the larger porphyrin ring.
|
|
|
What class of diseases are caused by defects in heme synthesis?
|
Porphyrias
|
|
|
What molecule is the result of heme degradation?
|
bilirubin.
|
|
|
What disease is caused by the accumulation of bilirubin in peripheral tissues?
|
jaundice
|
|
|
What are the two starting substrates in heme synthesis?
|
Acetate and Glycine
|
|
|
What molecule can be used to make succinyl CoA?
|
Acetyl CoA
|
|
|
Where in the cell does the first reaction in heme synthesis take place?
|
In the mitochondrial matrix
|
|
|
Where in the cell does the majority of heme synthesis take place?
|
In the cytosol.
|
|
|
What reaction forms the pyrrole rings of porphyrin?
|
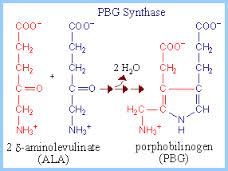
The second reaction where 8 Aminolevulinate (ALA)goes to 4 porphobilinogen (BPG)
|
|
|
Where in the cell does the final part of heme synthesis take place?
|
In the mitochondrial intermembrane space
|
|
|
What is another name for heme?
|
protoporphyrin IX
|
|
|
What is the last step in heme synthesis?
|
Addition of Fe
|
|
|
What regulates heme synthesis in hepatocytes?
|
heme, it functions in a negative feedback loop.
|
|
|
Where is the transporter for heme located?
|
In the outer-mitochondrial membrane, even though this membrane is porous heme is just too big and too polar to go through.
|
|
|
What cells in the body need to transport heme OUT of their cytosols?
|
Hepatocytes
|
|
|
What cells in the body need to transport heme INTO their cytosol?
|
Cells that are not capable of heme synthesis, but that still require heme in their mitochondria.
|
|
|
Where in the cell does heme really like to be? why do we care?
|
It likes to sit in the membranes when it is not bound to a protein, this is important b/c it has an Fe bound to it and it can damage proteins and generate ROS. So free heme can really damage membranes.
|
|
|
What cells is the ALAS1 gene expressed in?
|
Constitutively expressed in all cells
|
|
|
What cells constitutively express ALAS2?
|
Erythroid cells
|
|
|
What heme synthesis enzyme is embedded in the innermitochondrial membrane?
|
ALA synthase so the catalytic portion is located in the mitochondrial matrix, but it has an outer portion in the intermembrane space that heme can bind to and inhibit.
|
|
|
What effect do insulin or glucose have on heme synthesis?
|
They inhibit peroxisome proliferator-activated receptor 1 (PGC-1) which is an activator of ALAS-1.
|
|
|
What effect do glucagon or fasting have on heme synthesis?
|
They activate PGC-1 alpha transcription factor which activates ALAS1
|
|
|
What effect does lead have on heme synthesis?
|
"Lead Poisoning" inhibits the last step of heme synthesis (where Fe is added)as well as the second step (where the pyrrole rings are formed)
|
|
|
What is one of the consequences of Lead Poisoning?
|
Porphyrias b/c it inhibits lead synthesis.
|
|
|
What are the major clinical manifestations of acute porphyrias?
|
Neurologic effects
|
|
|
What are the major clinical manifestations of cutaneous porphyrias?
|
Photosensitivity
|
|
|
What tissues are the major sources where porphyria intermediate overproduction occurs?
|
1. Hepatic
2. Erythropoietic |
|
|
What clinical symptoms do the majority of the erythroid porphryias have?
|
Cutaneous symptoms
|
|
|
What is the major clinical feature of porphyria cutanea tarda (PCT)?
|
Skin photosensitivity to sunlight exposure resulting in sores/blisters and their urine is discolored to look like wine or tea
|
|
|
What enzyme deficiency causes acute intermittent porphyria?
|
A defect in hydroxymethylbilane synthase
|
|
|
What accumulates in acute intermittent porphryia?
|
Porphobilinogen (PBG) and delta-amino-levulinic acid (ALA)
|
|
|
What is the characteristic sequence of symptomatic events that is seen in acute intermittent porphyria?
|
1. abdominal pain
2. psychiatric symptoms, i.e. hysteria 3. peripheral neuropathy, mainly motor neuropathy. |
|
|
What enzyme deficiency causes erythropoietic protophyria (EPP)?
|
Ferrochelatase deficiency in erythropoietic cells
|
|
|
What accumulates in erythropoietic protophyria?
|
Protoporphyrin leading to cutaneous photosensitivity and hepatobiliary disease
|
|
|
What porphyria can have both cutaneous and hepatic manifestations?
|
Erythropoietic protophyria
|
|
|
Elevated levels of what enzyme signal liver disease?
|
ALT/AST
|
|
|
Where does breakdown of heme to bilirubin take place?
|

In macrophages
|
|
|
Where is heme oxygenase located?
|
Inside macrophages
|
|
|
What does heme oxygenase do?
|
Breaks heme apart into biliverdin using NADPH.
|
|
|
Where in heme degradation is CO produced?
|
In the first step where heme is broken down to biliverdin by heme oxygenase
|
|
|
Where is bilirubin produced?
|
In macrophages
|
|
|
What protein does bilirubin bind to in circulation?
|
Albumin
|
|
|
What happens to bilirubin in the liver?
|
It is conjugated to UDP-glucuronic acid to form bilirubin diglucuronide
|
|
|
What happens to bilirubin diglucuronide?
|
It is secreted into the bile
|
|
|
What is bilirubin diglucuronide turned into if it is secreted in stool?
|
Urobilinogen (which has a brownish color and is largely responsible for the color of stool)
|
|
|
What will Sy will pts have if they have a inability to conjugate bilirubin to UDP-glucuronic acid?
|
They will have stool that is whitish and not brown.
|
|
|
What is ultimately responsible for the color of human waste (both feces and urine)?
|
Heme
|
|
|
What is the direct bilirubin measurement?
|
- The reaction w/o accelerator (alcohol)
- Considered the measure of conjugated bilirubin |
|
|
What is the total bilirubin measurement?
|
Measures the reaction w/ accelerator (alcohol) since bilirubin is hydrophobic and not soluble this solubilizes unconjugated bilirubin so it can measure all bilirubin in the body. Then you subtract the conjugated bilirubin number and you get the amount of unconjugated bilirubin.
|
|
|
What can cause normal, healthy, people to look like they have jaundice?
|
Carrots
|
|
|
What causes hemolytic jaundice?
|
An acute situation causing RBCs to lyse, which causes more bilirubin to be synthesized than the Liver can handle, so the excess bilirubin accumulates in peripheral tissue.
|
|
|
How can Liver dz cause jaundice?
|
They are making normal amounts of bilirubin but the pt simply cannot conjugate it to UDP-glucuronic acid. So again, bilirubin accumulates in peripheral tissues and the pt gets jaundiced.
|
|
|
How can you distinguish b/e Liver jaundice and hemolytic jaundice and mechanical jaundice (caused by Gallstones)?
|
Hemolytic: There will be elevated levels of indirect/unconjugated bilirubin
Liver: There will be elevated levels of direct/conjugated bilirubin and normal levels of indirect/unconjugated bilirubin Gallstone: normal level of unconjugated and high levels of conjugated |
|
|
What enzyme is low in newborns and can cause neonatal jaundice?
|
UDP-glucuronyl transferase
|
|
|
What is newborn phototherapy?
|
The photons can modify bilirubin to form structural isomers that are more soluble or favor the oxidation of bilirubin.
|

