![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Associated findings in patients with dermatopathic lymphadenopathy include all of the following EXCEPT:
a. Peripheral blood eosinophilia b. Hyperplasia of Langerhans and dendritic cells c. Pruritus d. Oligoclonal B-cell proliferation e. Histiocytes laden with melanin pigment |
d. Dermatopathic lymphadenopathy
is a proliferation of histiocytes in patchy aggregates in the cortical or the peripheral areas of the lymph node. The paracortical areas are also expanded by Langerhans cells and interdigitating dendritic cells. 70% of patients with dermatopathic lymphadenopathy have cutaneous T-cell lymphoma or Sézary syndrome. |
|

|
Mantle cell lymphoma
Its characteristic cytogenetic finding is t(11;14), which places the JH region of the IgH (14q32) gene in proximity to the CCND1 (11q13) gene, resulting in amplification. |
|

|
Small lymphocytic lymphoma/chronic lymphocytic leukemia
The most common chromosomal anomaly is deletion of 13q14 (> half of cases). Other frequent findings are trisomy 12 (15–20%), del(11q), del(14q), and del(17p). |
|

|
Follicular lymphoma
|
|
|
Flow cytometry
As a cell passes through the chamber multiple parameters are obtained: size |
(forward light scatter - FLS)
|
|
|
Flow cytometry
As a cell passes through the chamber multiple parameters are obtained: complexity/cytoplasmic granularity |
(90° light scatter or side scatter (SSC)
|
|
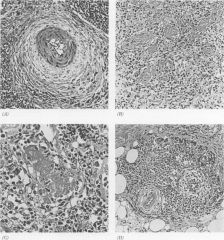
varies from case to case; storiform pattern of spindled fibroblasts or myofibroblasts in fibrous stroma of node with extension into lymphoid tissue and perinodal tissue; also vascular proliferation and mixed inflammatory infiltrate of plasma cells, immunoblasts, small lymphocytes, histiocytes, dendritic cells, neutrophils and fibroblasts
|
Inflammatory pseudotumor in lymph nodes
Positive stains: vimentin, CD45/LCA, CD68, actin; also vascular endothelial growth factor (Int J Surg Pathol 2001;9:207), occasionally EBV Negative stains: ALK, HHV8 |
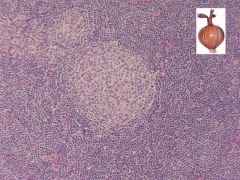
|

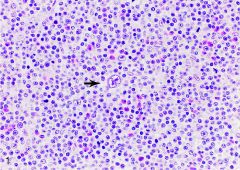
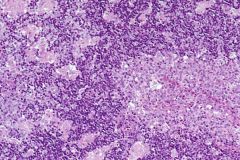
Medium-power photomicrograph showing pseudofollicular growth centers represented by pale staining nodules with prolymphocytes and paraimmunoblasts. Inset, low-power H&E photomicrograph showing indistinct pale nodules (pseudofollicular growth centers) surrounding well-circumscribed reactive follicles
|
Positive stains: CD5, CD19, CD20 (dim), CD23, surface Ig light chain, surface IgM (dim); also CD43, CD79a, CD79b (dim, in 20%), bcl2; variable CD11c, FMC7 (42%)
Negative stains: CD10, cyclin D1 Small lymphocytic lymphoma / Chronic lymphocytic leukemia |
|
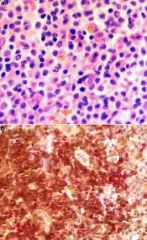
Section of lymph node showing a diagnostic binucleate Reed-Sternberg cell (arrow) with abundant amphophilic cytoplasm and prominent nucleoli in a background of numerous eosinophils, histiocytes, and reactive T lymphocytes (as confirmed by immunohistochemistry and shown in Figure 3 ). Note the frequent prolymphocytes with large vesicular nuclei and prominent central nucleoli (hematoxylin-eosin, original magnification ×400)
|
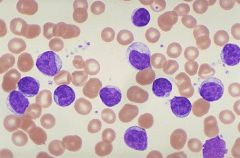
CLL/prolymphocytic leukemia: 10-55% prolymphocytes
Prolymphocytic leukemia: >55% prolymphocytes Bone marrow involvement is interstitial, not paratrabecular |
|
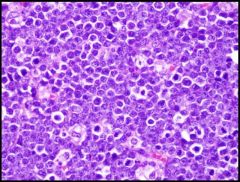
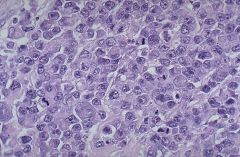
diffuse infiltration of monomorphic, medium-sized (10-25 micron) cells with abundant basophilic cytoplasm, non-cleaved round nuclei with coarse chromatin and 2-5 distinct nucleoli; mitotically active with starry sky pattern (stars are tingible body macrophages)
Imprints demonstrate cytoplasmic lipid vacuoles; rarely granulomas |
Positive stains: CD10, CD19, CD20, Ki-67 (almost 100%), surface immunoglobulin; also CD22, CD79a, bcl6, surface IgM; EBV positive in endemic African cases and AIDS cases
Negative stains: CD5, CD23, TdT Burkitt’s lymphoma |
|
|
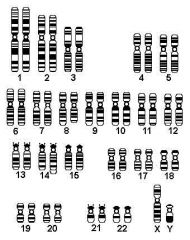
46, XY, t(8;14)
Molecular: c-myc translocations: t(8;14)(q24;q32): c-myc and IgH (75%); also reported in some diffuse large B cell lymphomas t(2;8)(p12;q24): Ig Kappa and c-myc (15%) t(8;22)(q24;q11): c-myc and Ig Lambda (10%) |
|
Molecular: IgH and IgL are clonally rearranged, but may be difficult to document in T cell rich cases
t(14;18)(q32;q21): IgH and bcl2 in 30%, also in follicular lymphoma t(3;14)(p27;q32): bcl6 and IgH in 30%, also in follicular lymphoma Numerous other translocations involving bcl6 (3q27) |
Diffuse large B cell lymphoma
|
|

Positive stains: CD19, CD20, CD22, DBA.44, CD79a, PAX5, TRAP (tartrate resistant acid phosphatase); also CD11c, CD25, CD103, HC2, FMC7; reticulin shows thickened fibers that may circle individual cells and infiltrate normal appearing areas; TIA1 in 56% (Mod Path 2004;17:840); flow cytometry with CD11c, CD20, CD25 and CD103 is useful (Archives 2007;131:383);
Combined TRAP and DBA44 is sensitive but not specific (AJSP 2005;29:474); variable staining for cyclin D1/bcl1 (Mod Path 2000;13:1308); atypical immunophenotyping in 34% (AJCP 2006;125:251), Negative stains: CD79b, CD5, CD23, CD10 |
Hairy cell leukemia
|
|
|
clinical syndrome defined by serum IgM monoclonal gammopathy, monoclonal Ig light chains (Bence-Jones protein) in urine, hyperviscosity syndrome and B cell neoplasm involving marrow, including lymphoplasmacytic lymphoma, B-cell CLL/SLL, marginal zone B cell lymphoma (MALT type), myeloma
|
Waldenström's macroglobulinemia
|
|
|
Diagnostic criteria for Waldenström's recommended by Second International Workshop:
|
IgM monoclonal gammopathy of any concentration
|
|
|
Diagnostic criteria for Waldenström's recommended by Second International Workshop:
|
Bone marrow infiltration by small lymphocytes showing plasmacytoid or plasma cell differentiation
|
|
|
Diagnostic criteria for Waldenström's recommended by Second International Workshop:
|
ntertrabecular pattern of bone marrow infiltration
|
|
|
Diagnostic criteria for Waldenström's recommended by Second International Workshop:
|
Immunophenotype is surface IgM+, CD19+, CD20+, CD22+, CD25+, CD27+, FMC7+, CD5 variable, CD10-, CD23-, CD103-, CD108-
|
|
|
Hyperviscosity syndrome:
|
due to IgM’s large size and number; symptoms are visual impairment (distended and tortuous retinal veins with hemorrhage and exudates), neurologic symptoms due to sluggish blood flow, bleeding due to IgM binding of clotting factors and cryoglobulinemia causing Raynaud’s phenomena and cold urticaria
|
|
(a) Representative field of the neoplasm showing small lymphoma cells. Note the Dutcher bodies in the field (hematoxylin-eosin). (b) Double staining for BCL-10 and CD20 demonstrates nuclear and cytoplasmic BCL-10 expression restricted to the neoplastic cells that are highlighted by the CD20 membranous stain.
|
Lymphoplasmacytic lymphoma/Waldenström macroglobulinemia (LPL/WM) diffusely involving BM
|
|
|
Positive stains: CD19, CD79a, surface and cytoplasmic immunoglobulin (IgM, IgD); also variable CD20, CD22, CD38, variable CD43, strong cytoplasmic immunoglobulin in plasma cell component (monoclonal kappa or lambda, not both)
Negative stains: CD5 (usually), CD10, CD23, bcl2 |
Lymphoplasmacytic lymphoma
|
|
|
Positive stains: CD5, CD19 (strong), CD20 (strong), cyclin D1/bcl1 (variable nuclear staining since cells are at different stages of cell cycle); also CD22, CD43, CD79a, FMC7, surface IgM or IgD, kappa or lambda, bcl2
In-situ hybridization for bcl-1 is more sensitive/specific than immunostains (Mod Path 2001; 14:62) Negative stains: CD23, usually CD10; also bcl6, CD11c, TdT, T cell antigens; usually p27(kip1) negative [B-CLL, follicular and marginal zone lymphomas are p27 positive, hairy cell leukemia is p27 weak/negative, |
Mantle cell lymphoma
|
|
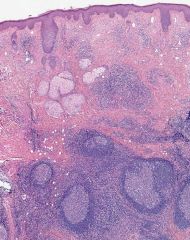
germinal center hyperplasia with polykaryocytes, fibrosis and proteinaceous material in germinal centers; also folliculolysis, interfollicular eosinophils and eosinophilic abscesses; increased paracortical plasma cells; variable hyalinized vessels
Soft tissue lesions show proliferation of thin-walled vessels with eosinophilia Chronic inflammatory disorder of unknown etiology Endemic in Asia, affects young men |
Kimura’s disease in lymph nodes
|
|
angiofollicular hyperplasia
Multicentric disease is almost always plasma cell variant with generalized lymphadenopathy and possible splenic involvement |
hyaline vascular (angiofollicular) variant - common (90%); prominent follicles within lymphoid tissue and no sinusesplasma cell variant - follicular hyperplasia with large germinal centers; diffuse plasma cells between follicles, often with Russell bodies
Castleman’s disease in lymph nodes |
|
Small, iregular-shaped epithellioid granulomas are distributed in the paracortex. Along the sinus, features of monocytoid B-cell hyperplasia are observed (HE)
|
Toxoplasma gondii
|
|
Canale-Smith syndrome
Inherited disorder due to defects in Fas/CD95/Apo-1 mediated apoptosis Childhood onset of lymphadenopathy, hepatosplenomegaly, hypergammaglobulinemia and autoimmunity; also cytopenias and increased risk of lymphoma |
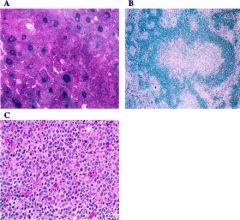
A: The paracortex is markedly expanded by lymphocytes with pale pink cytoplasm. Primary and secondary follicles are numerous. Some follicles show regressive changes (upper right ). H&E; original magnification, x100. B: Progressive transformation of germinal centers was a focal but relatively frequent finding. H&E; original magnification, x200. C: The paracortex is populated by lymphocytes, plasma cells, and immunoblasts. Note frequent mitotic figures. H&E; original magnification, x600.
Autoimmune lymphoproliferative syndrome in lymph nodes |
|
IMMUNOPHENOTYPE
•dim CD20, CD22, CD79b and SmIg •coexpress CD5 and CD23 •CD11c -- variant morphology/trisomy 12 GENETICS •karyotypic/molecular: - 17p13 (p53) and 11q22-23 (ATM): bad prognosis - 13q14: good prognosis (commonest) •IgH gene mutations: - absent/preGC: bad prognosis (ZAP70+/CD38+) - present/post GC: good prognosis (ZAP70-/CD38-) |
SMALL LYMPHOCYTIC LYMPHOMA
|
|
|
PML-RARα fusion transcript characteristically results in:
a. Undifferentiated leukemic cells without Auer rods b. Inv16(p13q22) translocation c. Chronic leukemia with prominent eosinophils d. Blast phase of chronic myelogenous leukemia e. Leukemia with marked coagulopathy |
e.This fusion transcript results in translocation t(5;17)(q22;q11-12), which is a feature of
acute promyelocytic leukemia |
|
|
Activation of the fusion gene AML1/ETO results in:
a. t(9;11)(p21;q23) translocation b. Acute lymphoblastic leukemia c. Leukemic cells with Auer rods d. Leukemia with biphenotypic profile e. All of the above |
c.This translocation is one of the most common chromosomal aberrations in
acute myeloid leukemia and occurs predominantly in younger patients. Leukemic cells have myeloid differentiation and show cytoplasmic Auer rods. This type of leukemia has good prognosis and good response to chemotherapy. |
|
|
Of the following histologic types of Hodgkin lymphoma, which one has the WORST prognosis?
a. Nodular sclerosis classical Hodgkin lymphoma b. Mixed cellularity c. Lymphocyte-depleted type d. Lymphocyte-rich e. Lymphocyte-predominant type |
c.The prognosis of Hodgkin lymphoma
is best in nodular sclerosis type, followed by mixed cellularity. The overall 5-year survival rate for Hodgkin lymphoma is 75%, and is worst in lymphocyte-depleted type. |

