![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
106 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the 4 categories of leukemia?
|
AML- Acute Myeloid L
ALL- Acute Lymphoblastic L CML- Chrocic myelosytic L CLL- Chronic Lymphocytic L |
|
|
|
In this leukemia, the spleen becomes the site of extra medullary hematopoeisis.
|
AML
|
|
|
|
Peripheral blood of this leukemia contains:
Blasts Auer rods, giant platelets nRBCs and Hypersegmented Segs |
AML
|
|
|
|
To diagnose this Leukemia you need:
-200 WBC count -Observable Hypercellular BM - 20% or > myeloblasts |
AML
|
|
|
|
True or False?
There are more blasts present in Chronic Leukemia than Acute Leukemia? |
False
|
|
|
|
This cytochemical stain stains primary granules containing peroxidase and is a good indicator of AML?
|
Myeloperoxidase (MPO)
|
|
|
|
This test differentiates AML from ALL and is a strong positive test for myeloblasts.
|
Myeloperoxidase (MPO)
|
|
|
|
This cytochemical stain:
- stains phospholipids and other lipids found in primary and secondary granules of Myeloid cells. -Negative in Lymphs -Differentiates ALL and AML -Sensitive for granulocyte precursor |
Sudan Black B (SBB)
|
|
|
|
This cytochemical stain:
- stains primary granules of myeloid cells - myeloblasts are strong positive -neutrophils, basophils, mast cells stain pos - eos, monos, and lymphs stain neg |
Specific Esterase (napthol AS-D chloroacetate esterase)
|
|
|
|
This cytochemical stain:
-strong pos for monocytes -negative reation w/ granulocytes -used to ID monoblasts and monocytes in acute myeloblastic anemia |
Nonspecific esterase
|
|
|
|
This cytochemical stain:
-stains an intracellular enzyme found in stem cells and immature T and B cells in BM - indicator of Lymphoblastic leukemias |
Terminal deoxynucleotidyl transferase (TdT)
|
|
|
|
This cytochemical stain:
- stains T lymphoblasts |
Acid phosphatase
|
|
|
|
This cytochemical stain:
- stains B lymphocytes in hairy cell leukemia |
Tartrate resistant acid phosphatase
|
|
|
|
This cytochemical stain:
- Stains glycoproteins and glycogen - ALL exhibits "block staining" |
Periodic Acid-Schiff (PAS)
|
|
|
|
This AML portrays
-Pseudo Chediak Higashi graunles -Pseudo Pelger Huet - Auer Rods -good long term prognosis |
AML w/ t(8;21) (q22;q22)
|
|
|
|
This AML portrays:
-Various stages of Monos, Eos, and other grans - high complete remission rate -NSE strong pos on Monos and Promonos |
AML W/ inv(16)(p13q22)
|
|
|
|
This AML portrays:
- Auer rods - * procoagulant/ fibrinolytic activity leads to DIC * - hypo/hypergranular varients - |
Acute promyelocytic leukemia w/ t(15;17)(q22;q21)
|
|
|
|
This AML portrays:
- mainly in adults - dyplasia in at least 2 cell lines - a myelodysplastic syndrome - a poor prognosis |
AML with Myelodysplasia
|
|
|
|
This AML M1 (not otherwise categorized) portrays:
- marrow replaced with blasts - CD 13, 33, 117 - MPO and SBB neg - No Auer rods - 5% of AML cases |
AML minimally differentiated
|
|
|
|
This AML (not otherwise categorized) portrays:
- similar to minimally diff. AML except that at least 5% of blasts are MPO and SBB pos. - Auer rods me also be present. - 10% of AML cases |
AML without maturation
|
|
|
|
This AML (not otherwise categorized) portrays:
- 30-45% of all AML cases - as in all AMLs, 20% if BM cells are blasts, but also > 10% of segs are beyond the pro stage - monocytic component is <20% of nonerythroid cells - 50% of blasts are MPO and SBB pos - Auer rods and blasts occur frequently |
AML with maturation
|
|
|
|
This AML (not otherwise categorized) portrays:
- a mixture of malignant cells w/ both myelocytic and monocytic features - contains monoblasts - NSE strong pos - Specific esterase is also pos - monoblasts are MPO and SBB neg |
Acute Myelomonocytic leukemia
|
|
|
|
This AML (not otherwise categorized) portrays:
- > 20% of BM cells are blasts w/ >80% of monocytic origin - monoblasts are predominant but also promonocytes and monocytes |
Acute Monoblastic and Acute Monocytic leukemia
|
|
|
|
True or False?
Acute monocytic leukemia is more common in adults, and Acute monoblastic leukemia is more common in kids. |
True
|
|
|
|
The hallmark feature for this AML is Extramedullary dz charasterized by :
- Gum infiltration - CNS dz - a poor prognosis |
Acute Monocytic/blastic leukemia
|
|
|
|
This AML (not otherwise categorized) portrays:
- usually affects Pts 50 years old or older - more than 50% of BM cells are erythroid precursors and 30% are monoblsts. |
Erythroleukemia
|
|
|
|
This AML (not otherwise categorized) portrays:
- usually affects Pts 50 years old or older - >80% of BM cells are erythroid precursors - Iron stain shows ringed sideroblasts - Myeloblasts are MPO and SBB pos - PSA stain shows "block" pattern in promonoblasts |
Pure erythroid leukemia
|
|
|
|
The affects of this AML are:
- ineffective erythropoiesis - high NRBC count in peripheral blood |
Acute Erythroid Leukemia
|
|
|
|
This AML (not otherwise categorized) portrays:
- rarest form of AML - occurs in children and adults - megakaryoblasts - diagnosis based on immunophenotyping |
Acute megakaryoblastic Leukemia
|
|
|
|
This acute leukemia is characterized by:
- rare occurrence - pancytopenia - BM hyperplasia - splenomegaly usually absent - * BM is so packed, marrow tap results a "dry tap" |
Acute Myelofibrosis
|
|
|
|
This Leukemia is:
- * Predominantly in children * - a mutation of lymphoid precursor cells |
Acute Lymphoblastic Leukemia
|
|
|
|
True or False?
L2 class ALL is more likely to occur in children and L1 class ALL is more likely to occur in adults. |
False
|
|
|
|
In this Leukemia:
- B-lineage lymphoblasts are predominant in BM - cells are uniformly TdT pos, HLA-DR pos, and CD10 pos |
Precursor B Leukemia
|
|
|
|
In this leukemia:
- T-lineage lymphoblasts are predominant in BM - TdT pos - CD 3 and 7 |
Precursor T Leukemia
|
|
|
|
What are the 4 Chronic Myeloproliferative Disorders (CMPDs)?
|
1. Chronic myelogenous leukemia (CML)
2. Myelofibrosis with myeloid metaplasia (MMM) 3. Polycythemia Vera (PV) 4. Essential thrombocythemia (ET) |
|
|
|
True or False?
Leukocyte alkaline phosphatase (LAP) can be high in all CMPDs except CML. |
True
|
|
|
|
This CMPD:
- 90-95% of Pts have Philadelphia chromosome 9:22 translocation (Ph1) - results in coding for p210, which increases tyrosine kinase activity, leading to suppressed apoptosis, excess cell production |
Chronic Myelogenous Leukemia
|
|
|
|
True or False?
One characteristic of CML is that it is a normocytic, normochromic anemia. |
True
|
|
|
|
Diagnosis of this CMPD consists of FISH test to detect BCR/ABL, or cytogenetics for Ph1 chromosome.
|
CML
|
|
|
|
Treatment of this CMPD includes:
- myelosupressive therapy - leukaphoresis - Tyrosine kinase inhibitor |
CML
|
|
|
|
How do you tell the difference between a leukamoid reaction and CML?
|
- Leukamoid does not contain PH1
- Eos and Basos are increased in CML, but not leukamoid - LAP is decreased in CML but increased in leukamoid |
|
|
|
This CMPD:
- usually occurs in ages 60-70 - BM is hypercellular w/ hyperplasia - clonal disorder with over-production of RBCs, WBCs, and platelets - *RBCs are much more sensitive to EPO than usual - increased blood viscosity - * 90% have JAK 2 mutation * |
Polycythemia Vera (PV)
|
|
|
|
In this CMPD:
- The most significant findings are increased RCM, splenomegaly, and JAK 2. |
PV
|
|
|
|
The major cause of death in untreated Pts with this CMPD is hemorrhage and thrmbosis.
|
PV
|
|
|
|
This rare CMPD:
- is characterized by marked thrombosytosis and abnormal platelet function. - increased PLT production due to hypersensitive megakaryocytes cytokines and TPO |
Essential Thrombocythemia (ET)
|
|
|
|
Characteristics of this rare CMPD include:
- Hgb count no higher than 13 g/dL - absence of BM fibrosis (no tear cells) - presence of stainable iron in BM |
ET
|
|
|
|
Thrombosis in microvasculature resulting in erythromelagia of extremities is indication of.......
|
ET
|
|
|
|
Factors that cause "reactive" type of this CMPD include:
- acute hemorrhage - post splenectomy - post operative - inflammation - hemolytic anemia |
ET
|
|
|
|
The goal of treatment for this CMPD is to prevent vaso-occlusion and hemorrhage. Usually by prescribing aspirin, platelet phoresis, myelosuppressive drugs.
|
ET
|
|
|
|
PLT is >600 x 10^9/L in this CMPD.
|
ET
|
|
|
|
Platelet count needs to be under what value to successfully prevent the effects of ET?
|
< 400 x 10^9/L PLT
|
|
|
|
This CMPD:
- is characterized by BM fibrosis, proliferation of megakaryocytes and granulocytes, and EM hematopoiesis - normal hematopoiesis is blocked as BM becomes more * fibrotic * - results in EM hematopoiesis and splenomegaly |
Myelofibrosis with Myeloid Metaplasia
|
|
|
|
Many tear drop RBCs can be observed in this CMPD. (They are due to splenic and BM fibrosis). Dwarf megakaryocytes, and giant platelets are also observed.
|
Myelofibrosis with Myeloid Metaplasia
|
|
|
|
In this CMPD,
- Hgb < 10mg/dL - MB draw usually results in a dry tap |
MMM
|
|
|
|
Treatment of this CMPD is hydroxyurea to control:
- leukocytosis - thrombocytosis - organomegaly |
MMM
|
|
|
|
True or False?
Lymphoma originates in the BM and is noted in the general circulation |
False, Lymphoma originates in the lymphatic system.
|
|
|
|
True or False?
Leukemia originates in the lymphatic tissue. |
False, Leukemia originates in the BM.
|
|
|
|
What are the 7 Lymphoproliferative Disorders (LPDs)?
|
- Chronic Lymphocytic Leukemia (CLL)
- Hairy Cell Leukemia - Sezary Syndrome - Prolymphocytic Leukemia - Hodgkin's/ Non-Hodgkin's Lymphoma - Multiple Myeloma - Waldenstrom's Macroglobulinemia |
|
|
|
This LPD is caused by a clonal proliferation of B cells and exhibits exclusively small lymphocytes and smudge cells on a smear and a WBC count >100,000 x 10^9/L
|
Chronic Lymphoproliferative Leukemia
|
|
|
|
This LPD is characterized by fragile mononuclear cells with hair-like projections of the cytoplasm and are diagnostic with the TRAP test. (CD 19, 20, 22, 11c, 25, 103)
|
Hairy Cell Leukemia
|
|
|
|
Symptoms of this LPD include a abdominal pain ( indicative of a massive spleen), Thrombocytopenia, Pancytopenia, and dry tap and treated by therapeutic splenectomy.
|
Hairy Cell Leukemia
|
|
|
|
This LPD is considered the leukemic phase of cutaneous T cell lymphoma.
|
Sezary cells
|
|
|
|
Sezary cells are pathognomonic of what lymphoma?
|
Cutaneous T cell Lymphoma
|
|
|
|
This rare LPD is a variant of CLL and has a majority of circulating prolymphocytes. Also has a strong CD 20 and Sig activity.
|
Prolymphocytic Leukemia
|
|
|
|
This LPD is the most common lymphoma in young males and also seen in people over 50.
|
Hodgkin's Lyphoma
|
|
|
|
The presence of large, multi-nucleated cells that resemble and owls eye are called ___________ cells and are indicative of ______________?
|
Reed-Sternberg cells
Hodgkin's Lymphoma |
|
|
|
This LPD is 3x more common than Hodgkin's Lymphoma and may present as painless cervical lymphnode involvement.
|
Non-Hodgkin's Lymphoma
|
|
|
|
This LPD is a disorder of the plasma cells, and causes a spike in the gamma region on a EP test.
|
Multiple Myeloma (MM)
|
|
|
|
In this LPD plasma cells are accelerated by cytokine IL-6 and contain colorless inclusions called Russell bodies or other crystalline inclusions.
|
Multiple Myeloma (MM)
|
|
|
|
Flame cells are present in the IgA version of this LPD.
|
Multiple Myeloma
|
|
|
|
In this LPD serum calcium levels are elevated due to increased osteoclast activity (bone break down) and may lead to kidney failure/ stones.
|
Multiple Myeloma
|
|
|
|
Monoclonal gammopathy, serum free light chains, Rouleaux formation, increased ESR, and Bence-Jones Proteins are all signs of which LPD?
|
Multiple Myeloma
|
|
|
|
What is the treatment for Multiple Myeloma?
|
Chemo/ radiation
Thalidomide |
|
|
|
What complication of Multiple Myeloma occurs in late Dz state and is characterized by increased plasma cells in circulating blood?
|
Plasma Cell Leukemia
|
|
|
|
This LPD is characterized by an overproduction of IgM from abnormal B cells.
|
Waldenstrom's Macroglobulinemia
|
|
|
|
True or False:
In Waldenstrom's Macroglobulinemia, IgM interferes with platelets by causing a platelet satallitism. |
False, The IgM impedes PLT function by coating the platelets.
|
|
|
|
Hyperviscosity syndrome, or the slow flow of blood that causes CNS symptoms, is an indicator of of which LPD?
|
Waldenstrom's Macroglobulinemia
|
|
|
|
Cryoglobulins may be found in which LPD, and lead to what phenomenon characterized by cold hands and feet?
|
Waldenstrom's Macroglobulinemia
Raynaud's Phenomenon |
|
|
|
This Glycoprotein is made in the liver to transport iron in the serum.
|
Transferrin
|
|
|
|
This iron is the storage form of iron in the body, found mostly in the RES.
|
Ferritin
|
|
|
|
What are the 3 broken-down components of Hemoglobin?
|
-Globin
- Iron - Protoporphyrin |
|
|
|
What are the 3 routes that lead to Anemia?
|
1. Dec. production of RBC or Hgb
2. Inc. destruction of RBC or Hgb 3. Loss of RBCs |
|
|
|
True or False?
1/3 of iron in the body is found in Hgb and the other 2/3 is "tissue iron". |
False, 2/3 is in Hgb and 1/3 is "tissue iron".
|
|
|
|
What is hemosiderin?
|
It is precipitated ferritin found primarily in the liver. Can be seen with heatoxylin-Eosin or Prussian Blue stain.
|
|
|
|
True or False?
100% of iron from RBCs is recycled. |
True
|
|
|
|
Describe how dietary iron gets converted to ferritin in the body.
|
1. Ingested as Fe3+,
2. converted to Fe2+ by stomach acid 3. Fe2+ absorbed in duodenum and oxidized back to Fe3+. 4. Fe3+ combines with apoferritin to for ferritin |
|
|
|
What are the three stages of iron deficiency?
|
1. Depletion of iron stores.
2. Iron-deficient erythropoiesis 3. Iron-deficiency anemia |
|
|
|
What are some causes of Iron deficiency anemia?
|
- nutritional deficiency
- gastrointestinal bleeding - other kinds of hemorrhage - menorrhagia -hemolysis |
|
|

This phenomenon, known as Koilonychia, is a common symptom of what microcytic anemia?
|
Iron deficiency anemia (IDA)
|
|
|
|
Delta aminolevulinic acid + EPO + vit. B6 lead to the production of what?
|
Protoporphyrin
|
|
|
|
In inherited sideroblastic anemia, because Pts are aminolevulinic synthetase deficient, they cannot create what important element of RBCs?
|
Protoporphyrin
|
|
|
|
What is the word for a clinical disorder that results in tissue damage from excess iron?
|
Hemachromatosis
|
|
|
|
True or False?
Gene mutations are the reason for the chromosomal abnormalities of Alpha Thalassemia. |
False, gene deletions are the cause.
|
|
|
|
What subclass of Alpha Thalassemia has no alpha globin chains present?
|
Barts hydrops fetalis
|
|
|
|
Why is Beta Thalassemia not recognizable in an infant until they are older?
|
B/c the absent beta chains do not affect Hgb F, which is the predominant Hgb for infants. It is only when the Hgb F levels decrease and the Hgb A levels increase that you would observe affects.
|
|
|
|
Describe the concept of the osmotic fragility test.
|
RBCs in thalassemia have a decreased osmotic fragility because of the lack a certain globin chain. When normal RBCs are put in a hypotonic solution, fluid follows the concentration gradient into the RBC to the point of cell lysis. Because cells in thalassemia have more cell surface area, they lyse at a much more hypotonic solution than normal RBCs.
|
|
|
|
True or False?
Hgb H dz has 2 functional alpha chains. |
False, Hgb H only has 1 functional alpha chain.
|
|
|
|
True or False?
Beta Thal it a homozygous disorder? |
True
|
|
|
|
True or False?
The reason for the genetic abnormalities in Beta Thal are from gene mutations. |
True
|
|
|
|
In what microcytic anemia do Pts compensate by producing 60-95% of Hgb F
|
Beta Thalassemia
|
|
|
|
What is the risk factor for transfusion in a Pt with Beta Thal?
|
It could lead to iron overload.
|
|
|
|
True or False?
Hgb levels are very high in Beta Thal? |
False, Hgb levels are around 6-9 g/dL
|
|
|
|
What test is used to screen for Hgb F?
|
Acid Elution Test (Kleihauer and Betke stain), Hgb F picks up Eosin stain and is observed.
|
|
|
|
What dz is the acid elusion test used to identify?
|
Hereditary Persistence of Fetal Hgb (HPFH),
|
|
|
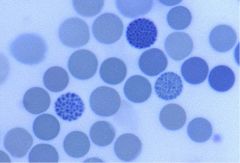
What microcytic anemia is characteristic of these "golf ball" cells?
|
Hgb H syndrome (1 functional alpha chain)
|
|
|
|
Which hemoglobins are fetal?
|
1. Hgb Gower I
2. Hgb Gower II 3. Hgb Portland |
there are 3 of them.
|

